AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2692-9562/131
1Department of Oncology and Robotic Surgery, Unit of Audiology, Oncological and Robotic Head and Neck Surgery, Careggi University Hospital, Florence, Italy.
2Pathology Unit, Local Hospital ASLAL, Ospedale san Giacomo Novi Ligure, Italy; 3Department of Health Sciences, University of Eastern Piedmont "Amedeo Avogadro", Italy.
4Department of Neuroscience, Reproductive Science and Dentistry, Section of Audiology, University of Naples ‘’Federico II’’, Napoli, Italy
5Unit of Histopathology and Molecular Diagnostics, Careggi University Hospital, Florence, Italy.
6Department of Neuroscience, Psychology, Drug’s Area and Child’s Health, University of Florence, Florence, Italy.
* These authors have equally contributed to the present work.
*Corresponding Author: Federica Pollastri, Unit of Audiology, Oncological and Robotic Head and Neck Surgery, Careggi University Hospital, Largo Brambilla 3, 50134 Florence, Italy.
Citation: Federica Pollastri, Cecilia Taverna, Vincenzo Marcelli, Annarita Palomba, Rudi Pecci, et al, (2024), Intrusive Schwannoma Associated with Capillary Lobular Hemangioma of The Ear: A Clinical, Radiological and Histopathological Challenge, Journal of Clinical Otorhinolaryngology, 6(6); DOI:10.31579/2692-9562/131
Copyright: © 2024, Federica Pollastri. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 22 August 2024 | Accepted: 02 September 2024 | Published: 29 November 2024
Keywords: lobular capillary hemangioma; vestibular schwannoma; schwannoma of external auditory canal
Schwannomas are benign nerve sheath tumors originating from Schwann cells. They are frequently found in the head and neck region, involving above all, the vestibular nerve in its course within the internal auditory canal. In this region, they are usually small and slow-growing masses. Sometimes they can invade adjacent structures at the cerebellopontine angle, but their extension towards the middle and external ear is extremely rare. Moreover, vestibular schwannomas are unlikely to occur associated with other lesions, such as hemangiomas.
Herein, we describe an extremely rare case of a giant vestibular schwannoma with a high growth rate, invasion of middle and outer ear structures, and bone erosion. The lesion was associated with a hemangiomatous reaction diagnosed as a lobular capillary hemangioma in the distal part, a unique event.
Schwannomas are benign, slow-growing tumors that arise from differentiated Schwann cells of the peripheral, cranial, or autonomic nerve sheaths in various anatomic sites. They derive from neural crest cells and typically exhibit expansive growth, pushing the neural fibers of the affected nerve laterally and toward the periphery. They are characterized by the presence of a residual capsule of perineurium around the lesion.
Approximately 25-45% of schwannomas arise in head and neck region (scalp, face, middle ear, mastoid, intracranial cavity, orbit, nasal and oral cavities, parapharyngeal spaces, medial and lateral regions of the neck, larynx), with the vestibulo-cochlear nerve being the most common site affected (8% of intracranial tumors, 80% of cerebellopontine angle tumors [1-3]. Vestibular schwannomas usually extend to the cerebellopontine angle due to the absence of bone structures that can contain their growth [4].
Regarding the external auditory canal, schwannomas are very rare and only a few cases have been described in the literature [5, 6]. Some authors describe a lesion with mild extension into the middle ear. In contrast, others observe schwannoma localized only in the outer ear without involving adjacent middle and/or inner ear structures [4, 7-18].
Lobular capillary hemangioma (pyogenic granuloma) represents a rare form of benign vascular lesion, usually found in skin, although it can be found in other anatomical sites, such as mucous membrane and capillaries; it is characterized by small benign vessels arranged in a lobular architecture associated with a myxoid stroma in the background. The lesion is often surrounded by varying degrees of inflammatory cells [19]. Pyogenic granuloma has a controversial etiology, as many factors can induce its growth, such as pregnancy hormone release, chronic mechanical stimulation, trauma or drugs [20,21]. Nearly 62.4% of lobular capillary hemangiomas develop in the head and neck region.
In this region, the most common sites of lobular capillary hemangioma development are the maxillary gum, lips, tongue and buccal mucosa [21, 22]; other sites such as nasopharynx, turbinates, and trachea are extremely rare [23-26]. Only occasionally has it been described in the external auditory canal, with very few cases reported in the literature [27-29]. The majority of them are related to pregnancy, reaction to skin scratching, or other types of trauma; lesions arising ex-novo in the external auditory canal or the concha are exceeding rare [30-32].
Here, we present a unique case of an intrusive vestibular schwannoma of the internal auditory canal and the cerebellopontine angle spreading to the inner, middle and outer ear, associated with a telangiectatic reaction in the distal part, diagnosed as a lobular capillary hemangioma.
In May 2021, a 54-year-old man presented to our clinic with mild left otorrhagia after inserting a cotton swab into the external auditory canal. Based on his medical history, the patient suffered from a progressive left hyperacusis (later resulting in anacusis) that started 15 years earlier, associated with tinnitus, for which he underwent two brain magnetic resonance imaging (MRI) scans in 2008 and 2012 to evaluate retro cochlear involvement, with negative results. He had no history of vertigo or imbalance and no evidence of facial paresis. His medical history included only arterial hypertension and tonsillectomy in childhood. On oto-microscopic and oto-endoscopic evaluation, including narrow-band imaging (NBI) endoscopy, the external auditory canal was wholly occupied by a pink-pale to grayish, hard-elastic, irregular lesion implanted on the anterior wall (Figure 1).
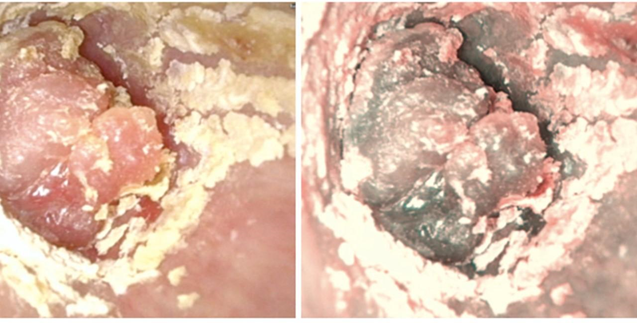
Figure I: on the left otoendoscopic view of the lesion of the external auditory canal, on the right the same lesion using NBI light.
There was no spontaneous or provoked hemorrhage. The tympanic membrane was not evaluable due to the lesion's complete occlusion of the external auditory canal. The patient underwent computed tomography (CT)
of the temporal bone, which revealed a hypodense formation originating from the external auditory canal and involving the bony structures of the middle ear. The lesion obliterated the mastoid cells (Figure II)
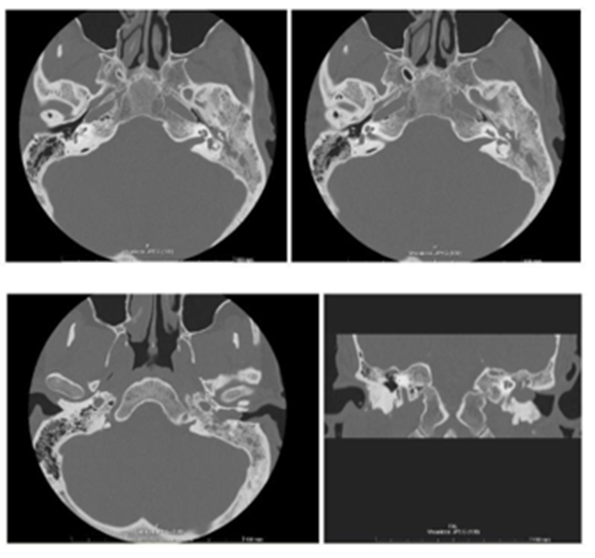
Figure II: petrous bone CT scan in axial and coronal plane shows a hypodense formation in the left external auditory canal and the middle ear, involving the bony structures, as well as an enlargement of the internal auditory canal.
and only an indistinct erosion of the auditory canal and ossicular chain was noted. After instrumental examination, a biopsy of the distal portion of the lesion was performed to determine the lesion's nature and exclude a possible glomus tumor.
Histopathologic examination described a lesion of small vessels arranged in a pseudo-lobular architecture, involving the connective tissue under the squamous epithelium of the external auditory canal. The endothelial cells, which were positive for CD31 and CD34 on immunohistochemistry, were small in size, with benign-looking nuclei, absence of atypia and pleomorphism, as well as architectural worrisome features, as tufting or pseudostratification. Based on the morphologic and immunohistochemical features, lobular capillary hemangioma was diagnosed (Figure III, A).
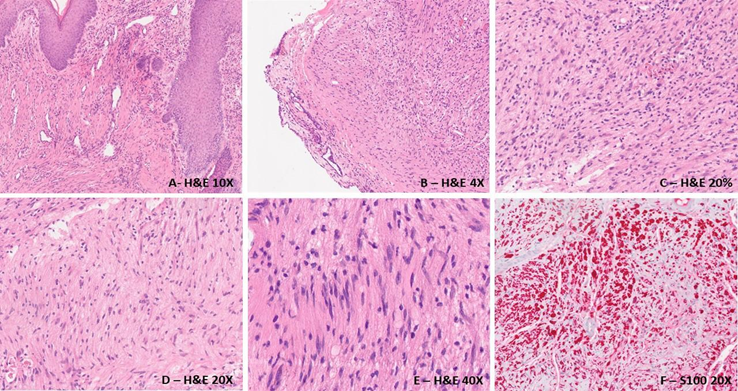
Figure III: A: the peripheral part of the lesion shows a benign vascular proliferation, composed of bland looking, small vessels in the subcutaneous connective tissue, interpreted as lobular capillary haemangioma; B: at low power, a peripheral capsule is present; C-D: schwannoma typically show hypercellular and hypercellular areas; E: in cellular areas, occasional Verocay bodies are seen, insisting in nuclear palisading around fibrillary processes; F: Immunohistochemical stain for S100 highlights the nerve sheath origin of the lesion.
Consequently, MRI of the petrous bone and MR angiography of the intra- and extracranial vessels was performed, which showed the presence of an extra-axial expansive lesion extending from the left internal acoustic meatus into the adjacent cistern, measuring 2.1x1 cm in the axial plane, with a small segment of the internal acoustic meatus free in the deep slope. The lesion
caused the initial compression of the left middle cerebellar peduncle. After contrast infusion, the lesion enhanced the signal, with significant contrast uptaking in the cochlea, vestibule and left lateral semicircular canal, as well as in the hypotympanic cavity to the hypotympanic septum and external auditory canal (Figure IV).
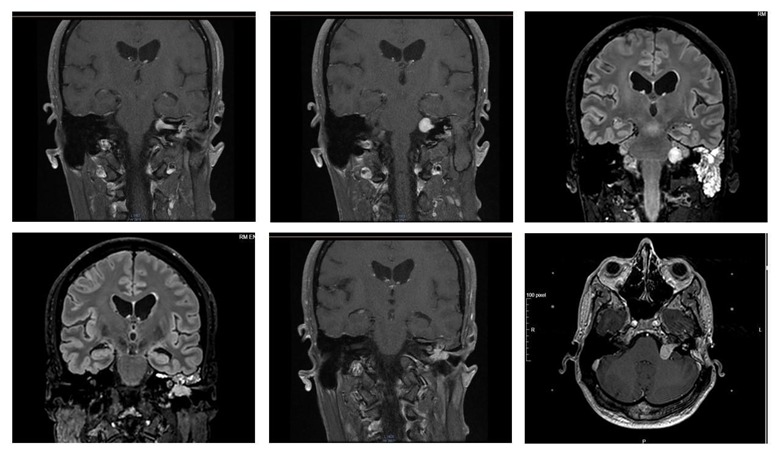
Figure IV: Brain MRI shows an extra-axial expansive lesion extending from the left internal acoustic meatus into the adjacent cistern (diameter in the axial plane 1x2.1 cm). The lesion enhances Gadolinium, with a significant uptake in the cochlea, vestibule, left lateral semicircular canal, hypotympanic cavity, hypotympanic septum and external auditory canal.
The instrumental findings were consistent with a diagnosis of vestibular schwannoma. After multidisciplinary tumor board discussion, a primary surgical approach was chosen. A translabyrinthine exeresis of the lesion was proposed because of the left anacusis, but the patient preferred to avoid it for
possible complications, especially facial paralysis. Consequently, a subtotal petrosectomy was performed to remove the part of the lesion involving the external and middle ear, and Gamma Knife treatment was proposed for the remaining part. During surgery, the external auditory canal, tympanic cavity and antrum were found to be involved in the lesion. The labyrinthine block was also partially covered by the formation and the incus and stapes suprastructure appeared to be eroded. The Falloppian canal was intact and there were no areas of dehiscence. The removed neoformation was sent for histologic evaluation.
A microscopic examination of the specimen revealed a dual component. The majority of the lesion was diagnosed as Schwannoma, being composed of bland-appearing spindle cells arranged in a storiform pattern with palisaded nuclei, with scattered hypercellular (Antoni A) and hypocellular areas, while the characteristic Verocay bodies were found only occasionally. Spindle cells showed rare and occasional mild atypia, while pleomorphism and mitotic activity were absent. In the background, myxoid stroma and occasional medium-sized vessels with thick sclerotic walls were present. In the distal part of the lesion, in the subcutaneous connective tissue underneath the squamous epithelium of the external auditory canal, a residual vascular lesion was found, consisting of thin, randomly arranged vessels without any atypical features. Spindle cells were positive for nerve sheath immunohistochemical markers such as S100 and SOX10, while the vascular cell population stained positive for CD31 and CD34, as the bioptical material previously analyzed. Based on all these features, the final diagnosis was schwannoma with collisional capillary lobular hemangioma (Figure 3, B-F). One year after surgery, the patient began Gamma Knife treatment for the portion of the lesion localized in the cerebellopontine angle.
At the last clinical control, in April 2024, the patient was stable, with no evidence of disease, 12 months after gamma knife treatment and 24 months after surgery.
We report an extremely rare case of a massive schwannoma arising from the cerebellopontine angle with invasion of the inner, middle and outer ear, mixed with a distal capillary proliferation of benign vessels, diagnosed in biopsy material as a lobular capillary hemangioma, leading to a challenging final diagnosis and complex management of the patient. To our knowledge, this is the first report describing this type of lesion [8,9].
The case described herein presents some clinical, radiologic and histopathologic challenges.
The localization of the neoplasm is peculiar; to our knowledge, only 3 cases of vestibular schwannoma reported in the literature initially presented as a middle ear mass. They present with progressive hypoacusis, vertigo and sudden hearing loss. Surgery of these 3 lesions reveal a post-inferior mass involving the round window niche, the stapes crura, the basal turn of the cochlea, the lateral semicircular canal and the facial nerve. The extension into the internal auditory canal and the cerebello-pontine angle led the authors to suggest that these tumors express a primary intracanalicular schwannoma with medial and lateral secondary extension [7, 10]. In one of these three cases, it is suggested that two different lesions might be present, a schwannoma and a neurofibroma. Still, the lack of nerve fibers within the tumor and the absence of any evidence of NF argue against this hypothesis [7].
Furthermore, in none of the other reports is there any invasion of the mastoid cells and no evidence of ossicular chain erosion; in contrast, the lesion we have found involved all middle ear structures and had erosive power toward the ossicles [11-17].
For the clinical and imaging features of the lesion, one hypothesis is the collisional presence of two different schwannomas, one originating from the cerebellopontine angle and the other from the nerve fibers present in the external auditory canal. Since the posterior and inferior parts of the outer ear are innervated by branches of the V, VII, IX and X cranial nerves, the auricular nerve and the occipital nerve (belonging to the components of the cervical plexus C2 and C3), the external part of the tumor may originate from one of these sensory nerves [1117. This theory, however, is afterwards discarded, as complete MRI showed a single, extensive mass; moreover, in the literature none of the cases of external auditory canal schwannoma described are also associated with vestibular schwannoma [11-17].
Because of the suspicion of two different schwannomas, the patient was screened for Von Recklinghausen disease (or neurofibromatosis type 1) and neurofibromatosis type 2, with negative results. Neurofibromatosis type 2 is also excluded because of the unilateral nature of the lesion, the patient's age, the absence of first-degree relatives, and other lesions typical of this genetic pathology [35].
On histologic examination, the lesion presents a dual component, which is extremely rare, especially for the association of schwannoma with lobular capillary hemangioma. Indeed, lobular capillary hemangioma can be found alone in the outer ear, although it is rare, with less than 20 cases reported in the literature so far [27-34]. The age of diagnosis is usually pediatric and tends to resolve spontaneously [36, 37]. Localization is similar to cases reported in the literature, occurring in the posterior part of the external auditory canal and tympanic membrane. The diagnosis is usually incidental as these lesions are typically asymptomatic and are found after bleeding provoked by using foreign bodies such as cotton swabs [38]. These lesions are generally benign, with no evidence of bone erosion or aggressive invasion of adjacent structures. This is in agreement with the case presented here, since the bone remodeling found during surgery is due to the erosive activity of the schwannoma, of which the lobular capillary hemangioma is, in our opinion, only a telangiectatic reaction of its most lateral part. The differential diagnosis must include other spindle cell lesions and vascular proliferations of the ear. For the schwannoma, different entities must be considered based on cellular characteristics and anatomic location of the lesion. Among spindle cell lesions, various types of nerve sheath tumors must be considered, such as neuroma, neurofibroma, and malignant peripheral nerve sheath tumor (MPNST); muscle cell proliferations, such as leiomyoma and leiomyosarcoma; melanoma, especially the desmoid subtype; and carcinomatous meningitis.
Immunohistochemistry can be useful in distinguishing nerve sheath tumors from entities of other origin. Spindle cell lesions of smooth muscle express myoid markers such as desmin and smooth muscle actin, and melanoma cells stain positive for HMB45 and MART1 but share expression of S100 with schwannomas. Therefore, a complete panel is mandatory, especially in small biopsies.
Carcinomatous meningitis can also spread to the ear in late stages, and if the primary tumor is unknown, it can be difficult to make the correct diagnosis. Anamnestic information is mandatory, and a pathologist should use a broad panel of immunohistochemical markers at least for epithelial malignancies (especially from lung, breast, kidney, gastrointestinal tract) and melanoma. Regarding tumors that share the same cellular origin as schwannomas, it is essential to recognize histologic, architectural, and morphologic features. Indeed, neuroma is a capsulated schwannoma and may show focal cellular palisading but presents a peripheral rim of EMA-positive elements. Neurofibroma shares with schwannoma the presence of a certain proportion of myxoid stroma, although hypocellular areas are absent and fibrous capsules are usually absent. Malignant peripheral nerve sheath tumors (MPNST) are composed of malignant elements with atypia and pleomorphism, infiltrative growth, and high mitotic activity.
The external auditory canal's associated lobular capillary hemangioma must be differentiated from more common lesions such as epithelial malignancies like squamous and basal cell carcinoma, amelanotic melanoma, and viral cutaneous lesions such as warts. In all of these cases, morphologic evaluation of the specimen reveals the vascular nature of the lesion and, in selected cases, immunohistochemistry can exclude epithelial elements that are positive for cytokeratin and melanoma.
The combination of two different lesions in this anatomical area is occasionally reported in the literature, as only another case of schwannoma of the external auditory canal showed thick-walled blood vessels on the surface, but this feature was strictly related to chondroid metaplasia of the cartilaginous portion of the external auditory canal [19].
For the clinical case herein described, the most likely hypothesis is that of a single lesion arising from the ponto-cerebellar angle or from the internal auditory canal, with unusually rapid growth resulting in medio-lateral expansion, involving middle ear structures, and providing an extension at the level of the external ear, with vascular secondary proliferation due to the rapid growth of schwannoma.
As the average growth rate of a vestibular schwannoma is approximately 1 mm per year, and the schwannoma rarely exhibits the pseudo-aggressive behavior described here, these two features contributed to the challenging diagnostic process [39].
In fact, 13 and 9 years before diagnosis, the patient presented with a normal MRI and no evidence of a vestibular nerve lesion. In 2021, the lesion measured a maximum diameter of 2.1 centimeters, leading to the hypothesis that the growth rate was almost double the normal rate.
The clinical and anatomopathological cases we have described are extremely rare and present challenging clinical, imaging, and histopathological features. Indeed, it is a histologically benign tumor, with unexpected and rapid growth. Moreover, the distal part of the lesion, firstly biopsied, diagnosed as a vascular benign neoplasm, lead to difficulties in decisions on patients' management. Clinically, the anacusis associated with the lesion lead clinicians to not simply rule out the involvement of neural and middle ear structures, with consequent further imaging investigations, allowing complete and rapid surgical management before their spread could lead to further impairment of important neural and bone structures and thus deliver further functional deficits. Dual treatment, with otosurgery and gamma knife radiotherapy, led to optimal control of the lesions at 24 months of follow-up, with no side effects or sequelae.
In conclusion, it is mandatory to investigate external ear lesions that are localized and benign on histopathological examination, as they can hide a more severe and complex disease that has to be rapidly managed.
Conflict of Interest: all authors declare they have nothing to disclose.
Informed consent: informed consent was obtained from all individual participants included in the study.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.