AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Krishna MA, Department of Orthopaedics, Bahadur Hospital, India.
Citation: Krishna MA and Madaan E, 2018.“Methodical clinical measurement of knee deformity”, J. Orthopaedics and Surgical Sports Medicine. 1(2); Doi: 10.31579/2641-0427/008
Copyright: © 2018 Krishna MA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 26 September 2018 | Accepted: 17 October 2018 | Published: 22 October 2018
Keywords: nee osteoarthritis; sagittal knee alignment; hip-knee-ankle
The recognition of the pattern and severity of deformity in knee osteoarthritis has important implications in its management and prognosis. A number of methods can be used to assess and measure the coronal and sagittal knee alignment: clinical deformity measuring device like a goniometer, standard knee radiographs, hip-knee-ankle (HKA) radiographs, computer navigation systems, magnetic resonance scan, computerized tomographic scan or simply a surgeon’s subjective measurement. Each of these methods has advantages and disadvantages. The aim of this study was to compare three methods of measurement: clinical measurement with a goniometer; HKA radiographs and computer navigation.
This study included 54 patients with arthritic knees, who underwent total knee replacement with computer navigation. The deformity in both coronal and sagittal planes was measured using the three methods and the results compared using Bland Altman limits of agreement.
The clinical measurement differed greatly from radiographic and computer navigation measurements. According to Bland Altman limits of agreement clinical measurements could be up to 10° away from the radiographic or computer navigated measurements in coronal plane. In the sagittal plane the clinical measurements could be up to 12° away compared to computer navigation measurements.
A combination of these measurements methods should be taken into account when assessing the deformity of a knee especially in relation to posture and weight bearing status. The methodical clinical measurement of knee deformity as described in this paper gives too wide a margin of error and should not be relied upon in isolation.
The recognition of the pattern and severity of deformity in knee osteoarthritis has important implications in its management and prognosis [1-5]. A number of methods can be used to assess and measure the coronal and sagittal knee alignment: clinical deformity measuring device like a goniometer; standard knee radiographs; hip-knee-ankle (HKA) radiographs; computer navigation systems and computerized tomographic scan (CT scan) [5-10]. CT scans can is also be used to assess rotational alignment [11-13]. However many of these modalities are not yet widely available and most surgeons rely on simple clinical assessment and standard knee radiographs. There is evidence in the literature showing that standard short knee radiographs are not sufficient to accurately assess knee alignment [14,15]. There is some suggestion that clinical anatomic axis measurement correlates well with radiographic mechanical axis [6], however in our experience clinical assessment may be inaccurate and can give an incorrect impression of the true deformity pattern. In our practice image-free computer navigation is used routinely for knee replacement and all patients have pre-operative and post-operative coronal hip-knee-ankle radiographs.
The aim of this study was to compare clinical measurements of knee deformity in osteoarthritis to both hip-knee-ankle radiographs and computer navigation measurements and to assess whether pre-operative clinical measurements provided useful information to enable the surgeon to plan the operation accurately.
Materials and Methods
The study was conducted under our institution’s Clinical Governance procedures for prospective audits. Patients with osteoarthritis in knee, admitted for primary total knee replacement with computer navigation in our institute under care of senior author were included in the audit. Those with previous surgery on the knee were excluded. Knee deformity was measured in 54 osteoarthritic knees who had been admitted for primary total knee replacement surgery. Clinical measurements, HKA radiographs and computer navigation measurements were used to assess the deformity. The coronal and sagittal plane deformity were evaluated using clinical and computer navigation measurements. On the radiographs only the coronal plane deformity was measured.
Clinical measurements
Clinical measurement was done on the day of admission. The patient was adequately exposed from the waist down. He/she was then asked to assume usual stance to avoid excessive limb rotation. For coronal plane measurement, surface landmarks were used to identify the hip, knee and ankle centers. The midpoint between the anterior superior iliac spine and the pubic tubercle was marked as the hip center [16].
The center of the knee was marked as the point between the medial and lateral border of the knee. The point in the anterior ankle between the medial and lateral malleolus was marked as the center of the ankle. A long arm goniometer was used to measure the coronal lower limb alignment using these surface landmarks. For flexion deformity, the patient was viewed from the side and the long axis of the thigh and the leg were determined, and the angle between them measured with the goniometer.
Radiographic Measurements
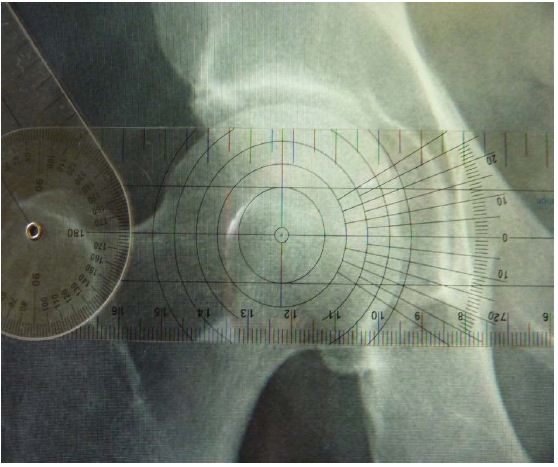
The pre-operative HKA radiographs, as stored in a Picture Archiving System (PACS, Kodak), were measured by two independent observers. The centre of the hip was identified using concentric circles (Figure 2B) [17]. The knee center was identified as the center of the line connecting the femoral trochlear midpoint and upper tibial midpoint. The ankle center was identified as the midpoint of the upper border of the talus [18]. The line connecting the three centers formed the coronal alignment of the knee (Figure 1A)

The measurements were performed by the senior surgeon or a trainee under his supervision.
Demographic data and body mass indices were collected for all patients.
Data Analysis
Deformity was measured as deviation from 180°. Neutrally aligned knees were given as 0°. In the coronal plane varus deformity was indicated as negative (-) and valgus deformity as positive (+). In the sagittal plane flexion deformity was indicated as positive (+) and hyperextension as negative (-). Interobserver agreement for the measurement of the radiographs was analyzed with the intraclass correlation coefficient. The radiographic and navigation measurements were used as baselines to compare with the clinical measurements. Comparisons between groups were made using the Wilcoxon sign ranks test. The Bland Altman method was used to assess agreement between two methods of measurement [19]. For this the differences were always calculated as clinical minus from the baseline (Radiographic or Navigation).
he patient population included 28 males and 26 females with a mean age of 68.4 (SD 8.6). The body mass index (BMI) ranged from 25 to 48.5 with a mean of 32.7 (SD 5.5). The inter-observer agreement between the two sets of radiographic measurement was good (ICC = 0.993). For 53 cases the difference in alignment between observers was 1° or zero. Only one case had a difference of 2°.
Coronal plane assessment
Using HKA radiographic measurement of coronal alignment as a baseline, the mean difference of the clinical measurements was 0.8° (range -12° to +12°). The Wilcoxon sign ranks test showed no statistical difference between the clinical and radiographic measurements (p = 0.173). However the Bland Altman limits of agreement (± 95 % CI) were ± 9.6° around a mean of 0.8°. Taking differences of 3° as significant, seven knees assessed as valgus clinically, appeared varus on radiographs. Three clinically straight knees showed significant varus and one clinically valgus knee was neutral on the radiograph. Mean BMI for the incorrectly assessed knees was 33.7.
Using computer navigation measurements as a baseline, the mean difference of the clinical measurements was 0.3° (range -10.5° to +9°). The Wilcoxon signed ranks test showed no statistical difference between the clinical and computer system measurements (p = 0.626). The Bland Altman limits of agreement were ± 9.4°. Taking differences of 3° as significant, four knees assessed as valgus clinically, measured varus with the navigation system and one knee assessed clinically as varus was measured valgus. Two clinically straight knees showed significant varus and one clinically valgus knee was neutral as measured by the navigation system. Mean BMI for the incorrectly assessed knees was 32.3.
Sagittal assessment
For flexion deformities no radiographic measurements were available so computer navigation measurements were the only baseline. The mean difference from clinical measurements was 1.6° (range +19° to -11.5°). The Wilcoxon signed ranks test showed no statistical difference between the two measurements (p = 0.156). However the Bland Altman limits of agreement were ± 12.6°. When stratified for BMI, the Bland Altman limits of agreement were significantly wider for patients with BMI < 30> 30 (± 8.7° about a mean difference of -0.9°). Taking differences of 3° as significant 31(63%) patients had a different deformity as assessed by the navigation system when compared to the clinical measurements.
Most of the time surgeons record the clinical deformity measurements in the patient notes. This forms a part of pre-operative planning, and post-operatively it becomes an important reference point against which improvement in alignment is compared and is therefore vital in patient evaluation. It may also serve as a legal record in cases of litigation. In our study we found clinical measurement to be an unreliable method of deformity assessment.
Our results show that the error of clinical measurement when compared to either HKA radiographs or computer navigation measurements did not reach statistical significance; however when analyzed further with the Bland Altman method, the limits of agreement were quite wide for both coronal and sagittal measurements.
In the coronal plane, the difference between clinical and radiological measurements could be up to 10° either side in 95% of the cases. Similarly in the sagittal plane, clinical measurements could be off by as much as 12° compared to computer measurement. We feel that such limit of agreement is simply too wide to be safely accepted as a surgical standard. We therefore maintain that clinical measurement is at best an estimate of the true amount of deformity with a very wide margin of error. Within this cohort it showed the varus knee as valgus and vice versa in 13% of patients. It should also be pointed out that the technique that we used in this series was very methodical compared to the usual visual estimate employed in day to day practice which is done without any reference to the hip centre. This undoubtedly has improved the accuracy of our clinical measurement of coronal deformity.
Gallie and co-workers have shown that visual estimation of fixed flexion deformity has a higher mean error compared to navigation using radiographs as standard [20]. Our result showed that clinical measurement of flexion deformity could leave a margin of error as high a 12°.
There was some expectation that increased body mass index would influence error in clinical measurement but we did not demonstrate this in our series. On the contrary the clinical measurements of flexion deformity in patient with body mass index below 30 showed a higher mean error compared to patients with body mass index above 30 when navigation measurements were used as the baseline.
As the two baselines that could be used to check the clinical measurements against do not always agree, it was hard to assess when they were “correct”. There is evidence in the literature to show that radiographic and navigation measurements of knee deformity although well correlate, do not give the same absolute values [21,22].
Human assessment of angles is known to be poor [6,23] and the accuracy of alignment estimates may be variable (±5°) 15. The use of knee radiographs has also been found to be an inaccurate measure of mechanical lower limb alignment [24]. Full-length hip-knee-ankle radiographs are susceptible to limb positioning errors with apparent variations in alignment produced as a result of knee flexion or rotation [25]. Authors claimed weight bearing and collateral ligaments as factors which could account for the differences in measurements between radiographs and computer navigation [22]. Collateral ligament laxity may vary between individuals and has been found to be different in males and females [26]. The knee coronal alignment has been found to be dynamic and changes with posture as was found in a study on normal knees [27,28].
We propose that the discrepancy between radiographic and navigation methods is at least partly explained by the absence of the effect of gravity with navigation when the measurements were taken supine, even though we have tried to simulate this by applying axial load to the foot. It was, of course, necessary to expose the joint sufficiently to gain access to the bony landmarks during navigation. Even though this initial exposure was consistently kept to a minimum, the full effect of this on the actual deformity prior to exposure was impossible to determine. It may well have also contributed to the observed discrepancy between radiographic and computer measurement.
Methodical clinical measurement of knee deformity as described in this paper gives too wide a margin of error and should not be relied upon in isolation. A combination of other modalities like long leg radiographs and computer navigation will add to the assessment, but one should consider the effect of posture on the measurements when assessing the knee deformity.