AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Ahmed Ramadan Saad Zidan, Department of Orthopedic Surgery, Faculty of Medicine, Misr University for Science and Technology, Egypt.
Citation: Waleed A El Tohamey, Ahmed R S Zidan, Mohamed S Hamza, and Hossam M Safouh, (2024), Use of Peroneus Longus Tendon as Autograft for Anterior Cruciate Ligament Reconstruction: A Prospective Interventional Study, J Clinical Orthopaedics and Trauma Care, 6(3); DOI: 10.31579/2694-0248/086
Copyright: © 2024, Ahmed Ramadan Saad Zidan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 11 March 2024 | Accepted: 21 March 2024 | Published: 29 March 2024
Keywords: anterior cruciate ligament; bone–patellar tendon– bone
Background: The anterior cruciate ligament (ACL) is considered the main passive structure that maintains the stability of the knee with the femur and the tibia. The main function of the Anterior cruciate ligament is to limit the tibial forward movement and knee varus and valgus in the state of extension. The Anterior cruciate ligament runs anteriorly, medially, and distally to the tibia. Its length ranges from 22 to 41 mm (mean, 32 mm (, and its width from 7 to 12 mm.
Objective: To assess the functional outcome and donor site morbidity of the peroneus tendon in ACL reconstruction.
Patients and Methods: This Prospective Observational Study was conducted at tertiary care hospital at Misr University for Science and Technology Hospital (Souad Kafafi Hospital) from June 2022 to October 2023 and performed on a total of 20 patients who presented with unilateral anterior cruciate ligament and underwent reconstruction by using of peroneus longus tendon as autograft.
Results: As regards operative characteristics, the current research study revealed that the time from injury to surgery ranged between 2 to 25 weeks with mean of 9.45 ± 7.39 weeks. The total operative time was ranged between 34.5 to 55 min with mean of 42.26 ± 4.66 min. The harvest graft time was ranged between 6.4 to 8.2 min with mean of 7.38 ± 0.53 min and the graft diameter ranged between 7.5 to 8.8 mm with mean of 8.15 ± 0.36 mm. As regards A.O.F.AS score follow-up, our study results revealed that the A.O.F.AS score was increased in the studied group after 6 weeks with a weak significant improvement of AOFAS after 6 months of treatment. As regards I.K.D.C score, our study results revealed that there was highly significant improvement of IKDC score in the study group at 6 weeks postoperatively. As regards the return to normal activity, our study result revealed that the minimum time for normal activity was 2.5 month and the maximum time was 12 months in our patients with mean of 6.05 ± 2.98 months. As regards complications, our study results revealed that few postoperative complications were recorded such as superficial infection in 2 cases (10%), hemarthrosis in 2 cases (10%) and only one case (5%) had arthro-fibrosis and one case (5%) failed.
Conclusions: Peroneus longus tendon (PLT) is a promising graft in ACL reconstruction. It is considered the first-option graft in ACL reconstruction as it provided good functional results, prevented potential complications of the autograft harvested from the knee region, and did not significantly affect the ankle joint and demonstrated the absence of significant post-operative morbidity regarding biomechanical inconveniency to the ankle donor site. Given these findings, PLT autograft is a suitable alternative graft choice from outside the knee for patients undergoing ACL reconstruction.
The Anterior cruciate ligament (ACL) reconstruction improves knee stability and function with many graft types, either autografts or allografts, which have already been studied extensively. Among these grafts, bone–patellar tendon– bone (BPTB) and four-strand hamstring autografts are the two most common autografts used for ACL reconstruction and each has its advantages and disadvantages [1].
According to the latest studies, BPTB is the best graft choice because it has bone-to-bone healing which permits the effective incorporation of tunnel and graft, leading to a faster return to function and sports activity. This characteristic is important in professional athletes with ACL injuries. However, it carries the risk of patellar fracture, with an invasive approach and a large incision, fixed length and a weaker than native ACL, making it unsuitable for double-bundle reconstruction and anterior kneeling pain. Pain free kneeling is considered very important in the Asian population, especially in Indonesians, who kneel rigorously when praying. For these reasons, hamstring autografts are becoming popular in the Asian population [2].
A hamstring autograft is easy to harvest with minimal donor site morbidity and strength that is comparable to that of the native ACL. On the other hand, it has unpredictable graft size and a potential decrease in hamstring power, which is crucial for some athletes who need dominant hamstring power. Some orthopedic surgeons are therefore attempting to use the peroneus longus tendon as a graft [3].
Peroneus longus tendon autografts are commonly used in some orthopaedic procedures, including spring ligament reconstruction, deltoid ligament reconstruction and medial patellofemoral ligament (MPFL) reconstruction (4) (anterior half of the peroneus longus tendon). This is possible, due to the synergistic function of the peroneus longus and peroneus brevis. Some studies have even found that the peroneus brevis is a more effective evertor of the ankle, justifying the harvest of the peroneus longus tendon [5].
Some previous case series reported using the peroneus longus tendon as the first choice for an autograft in ACL reconstruction, with good clinical outcome and minimal donor site morbidity, while other studies did not agree, due to donor site morbidity. In 2017, Phatama et al. reported that there was no significant difference between the peroneus longus and hamstring tendon in terms of tensile strength [6].
Consequently, the purpose of this study is to assess the functional outcome and donor site morbidity of the peroneus tendon in ACL reconstruction. If a peroneus longus autograft does in fact show an effective functional outcome with less donor site morbidity compared with the hamstring tendon, its use as the graft of choice in single-bundle ACL reconstruction can be encouraged in clinical practice, especially in the group of patients in whom dominant hamstring power is needed or the group of patients who frequently kneel as part of their daily religious activity, where any anterior kneeling pain could not be tolerated [5].
In this thesis, authors aim to assess the functional outcome and donor site morbidity of the peroneus tendon in ACL reconstruction.
After ethical committee approval and informed consent from the patients, this Prospective Observational Study was conducted at tertiary care hospital at Misr University for Science and Technology Hospital (Souad Kafafi Hospital) from June 2022 to October 2023 and performed on a total of 20 patients who presented with unilateral anterior cruciate ligament and underwent reconstruction by using of peroneus longus tendon as autograft.
Inclusion criteria: Patients with an isolated rupture of the ACL. Age between 16-45 years. All patients were diagnosed with ACL tear on clinical and radiological examination (magnetic resonance imaging [MRI]), included in the study.
Exclusion criteria: Associated ligament injury. Chondral damage. Meniscal injury. Fracture around the knee. The presence of a pathological condition in the lower extremity or an abnormal contralateral knee joint.
Preoperative Assessment:
Clinical Assessment: Patients underwent a comprehensive medical history evaluation to ascertain general health status and identify any relevant medical comorbidities. Clinical history included inquiries regarding pain, instability (giving way), swelling (hemarthrosis), locking, and any audible "pop" or "snap" sensations experienced. Physical examination techniques included: Inspection for lower limb alignment and gait abnormalities. Palpation of the affected knee joint to assess effusion and identify tender points. Assessment of range of motion (ROM) and thigh circumference. Evaluation of neurovascular status to ensure limb integrity. Special tests for ligamentous injuries, including. Lachman test, anterior drawer test, pivot shift test, valgus and varus stress tests, and McMurray’s test for meniscus injury, were performed as indicated.
Radiographic Diagnosis: Standard anteroposterior (AP) and lateral X-ray views, complemented by magnetic resonance imaging (MRI), were obtained for all patients to confirm ACL insufficiency and assess associated knee pathology.
Laboratory Investigations: Preoperative routine laboratory tests encompassed complete blood count, coagulation profile, liver and kidney function tests, and blood glucose levels.
Scoring System: Subjective and objective International Knee Documentation Committee (IKDC) scores and Lysholm Knee Scoring Scale were recorded upon admission (preoperatively) and at 6 month and 12 months postoperatively to establish baseline and postoperative functional assessments.
Operative Preparation: Patients received a single preoperative dose of prophylactic antibiotic (first-generation cephalosporin) within one hour preceding skin incision. All surgeries were performed under spinal anesthesia.
Operative Technique:
Surgical Approach and Graft Harvesting:
A tourniquet is applied to the proximal thigh to facilitate visualization and hemostasis during the procedure. The surgical team begins by making a small longitudinal incision approximately 2 cm proximal and 1 cm posterior to the lateral malleolus. Careful dissection is performed to expose the peroneus longus tendon (PLT) while preserving the integrity of surrounding neurovascular structures including the superficial peroneal nerve.
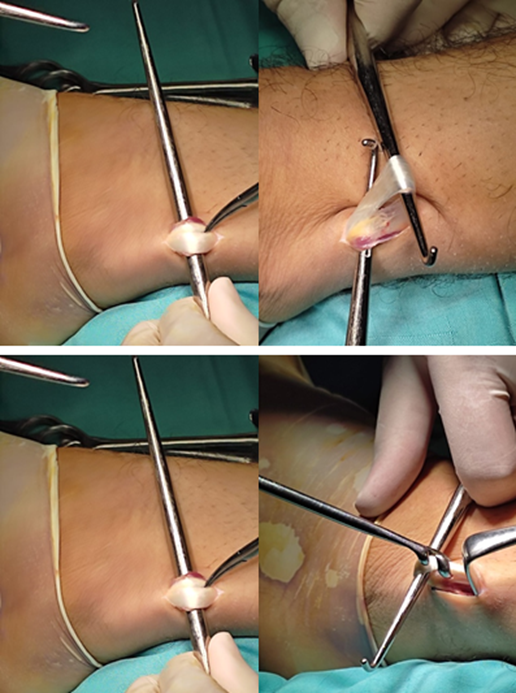
Figure 1: Incision and graft harvesting and discrimination of proneus Longus tendon.
Special attention is paid to identifying the course of the PLT as it courses distally along the lateral aspect of the leg. Once adequately exposed, the PLT is carefully dissected free from its surrounding sheath, taking care to maintain its structural integrity and minimize trauma to the tendon fibers.
A tendon stripper or similar device may be used to facilitate the harvesting process, ensuring a smooth and controlled extraction of the PLT. The length and diameter of the harvested tendon are meticulously assessed to ensure suitability for ACL reconstruction.
Graft Preparation and Suturing:
With the PLT harvested, the surgical team proceeds to prepare the tendon graft for ACL reconstruction. Any excess soft tissue is trimmed, and the graft is carefully cleansed to remove debris and blood clots. The PLT is then sized appropriately based on preoperative measurements and intraoperative assessment. Suturing of the PLT may be performed using high-strength, non-absorbable sutures to ensure secure fixation and stability of the graft. Care is taken to maintain proper tension and alignment throughout the suturing process, minimizing the risk of graft misalignment or laxity.
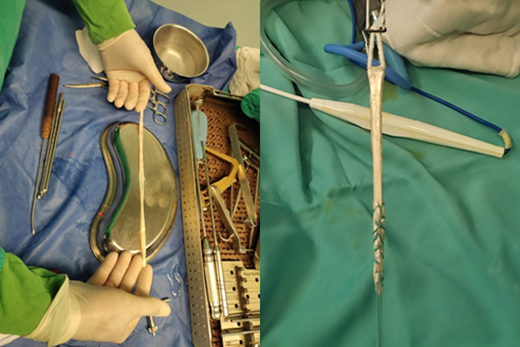
Figure 2: Graft preparation.
Arthroscopic ACL Reconstruction:
With the PLT graft prepared and sutured, attention is turned to the arthroscopic aspect of the procedure. Standard arthroscopic portals are established, including anteromedial and anterolateral portals, allowing for comprehensive visualization of the knee joint. Arthroscopic instrumentation is utilized to assess the integrity of the ACL stump and identify any associated intra-articular pathology, such as meniscal tears or chondral lesions.
Tunnel Creation and Graft Fixation:
The intercondylar notch is viewed through the AL portal and remnants of the torn ACL are resected using a basket punch and motorized shaver blade inserted into the knee joint through the AM portal. Some of the native ACL tissue is preserved at the femoral and tibial attachment sites to aid with later placement of the ACL femoral and tibial tunnels.
Femoral Tunnel
The femoral tunnel's optimal placement in ACL reconstruction is paramount for achieving biomechanical stability and successful graft integration. The preferred tunnel center is meticulously determined Although the clockface reference method has often been used to specify the location of the ACL femoral tunnel, the clockface reference method has several shortcomings: it ignores the depth of the intercondylar notch. In most situations, there are remnants of the native ACL present to aid with anatomic ACL femoral tunnel placement. This “eyeball” technique is fairly accurate.
Lateral Intercondylar and Bifurcate Ridges When there are no remnants of the native ACL present, the underlying bony morphology of the ACL femoral attachment site can provide useful anatomic landmarks to assist with anatomic ACL femoral tunnel placement. the tunnel center is precisely positioned between the lateral intercondylar ridge and the posterior articular margin. This alignment, combined with a distance of approximately 2.5 mm plus the planned tunnel radius from the posterior articular cartilage, centers the tunnel directly over the lateral bifurcate ridge.

Figure 3: Creation femur tunnel.
Tibial Tunnel
A standard tibial guide is set to around 55 and is used to create an anatomic tibial aperture with whichever tunnel orientation and length are desired. The tibial tunnel is placed 9 mm posterior to the intermeniscal ligament or 7 to 10 mm anterior to the posterior cruciate ligament insertion with the center of the tunnel ideally being just posterior and medial to the anterior horn of the lateral meniscus. This allows for an anatomic recreation of the tibial footprint of the ACL

Figure 4: Creation femur tunnel.
Graft Passage and Fixation
On the femoral side, an EndoButton is utilized for suspensory fixation, while a Bio bioabsorbable interference screw is employed on the tibial side.
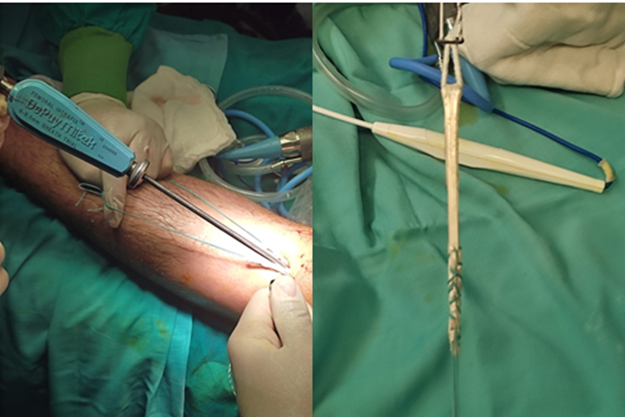
Figure 5: Graft passage and fixation.
Post-operative Care:
Recovery Room: Upon completion of the surgical procedure, patients were carefully monitored in the recovery room.
In the Ward (Antibiotics): Following surgery, patients received intravenous first-generation cephalosporin antibiotics administered in two divided doses for 3 days postoperatively to prevent infection.
Drain Removal: Surgical drains were removed 24 hours after the procedure to facilitate the healing process.
Early Mobilization: Patients were encouraged to initiate movement on the day of surgery, including, protected full weight-bearing as tolerated with crutches, passive range of motion exercises (0° - 90°).
Discharge: All patients were discharged the day after surgery, under the guidance of the medical team.
After Discharge: Following discharge, patients received routine prophylaxis for thrombosis for a duration of two weeks. Regular clinical evaluations were scheduled during the follow-up period to monitor progress and address any concerns.
Wound Care: Wound inspection and suture removal were performed after two weeks to assess healing progress and ensure optimal wound management.
Range of Motion Assessment: At the two-week post-operative mark, patients underwent evaluation to assess the full range of motion in the affected knee. Rehabilitation efforts were tailored to facilitate immediate full weight-bearing as tolerated and encourage full range of motion. No restrictive rehabilitation braces were utilized.
Postoperative Rehabilitation Program:
Phase I: This phase spanned from injury until surgical reconstruction in acute cases. Criteria for advancement to the next phase included minimal to no swelling in the knee, full range of motion, and normal gait without limping.
Phase II: Beginning on the day of surgery and continuing through the second postoperative week, this phase involved cold therapy, protected full weight-bearing as tolerated with crutches, passive range of motion exercises (0° - 90°), and quadriceps muscle strengthening exercises through isometric contraction exercise. Closed chain exercises, such as sitting on a chair with a skateboard under the sole, were employed to promote hip, knee, and ankle mobility.
Phase III: From the third to sixth postoperative weeks, patients progressed to non-protected full weight-bearing, gradual achievement of full range of motion, and implementation of quadriceps, hamstrings, calf, and proprioception exercises. Stair climbing was recommended during the initial four postoperative weeks, with the healthy leg leading during ascent and the operated leg leading during descent.
Phase IV: Commencing at the end of the sixth week until the patient's return to full athletic competition (typically around six months postoperatively), this phase included exercises such as leg press exercises, dynamic hip abduction with the contralateral leg, and running. Running activities were only permitted after six months, provided that patients had regained full subjective functional stability.
Follow-up Evaluation:
All patients underwent regular follow-up evaluations at two-week intervals up to the second postoperative month, followed by assessments at three months, six months, and twelve months postoperatively. At the twelve-month mark, patients underwent comprehensive evaluation according to predefined parameters:
Clinical Evaluation: Postoperative clinical assessment mirrored preoperative evaluation criteria. Additionally, examination of the graft donor site was performed to assess tenderness, irritation, and any abnormal sensations in the surrounding skin.
Postoperative Rating Scales: Following clinical and radiographic assessments, postoperative rating scales were calculated. The IKDC scoring system, including subjective and objective evaluations, were utilized for comprehensive assessment at the six,twelve-month postoperative milestone, and Functional assessment of the ankle joint was done by use of the American Orthopedic Foot and Ankle Score (AOFAS)–Hindfoot
Outcome Measurement:
Knee stability and function were evaluated clinically by using Lachman test and KT‑2000 arthrometer as well as subjectively with the International Knee Documentation Committee (IKDC) score at 6 months postoperatively.
A. Functional outcome
1. The Lachman test:
The Lachman test was given grades (1, 2, and 3) depending on the amount of anterior translation (3–5 mm, 5–10 mm, and >10 mm, respectively) for the tibia over the femur.
2. KT‑2000: KT‑2000 was graded as 0–2 mm, 3–5 mm, and >6 mm displacement.
3. (IKDC): the International Knee Documentation Committee score
3. AOFAS: the American Orthopedic Foot and Ankle Score.
Functional assessment of the ankle joint was done by use of the American Orthopedic Foot and Ankle Score (AOFAS)–Hindfoot scale.
B. Patient Satisfaction:
Patients were subjectively asked for the satisfaction of their return of function of the affected knee, and movements of ankle joint restriction were noted down with comparison to the other ankle joint.
C. Complications: e.g DVT, Wound infection, Implant failure.
The collected data was coded, tabulated, and statistically analyzed using IBM SPSS statistics (Statistical Package for Social Sciences) software version 22.0, IBM Corp., Chicago, USA, 2013 and Microsoft Office Excel 2007. Descriptive statistics were done for quantitative data as minimum& maximum of the range as well as mean±SD (standard deviation) for quantitative normally distributed data, while it was done for qualitative data as number and percentage. Inferential analyses were done for quantitative variables using Shapiro-Wilk test for normality testing, independent t-test in cases of two independent groups with normally distributed data. In qualitative data, inferential analyses for independent variables were done using Chi square test for differences between proportions and Fisher’s Exact test for variables with small expected numbers. The level of significance was taken at P value < 0>
In order to highlight the efficiency of neuro-dynamic techniques compared to classical recovery, I will further present graphically the values obtained from the tests used.
Table 1: Patients characteristics of the studied population.
| Gender | No. | % | c2 | P |
| Males | 17 | 85.0 | 13.64 | 0.000* |
| Females | 3 | 15.0 | ||
| Total | 20 | 100 | ||
| Laterality | No. | % | c2 | P |
| Right | 15 | 75.0 | 10.27 | 0.000* |
| Left | 5 | 25.0 | ||
| Age | Min | Max | ||
| Range (years) | 16 | 46 | ||
| Mean ± SD (years) | 25.65 ± 7.645 | |||
c2: Chi square, p >0.05: non-significant, *p <0>
Table 2: Mechanism of injury in the studied patients.
| Treatment | No. | % |
| Rapid change of direction | 2 | 10 |
| Football tackle | 6 | 30 |
| Direct trauma | 6 | 30 |
| Falling down while running | 2 | 10 |
| Falling down and twisting | 1 | 5 |
| Landing from a jump incorrectly | 2 | 10 |
| Traffic accident | 1 | 5 |
| Total | 20 | 100 |
Table 3: Incidence of comorbidities of the studied patients.
| Treatment | No. | % |
| Smoking | 7 | 35 |
| Obesity | 2 | 10 |
| Hypertension | 2 | 10 |
| Diabetes mellitus | 2 | 10 |
Table 4: Diagnostic tests of the studied patients.
| Test | Positive | Negative | Significance | |||
| No. | % | No. | % | χ2 | P | |
| Anterior drawer | 20 | 100 | 0 | 0.00 | 168.0 | 0.000* |
| Pivot shift test | 20 | 100 | 0 | 0.00 | 168.0 | 0.000* |
Grade: 1 2 3 | 1 8 11 | 5.00 40.0 55.0 | 12.37 | 0.000* | ||
| Lachman | Range | Mean ± SD | ||||
| Translation | 5 – 17 | 10.2 ± 3.44 | ||||
c2: Chi square test, p <0>
Table 5: Operative data of the studied patients.
| Data | Range | Mean ±SD |
| Time before surgery (weeks) | 2 – 25 | 9.450 ± 7.388 |
| Operative time (minutes) | 34.5 – 55 | 42.255 ± 4.659 |
| Time for graft harvest (minutes) | 6.4 – 8.2 | 7.375 ± 0.534 |
| Graft diameter (mm) | 7.5 – 8.8 | 8.15 ± 0.36 |
Table 6: Comparison between the American Orthopedic Foot and Ankle Score (AOFAS) preoperatively and 6 months postoperatively.
| AOFAS | Preoperative | Postoperative | t | p |
| Range | 90 – 99.8 | 95 – 99.5 | ||
| Mean ±SD | 97.61 ± 3.328 | 98.42 ± 0.974 | 0.985 | 0.047* |
t: unpaired t-test, p <0>
Table 7: Comparison between the International Knee Documentation Committee (IKDC) score preoperatively and 6 months postoperatively.
| IKDC | Preoperative | Postoperative | t | p |
| Range | 75.5 – 84.1 | 91.5 – 95.5 | ||
| Mean ±SD | 79.68 ± 2.73 | 93.88 ± 1.176 | 1.826 | 0.009* |
t: unpaired t-test, p <0>
Table 8: Time to return to normal activity.
| Time (month) | Min | Max | Mean ±SD |
| Return to normal activity | 2.5 | 12 | 6.05 ± 2.98 |
Table 9: Postoperative complications.
| Time (month) | No. | % |
| Infection | 2 | 10.0 |
| Hemarthrosis | 2 | 10.0 |
| Arthrofibrosis | 1 | 5.0 |
| Failure | 1 | 5.0 |
An active 29years-old man presented with a swollen Right knee during football playing. x-ray scan revealed no knee O.A, and a MRI scan showed a full thickness tear of the ACL intact medial and lateral meniscus. The posterior cruciate and collateral ligaments, were normal. Clinically, the knee had marked antero-posterior laxity. The pre-operative tests revealed lachman +3 and positive anterior drawer tests,pivot test positive. The IKDCs was70.9, he underwent an arthroscopic ACL reconstruction with peroneus longus tendon graft.
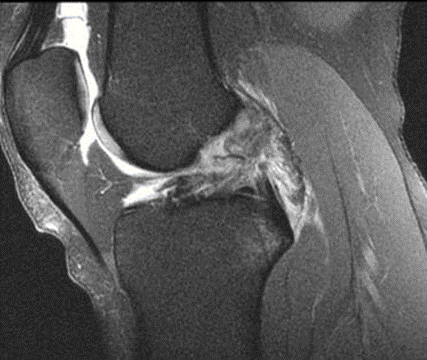
Figure 6: Pre-operative MRI.
The graft was peroneus longus tendon auto-graft, fixed by inter ferance biodegradable screws on tibial side and end button on femor side. Postoperative laxity tests and pivot shift were done.

Figure 7: Postoperative full extension 3 months.
Physiotherapy Protocols were followed. MRI scan at 6 months showed the reconstruction to be intact, after reconstruction, his knee on examination was stable and the patient IKDCs was 85.2.
Figure 8: Postoperative 6months MRI state of the graft.
An active 64 years-old man presented to us with a swollen and painful right knee following falling down while running. This patient had no previous injuries to the knee and x-ray scan revealed no knee O.A, and a MRI scan a full thickness tear of the ACL. The posterior cruciate and collateral ligaments, medial and lateral meniscus was normal.

Figure 9: Preoperative MRI showing torn ACL.
At this point, the 0patient had received no treatment and had symptomatic instability and occasional pain. Clinically, the knee had marked antero-posterior laxity. The pre-operative tests revealed positive lachman +3 and positive anterior drawer, and pivot test. The IKDCs was 66.4. The option of surgical reconstruction was chosen. he underwent an arthroscopic ACL reconstruction with the traditional technique. The graft was peroneus longus tendon graft auto-graft.
Postoperative laxity tests and pivot shift were excellent. Standard physiotherapy protocols were followed. MRI scan at 6 months showed the reconstruction to be intact, after reconstruction, his knee on examination was stable and the patient IKDCs was 90.7.
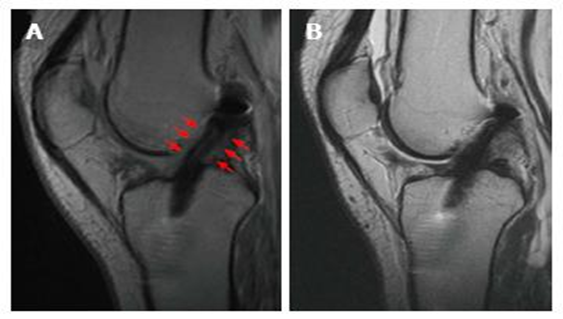
Figure 10: 6 months Post-operative MRI.
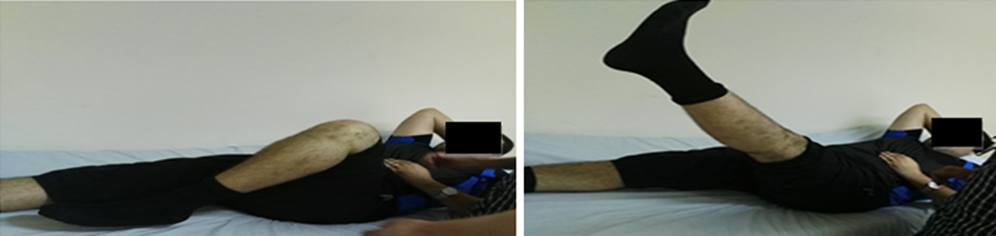
Figure 11: 6 Month ROM.
Anterior cruciate ligament reconstruction (ACLR) has been recognized as the standard treatment to restore knee stability and joint function after an ACL rupture. Several autograft options are currently used for ACLR, such as bone-patellar tendon-bone, hamstring tendon, and quadriceps tendon. Each of these autografts has advantages and disadvantages. Surgeons should consider the graft strength, size, and safe and easy graft harvesting with minimal donor site morbidity [7].
Some studies suggested peroneus longus tendon as an alternative autograft option for ACLR. The peroneus longus tendon has adequate size, and biomechanical evaluations of its properties revealed it has sufficient strength for knee ACLR [8].
Since various surgical approaches for management of ACL reconstruction represent major conflict and may be associated with complications, evaluating the functional outcome and knee stability results of ACL reconstruction using PLT graft was highlighted as a main point of interest [9].
Consequently, the current study was conducted and aimed to assess the functional outcome and donor site morbidity of the peroneus tendon in ACL reconstruction.
This Prospective Observational Study was conducted at tertiary care hospital at Misr University for Science and Technology Hospital (Souad Kafafi Hospital) from June 2022 to October 2023 and performed on a total of 20 patients who presented with unilateral anterior cruciate ligament and underwent reconstruction by using of peroneus longus tendon as autograft.
During this study, 33 patients were assessed for eligibility and 20 patients were included in the study. Of all eligible patients, 8 patients were excluded from the study based on the inclusion criteria and 5 patients refused to participate in of the study.
Ultimately, the analysis was based on the data of 20 patients who presented with unilateral anterior cruciate ligament and underwent reconstruction by using of peroneus longus tendon as autograft.
The current study revealed that there were 17 males (85%) and 3 females (15%) with statistically significant difference (p <0>
As regards Mechanism of injury, the current research study revealed that the most common etiologies for injury were football tackle in 6 cases (30%) and direct trauma in 6 cases (30%), followed by rapid change of direction (10%), falling down while running (10%), and landing from a jump incorrectly each in 2 cases (10%), while only 1 case (5%) with traffic accident and 1 case (5%) with falling down and twisting.
Anterior drawers test, Lachman’s test and pivot shift test were done preoperatively during an examination of the knee joint to confirm the diagnosis and assess the amount of translation. postoperatively at 1 year follow-up anterior drawers test, Lachman’s test and pivot shift test were repeated to check for anterior translation [10].
Accordingly, our study results revealed that the anterior drawer test and Pivot shift test were positive in all cases (100%). Lachman grade [1], was found only in one case (5%), grade (2) in 8 cases (40%) and most of patients 11 (55%) were grade (3) with statistically highly significant difference in comparison between the three grades (p <0>
As regards operative characteristics, the current research study revealed that the time from injury to surgery ranged between 2 to 25 weeks with mean of 9.45 ± 7.39 weeks. The total operative time was ranged between 34.5 to 55 min with mean of 42.26 ± 4.66 min. The harvest graft time was ranged between 6.4 to 8.2 min with mean of 7.38 ± 0.53 min and the graft diameter ranged between 7.5 to 8.8 mm with mean of 8.15 ± 0.36 mm.
In concordance with our findings, Joshi et al. (9) conducted a prospective interventional study that enrolled 48 patients to evaluate the functional outcome and knee stability results of ACL reconstruction using PLT graft and revealed that 36 were male and 12 were female. The mean age of the patients was 27.2 years, with a range of 18–36 years. Regarding the cause of injury, 19 (39.58%) of the patients had injuries due to road traffic accidents, 17 (35.41%) due to sports, 7 (14.5%) assault, and 5 (10.41%) domestic accidents. The graft harvest time was 7.4 min ranging from 5 to 9 min. The mean thickness of the graft on doubling was 7.9 mm (7–9 mm).
Furthermore, the mean time for harvesting the graft was 7.4 min. This shorter duration is important as it saves a significant amount of tourniquet time for reconstruction of the ACL per se. A less experienced surgeon can easily harvest the PLT graft, compared to bone patellar tendon bone (BPTB) and HT graft, which builds up the confidence in the surgeon. The ease of the procedure decreases the chances of mistakes during reconstruction [9].
Diameter of the autograft in ACL reconstruction surgery is an important factor contributing to failure. The exact graft diameter needed to avoid such failure rates is not clear [9]. Xu et al., [11] concluded that when graft sizes larger than 8.5 mm were selected, the clinical outcomes were superior in the autograft group. They also suggested the importance of restoring the insertion site to at least 60%–80% of cross‑sectional area during anatomic ACL reconstruction [12]. A review article by Figueroa et al., [13] recommended that even an increase of 0.5 mm up to a graft size of 10 mm is beneficial to the patient. In our study, the mean graft diameter was 8.7 mm ranging from 7.9 mm to 9.1 mm. Rhatomy et al., [14] compared the graft thickness of quadruple hamstring and peroneus and concluded that there was a mean difference of 0.6 mm in favor of peroneus longus graft.
Wiradiputra et al., [15] used PLT graft to replace the injured ACL and found that the diameter of the PLT graft was 8.5 mm, which was larger than the ideal in diameter so that the reconstruction could be performed rapidly. However, Magnussen et al., [16] stated the ideal minimum graft diameter of 7 mm is best to avoid revision surgery. Other studies affirmed that a graft diameter of no less than 8 mm is the acceptable range for reconstruction (17, 18).
As regards A.O.F.AS score follow-up, our study results revealed that the A.O.F.AS score was increased in the studied group after 6 weeks with a weak significant improvement of AOFAS after 6 months of treatment (p = 0.047).
As regards I.K.D.C score, our study results revealed that there was highly significant improvement of IKDC score in the study group at 6 weeks postoperatively (p-value =0.009).
Various studies reported good results after ACL reconstruction with the peroneus longus tendon, in terms of both functional outcome and knee stability [19-21]. Our study supports that assertion.
Our study assessed the functional outcome of the knee and ankle using AOFAS, and IKDC to determine the morbidity and stability.
There were controversial evidences when ankle functional outcomes were evaluated. Angthong et al., [20] had reported a reduction in ankle peak torque eversion and inversion. However, a study by Rhatomy et al., [14] compared hamstring with PLT autograft and did not find any significant difference between the 2 in 1 year follow‑up, although considered only the functional outcome scores of ankle joint which were normal on follow‑up and also showed similar results in AOFAS score at end of 1 year compared to preoperative assessment without significantly affecting the ankle functions.
In concordance with our findings, Joshi et al., [9] reported that the mean IKDC score postoperatively was 78.16 ± 6.23, and the mean AOFAS score was 98.4 ± 4.1 and none of the patients had any neurovascular deficit. Moreover, there was no obvious effect of harvesting PLT while examining the arch of the foot. On checking ankle stability by anterior and posterior drawer test, we found no difference from the contralateral limb. None patients had any complaints pertaining to the ankle joint. This can be attributable to the regeneration potential of harvested full‑thickness tendon. This has been shown both clinically and by MRI Takeda et al., [22], thus making patient free from any complaints of ankle joint.
In support of our results, a prospective study on 25 patients was conducted to evaluate functional outcomes after ACL reconstruction using a triple-layered PL graft. Khajotia et al., [23] observed that there was an improvement in IKDC score with no patients having ankle dysfunction but 2 patients had pressure pain at the graft harvest site at the end of 6 months.
In agreement with our findings, Wiradiputra et al., [15] revealed that there was no limitation of ankle eversion and first ray plantar flexion with good ankle motor strength. AOFAS analysis was 100% at end of 1 year and concluded that peroneus longus can be used as the first option in ACL reconstruction because there was no significant postoperative morbidity associated with biomechanical inconveniency to the donor site.
Moreover, Sholahuddin et al., [24] conducted a prospective study that followed up the patients for 2 years who underwent peroneus longus graft for ACL reconstruction and observed excellent IKDC, MCS, Tegner-Lysholm score, AOFAS and FADI scores. In addition, good graft diameter was harvested, thigh hypotrophy was less, with excellent ankle function and a better serial hop test result was achieved.
Comparative studies on the use of HT and PLT grafts showed no significant differences between the pre- and 1-year post-surgery, based on the IKDC, modified Cincinnati, and Lysholm Knee Scoring Scale. The PLT graft was considered more superior because it provides larger graft diameter and less thigh hypotrophy with excellent ankle function based on AOFAS and Foot and Ankle Disability Index (FADI) [14, 25].
Bi et al., [26] compared the use of single-bundle anterior half of PLT vs. semitendinosus tendon. At the 2-year follow-up, the study found no differences between both groups in the VAS scale, IKDC score, pivot shift test, and KT-1000. Besides, the AOFAS score in the PLT group was more excellent than the semitendinosus tendon group. This finding concluded that PLT graft provides greater strength and relatively safe for reconstruction.
Analyzing the functional outcome using Lysholm score and Modified Cincinnati scores for the knee joint and American Orthopedics Foot and Ankle Scoring for ankle joint, Vijay et al., [10] reported that PL autograft showed improved Lysholm score and modified Cincinnati functional scores. There was better knee flexion strength improvement at the end of 1 year in the PL group compared to the HST autograft group. AOFAS score also showed significant improvement at the end of 1 year in the PL group.
In agreement with our results, Keyhani et al., [7] compared the clinical outcome and donor site morbidity in ACLR using peroneus longus tendon autograft versus hamstring tendon autograft and revealed that FADI score, and AOFAS score were used to evaluate donor ankle morbidity after peroneus longus harvesting and no patient experienced ankle joint dysfunction or difficulty in sports activities due to peroneus longus autograft transfer. There was no significant difference in ankle ROM for all movements between the peroneus longus harvested compared to the contralateral side.
As regards the return to normal activity, our study result revealed that the minimum time for normal activity was 2.5 month and the maximum time was 12 months in our patients with mean of 6.05 ± 2.98 months.
As regards complications, our study results revealed that few postoperative complications were recorded such as superficial infection in 2 cases (10%), hemarthrosis in 2 cases (10%) and only one case (5%) had arthro-fibrosis and one case (5%) failed.
In concordance with our results, Joshi et al., [9] revealed that a there was one patient with superficial infection (Staphylococcus aureus) at the graft donor site which was treated with oral antibiotics (cefoperazone). None of the patients had any neurovascular deficit. The mean follow‑up duration was 19.4 months (15–24 months). Forty‑six (95.83%) patients were satisfied with their results of the knee surgery, and 45 (93.75%) patients had no complaints of ankle joint postoperatively.
Donor site morbidity is an important consideration while looking for a graft for ACL reconstruction. Most widely used BPTB autograft is associated with complaints of anterior knee pain and kneeling pain postoperatively [27, 28]. A meta‑analysis of studies has shown an increased incidence of osteoarthritis in a BPTB autograft ACL reconstruction of knee. It has also documented that this autograft has an increased incidence of adhesions leading to extension deficit [29].
Vijay et al., [10] compared the functional outcome and donor site morbidity between hamstrings and peroneus longus autograft in anterior cruciate ligament reconstruction and revealed that anterior kneeling pain was also found in about 27% of patients after hamstring tendon harvesting in the HST group, while no patients developed any ankle pain, numbness over the knee joint or ankle joint and limitation of the movement at the ankle joint.
Keyhani et al., [7] revealed that no pain or complaint about the weakness of the ankle joint, vascular and neurological complications, or other discomforts over the donor site of the ankle was noted. No serious instability or complication was found in both groups. Thigh hypotrophy was considerably more significant in the hamstring tendon group compared to the peroneus longus group at a minimum of 2 years of follow-up.
He et al., [30] concluded that the PLT graft is suitable as an autograft harvested outside the knee to avoid the complication of quadriceps-hamstring imbalance that may occur after harvesting the graft from the knee.
Regardless of all the advantages of PLT grafts in ACL reconstruction, the graft preference was decided based on various clinical considerations by the surgeons. In achieving an excellent result, the consideration of the appropriate graft usage depends on many factors, including the associated meniscal and ligament lesions, high or low demand patient's activities, medical condition or comorbidities, pre-surgical status, patient decision, and the post-operative rehabilitation protocol [31].
Peroneus longus tendon (PLT) is a promising graft in ACL reconstruction. It is considered the first-option graft in ACL reconstruction as it provided good functional results, prevented potential complications of the autograft harvested from the knee region, and did not significantly affect the ankle joint and demonstrated the absence of significant post-operative morbidity regarding biomechanical inconveniency to the ankle donor site. Given these findings, PLT autograft is a suitable alternative graft choice from outside the knee for patients undergoing ACL reconstruction.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
