AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Anthony Kodzo-Grey Venyo, Department of Urology, North Manchester General Hospital, Delaunay’s Road, Crumpsall, Manchester, Lancashire, M8 5RB, United Kingdom.
Citation: Anthony K. G Venyo, (2022). Irreversible Electroporation of Carcinoma of the Prostate Gland with a Focus on Localized Carcinoma of the Prostate Gland: A Review and Update. J Clinical Research and Reports, 10(5); DOI:10.31579/2690-1919/239
Copyright: ©2022. Anthony K. G. Venyo. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 28 February 2022 | Accepted: 16 March 2022 | Published: 28 March 2022
Keywords: adenocarcinoma of prostate; localized; low-risk; intermediate-risk; medium-risk; radical prostatectomy; radical radiotherapy; irreversible electroporation; oncology outcome; functional outcome; serum prostate-specific antigen; prostate biopsy
Even though adenocarcinoma of the prostate gland could be lethal in its advanced stage, adenocarcinoma of the prostate gland can be effectively treated when the carcinoma is localized to the prostate gland and when the localized adenocarcinoma is a low-risk or intermediate-risk localized adenocarcinoma of the prostate gland. it is localized. Traditionally, radical prostatectomy (RP) or radical radiotherapy (RT) in the form of either external beam radiotherapy or brachytherapy were utilized to treat all men who have localized adenocarcinoma of the prostate gland as treatment of curative intent. Nevertheless, Radical prostatectomy and radical radiotherapy do tend to be associated with significant risks of post-treatment side effects. Some patients who have localized prostate cancer may not be medically fit as a result of their comorbidities to undergo radical prostatectomy or radical radiotherapy to their prostate cancers. Over recent years a number of less-invasive treatment options are being utilized for the treatment of some localized adenocarcinomas of the prostate gland and some of the treatment options include: Cryotherapy of prostate Cancer; Radiofrequency ablation of prostate cancer, High Intensity Focused Ultrasound Treatment of Prostate Cancer and Irreversible Electroporation of prostate cancer as focal ablation or whole gland ablation. Focal therapy has emerged as a potential form of treatment that can achieve similar oncological outcomes to radical treatment while preserving functional outcomes and decreasing rates of adverse effects. Irreversible electroporation (IRE) is one such form of focal therapy which utilizes pulsatile electrical currents to ablate tissue. This modality of treatment is still in an early research phase, with studies showing that IRE is a safe procedure that can offer good short-term oncological outcomes whilst carrying a lower risk of poor functional outcomes. Irreversible Electroporation (IRE) is a new radiology image-guided tissue ablation which does induce cell death through very short but strong electric fields. IRE had been demonstrated to have preserving properties towards vessels, nerves, as well as the extra-cellular matrix. For this reason, IRE could represent an ideal treatment option for adenocarcinoma where other treatment options including radical prostatectomy and radical radiotherapy tend to unselectively destroy that encompass the prostate cancer and inducing side effects including urinary incontinence as well as sexual dysfunction / impotence. Some results of studies in which IRE had been utilized for the treatment of curative intent of localized low-risk and intermediate-risk adenocarcinomas of the prostate gland had indicated complete efficacy of IRE to the standard of radical prostatectomy and standard radical radiotherapy with regard to the 5-year tumour recurrence rate as well as better preservation of genitourinary function which did prove the safety as well as suitability of IRE for the treatment of localized low-risk and intermediate risk adenocarcinoma of the prostate gland. Some data pertaining to IRE besides focal treatment of early adenocarcinoma of the prostate gland had shown that IRE besides focal treatment of early prostate cancer could also be utilized for whole prostate gland ablations in patients who develop recurrent prostate cancer as well as a problem-solving treatment for the control of local tumour within the prostate gland that are not amenable to surgery or radiotherapy anymore. Some studies had demonstrated comparable short-term and medium-term functional outcomes functional outcomes with radical prostatectomy and radical radiotherapy but following longer surveillance assessments those underwent IRE were found tom have superior genitourinary function in that a number of the sexual dysfunction and urinary incontinence had resolved but with regard to the oncology outcome repeat follow-up biopsy of the prostate had demonstrated a higher positive tumour biopsy upon pathology examination for which either further IRE, or radical radiotherapy, or radical prostatectomy was required as subsequent treatment of curative intent in that radical prostatectomy of curative intent had superior medium-term to long-term outcome in comparison with IRE. IRE can also be utilized to treat locally recurrent prostate cancer following: (a) radical radiotherapy and (b) following the finding of persistent or locally recurrent adenocarcinoma of the prostate gland pursuant the undertaking of IRE as treatment of curative intent of localized adenocarcinoma of the prostate gland. Following failure of IRE treatment for localized adenocarcinoma of the prostate, the persistent carcinoma of the prostate gland could also be treated by means of radical prostatectomy, or radical radiotherapy or any other minimally invasive treatment of curative intent including cryotherapy, radiofrequency ablation of the prostate and high intensity focused ultrasound treatment. Considering that IRE tends to be associated with good short-term and medium-term outcome which also tends to be generally superior to the outcome following radiotherapy as well as radical prostatectomy, and the fact that the medium-term to long-term oncology outcome tends to be good but the oncology outcome following radical prostatectomy as well as radiotherapy would tend to be a bit superior to IRE, it could be suggested that patients who have low-risk and intermediate-risk localized adenocarcinoma who prefer to maintain their genitourinary function could be offered IRE as first line treatment of curative intent which should be followed up with regular frequent assessments which would enable early identification of treatment failures at an early stage. The individuals who are found to have IRE failure could then be offered radical prostatectomy or radical radiotherapy as second line treatment of curative intent. Finally, there is need for a global multi-centre trial of IRE in the treatment of curative intent of localized low-risk, intermediate-risk, as well as high risk groups and those who have high risk group localized prostate cancer could be offered adjuvant therapy and all these treatments should be compared with radical radiotherapy and radical prostatectomy with a long period of follow-up to enable a consensus opinion to be established as well as guidelines to be formulated.
Carcinoma of the prostate gland can be localized carcinoma of the prostate gland, locally advanced carcinoma of the prostate gland or metastatic carcinoma of the prostate gland. It has been iterated that carcinoma of the prostate gland has continued to be one of the commonest diagnosed carcinomas in men as well as a leading cause of cancer deaths in men globally [1,2]. It has also been documented that even though carcinoma of the prostate gland could be lethal in its advanced stage, carcinoma of the prostate gland could be treated effectively when it is localized to the prostate gland [1]. Traditionally radical prostatectomy (RP) or radical radiotherapy (RT) either in the form of external beam radiotherapy or brachytherapy were utilized for the treatment of all men who have localized prostate cancer, irrespective of their risk [1]. Nevertheless, notwithstanding their improved survival benefits, radical prostatectomy (RP) and radical radiotherapy (RP) have tended to be associated significant risks of post-treatment side effects / complications and the two commonest of these complications tend to include urinary incontinence (UI) and erectile dysfunction (ED). [ong 0000]. It has been iterated that over the preceding decade, a change in the treatment of very low-risk as well as low-risk adenocarcinoma of the prostate gland, as well as an increasing interest in new techniques for the treatment of intermediate-risk localized adenocarcinoma of the prostate gland has emerged [1]. it has also been iterated that very low-risk and low-risk adenocarcinoma of the prostate gland does tend to be associated with an unlikely chance of developing metastasis as well as a very low-risk of mortality [2]. In view of the aforementioned facts, new guidelines, do now recommend treatment of such very low-risk group and low-risk groups of localized prostate cancer by means of active surveillance to delay or mitigate the need to undertake radical prostatectomy (RP) or radical radiotherapy [1,3]. Likewise, it has been iterated that some evidence had indicated that intermediate-risk group of localized-adenocarcinoma of the prostate gland tend to be associated with oncology outcomes that are close to the oncology outcomes of low-risk localized adenocarcinoma of the prostate gland [1,4]. Nevertheless, the risk for the development is stated to be still relevant and does warrant some form of therapy [1]. It has been documented those different types of focal therapy to the prostate gland are currently being utilized on trial basis for these men [1].
It has been explained that by focusing treatment upon a specific area of the prostate gland, the aim of focal treatment is to achieve similar oncology outcomes to radical treatment while preserving functional outcomes as well as decreasing the rates of adverse effects [1]. Irreversible electroporation (IRE) is a new focal therapy option which utilizes pulsatile electrical currents to ablate tissue. Animal and human models had been utilized to confirm that IRE could induce cell death but at the same time preserving important encompassing structures [5].
The mechanism in which IRE does this is said to be via the destabilization of the cell membrane, which then causes the alteration of membrane shape and the formation of nanopores. It has been iterated that the excessive permeability of these cells does tend to disrupt the osmotic balance, and this leads to irreversible damage and the process of apoptosis [1,6]. It has been documented that the IRE technique has now been refined in order to administer electrical pulses at levels to prompt cell death whilst keeping the procedure below harmful thermal thresholds [1,5]. It has been pointed out that with regard to important structures such as blood vessels, IRE has been demonstrated to decrease smooth muscle cells but maintain the connective tissue matrix [1,7]. Hence, it has been utilized effectively within liver lesions where damage to bile ducts and hepatic vessels are lethal [1,8,9]. It has been pointed out that with regard to men who have adenocarcinoma of the prostate gland, preservation of the neurovascular bundles adjacent to the gland could emanate in the preservation of continence and erectile function, which would therefore increase or improve the quality of life of the patient [1].
It has been pointed out that initial trials for localized adenocarcinoma of prostate gland patients had demonstrated promising results with regard to both oncology and functional outcomes; nevertheless, more information on the clinical performance of IRE is required before clinicians could integrate IRE into their routine clinical practice [1]. Even though IRE is being utilized in some research and academic centers within many developed countries, it would be envisaged that many clinicians globally may not be familiar with utilization of IRE in the treatment of many lesions within the body including localized adenocarcinoma of the prostate gland. Considering that IRE has only be utilized in the treatment of prostate cancer, it would be envisaged that perhaps the short-term and perhaps the intermediate-term outcome of IRE for the treatment of prostate cancer would be known and the long-term outcome of IRE in the treatment localized adenocarcinoma would not be known yet. Before a consensus is made globally regarding the utilization as well as timing and indications for utilizing prostate cancer is made it would be important to summate the outcome of IRE in the treatment of carcinomas of the prostate gland that have been reported in various journals in order to be sure about the outcome of treatment of prostate cancer with IRE. The ensuing article of IRE in the treatment of prostate cancer is divided into three parts: (A) Overview that has defined Irreversible electroporation as well as described various lesions of the body that have been treated by IRE, (B) Miscellaneous Narrations and Discussions Related to Utilization of IRE in Research Work Focusing on Animal Studies And (C) Utilization of Irreversible Electroporation OF Prostate Cancer IN Human Beings and In Few Animals.
To Review and Update the Literature on Irreversible Electroporation in The Treatment of Various Lesions of The BODY In General and with a Focus of Localized Adenocarcinoma of the Prostate Gland.
Various Internet data bases were searched including: Google; Google Scholar; Yahoo; and PUBMED. The search words that were used included: Irreversible Electroporation; Irreversible Electroporation of Prostate Cancer; Irreversible Electroporation of Adenocarcinoma of Prostate; Irreversible Electroporation of Carcinoma of Prostate; Irreversible Electroporation of Localized Prostate Cancer. One hundred and six (106) references were identified which were used to write the review and update of the literature on Irreversible Electroporation in General And Irreversible Electroporation of Prostate Cancer which has been divided into three parts: (A) Overview that has defined Irreversible electroporation as well as described various lesions of the body that have been treated by IRE, (B) Miscellaneous Narrations And Discussions Related to Utilization of IRE in Research Work Focusing On Animal Studies And (C) Utilization of Irreversible Electroporation OF Prostate Cancer IN Human Beings and In Few Animals.
Overview
Definition / general statements
Irreversible electroporation (IRE) is a terminology that is utilized for soft tissue ablation technique which utilizes short but strong electrical fields in order to create permanent and thus lethal nanopores within the cell membrane, and to disrupt cellular homeostasis [10]. The resulting cell death does emanate from induced apoptosis or necrosis which has been induced by either membrane disruption or secondary breakdown of the membrane as an emanation of transmembrane transfer of electrolytes and adenosine triphosphate [10,14]. It has been stated that the main utilization of IRE does lie upon tumour ablation within regions where precision and conservation of the extracellular matrix, blood flow and nerves are of importance [10]. The first generation of IRE for clinical utilization, in the form of the NanoKnife System, became commercially available for research purposes in 2009, and this was mainly for the surgical ablation of soft tissue tumours [10,15].
It has additionally been iterated that ablation of cancerous tissue ablation by means of IRE does appear to demonstrate significant cancer specific immunological responses that are currently being evaluated alone and in combination with cancer immunotherapy [10,16-19].
History
With regard to the history of Irreversible electroporation (IRE). It has been iterated that the first observations of the effects of IRE was reported in 1898. [10] [20] Nollet did report the first systematic observations of the appearance of red spots upon animal and human skin that had been exposed to electric sparks [10, 21]. Nevertheless, the use of IRE for modern medicine did begin in 1982 with the seminal work of Neumann and colleagues. [10] [22] Pulsed electric fields were utilized to temporarily permeabilize cell membranes in order to deliver foreign DNA into cells. Within the ensuing decade, the combination of high-voltage pulsed electric fields with the chemotherapeutic drug bleomycin and with DNA had yielded new clinical applications including: electrochemotherapy as well as gene electro-transfer. [10,23-27] It has been iterated that utilization of irreversible electroporation (IRE) for therapeutic purposes was first suggested by Davalos, Mit, as well as Rubinsky [10] [28].
[A] Mechanism of Irreversible electroporation
Irreversible electroporation is said to utilize ultra-short pulsed but very strong electrical fields, micropores and nanopores are induced in the phospholipid bilayers which form the outer cell membranes. [10] It has been iterated those two types of damage can occur following irreversible electroporation and these include: [10]
It has been iterated that that even though the ablation method is generally accepted to be apoptosis, some findings seem to contradict a pure apoptotic cell death, which has made the exact process by which IRE causes cell death unclear [10,14,29] Nevertheless, all studies do agree that the cell death is an induced cell death in which the cells dying over a varying time period of hours to days and does not rely on local extreme heating and melting of tissue by means of high energy deposition like most ablation technologies [10].
When an electrical field of greater than 0.5 V/nm [30] is applied to the resting trans-membrane potential, it has been promulgated that water does enter the cell during this dielectric breakdown. Hydrophilic pores tend to be formed. [31,32] It has been iterated that a molecular dynamics simulation by Tarek [33] had demonstrated this proposed pore formation in two steps as follows: [34]
It has been postulated that as the applied electrical field increases, the greater is the perturbation of the phospholipid head groups, which in turn increases the number of water- filled pores [10,35]. It has been documented the entire electroporation process could occur within a few nanoseconds. [10,33] It has been iterated that the average sizes of nanopores are likely cell-type specific. In swine livers, they average around 340-360 nm, as found using SEM [10,34]. A secondary promulgated mode of cell death was postulated to be from a breakdown of the membrane ensuing transmembrane transfer of electrolytes and adenosine triphosphate [10,13]. Other effects like heat [10,36] or electrolysis [10,37,38] were also demonstrated to play a pivotal role with regard to the currently clinically applied IRE pulse protocols.
Potential Advantages and Disadvantages of Irreversible Electroporation (IRE)
Advantages of Irreversible Electroporation (IRE) Some of the advantages of IRE have been summates as the ensuing: [10]
Disadvantages of Irreversible Electroporation (IRE)
Strong muscle contractions – It has been documented that the strong electric fields that are created by Irreversible Electroporation (IRE), due to the direct stimulation of the neuromuscular junction, do cause strong muscle contractions that require special anesthesia and paralysis of the entire body [10,43].
Utilization of Irreversible Electroporation in Medical Practice
A number of electrodes, in the form of long needles, tend to be placed encompassing the target volume. The point of penetration for the electrodes is chosen based upon the anatomical conditions [10]. Radiology imaging is important for the placement and this could be achieved by means of ultrasound scan, magnetic resonance imaging (MRI) scan or computed tomography (CT) scan [10]. The needles are then connected to the Irreversible Electroporation (IRE)-generator, which then does proceed to sequentially build up a potential difference between two electrodes. The geometry of the Irreversible Electroporation (IRE)-treatment field tends to be calculated in real time and it could be influenced by the user [10]. Depending upon the treatment-field and the number of electrodes that are utilized, the ablation tends to take between 1 minute and 10 minutes [10]. In general muscle relaxants tend to be administered, in view of the fact that even under general anesthesia, strong muscle contractions tend to be induced by excitation of the motor end-plate [10].
Typical parameters (1st generation IRE system):
The ensuing summations have been made regarding the typical parameters of 1st generation irreversible electroporation (IRE) system: [10]
It has been iterated that the shortly pulsed, strong electrical fields tend to be induced via thin, sterile, disposable electrodes. [Wikipedia 10] The potential differences tend to be calculated as well as applied through a computer system between these electrodes in accordance to a previously planned treatment field [10].
One specific device that is utilized for the Irreversible Electroporation (IRE) procedure is the NanoKnife system which was manufactured by AngioDynamics, that received FDA 510k clearance on October 24, 2011 [48].
The NanoKnife system did also receive an Investigational Device Exemption (IDE) from the FDA which enables AngioDynamics to conduct clinical trials utilizing this device [48]. The Nanoknife system is said to transmit a low-energy direct current from a generator to electrode probes that inserted/placed within the target tissues for the surgical ablation of soft tissue [10]. It has been stated that in 2011, AngioDynamics apparently did receive an FDA warning letter for promoting the device for indications for which it had not received approval [10,49].
It has also been documented that in 2013, the United Kingdom National Institute for Health and Clinical Excellence (NICE) had issued a guidance that the safety and efficacy of utilization of irreversible electroporation (IRE) of the treatment of various types of cancer had not yet been established [10,50]. Current evidence related to the safety and efficacy of irreversible electroporation for treating primary lung cancer and metastases in the lung is inadequate in quantity and quality. Therefore, this procedure should only be used in the context of research.
It has been iterated that newer generations of Electroporation-based ablation systems are being developed specifically in order to address the shortcomings of the first generation of Irreversible Electroporation (IRE); however, as of June 2020, none of the technologies were available as a medical device to be utilized [10,38,51,52].
It has been iterated that potential organ systems, in which Irreversible Electroporation (IRE) could be of significant impact due to its properties include: the pancreas, the liver, the prostate gland.
Hepatic (liver) irreversible electroporation (IRE) is stated to appear to be safe, even when performed near vessels and bile ducts [10,53,54] with an overall complication rate of 16%, with majority of the complications being needle related (pneumothorax and hemorrhage). The COLDFIRE-2 trial which included 50 patients did show 76% local tumour progression-free survival after 1 year of follow-up [55]. However; no studies had been undertaken which hade compared Irreversible Electroporation (IRE) to other ablative treatment options; nevertheless; thermal ablations procedures had been reported to be associated with a higher efficacy in that matter with about 96% progression free survival. In view of this, Geboers et al. [45] did conclude that Irreversible Electroporation (IRE) should at the moment only be performed for only truly unresectable and tumours that are considered to be non-ablatable. It has been documented that the overall survival rates in studies related to utilization Irreversible Electroporation (IRE) for cancer of the pancreas do provide an encouraging non-variable end-point and do show an additive beneficial effect of Irreversible Electroporation (IRE) in comparison with the standard-of care chemotherapeutic treatment with FOLFIRINOX which entailed a combination of 5-fluorouracil, leucovorin, irinotecan, and oxaliplatin) (median OS, 12–14months) [56,57]. Nevertheless; Irreversible Electroporation (IRE) does appear to be more effective in conjunction with systemic therapy and it has not been suggested as first-line treatment option of choice [58]. It has additionally been iterated that even though Irreversible Electroporation (IRE) does make adjuvant tumour mass reduction treatment for LAPC possible for the first time, IRE does remain, in its current state, a high risk and high side effect associated treatment procedure which is justified only due to the high mortality and the lack of alternative treatments [10].
Prostate
It has been iterated that the concept of treating carcinoma of the prostate gland with utilization of Irreversible Electroporation (IRE) was first promulgated by Gary Onik and Boris Rubinsky in 2007 [10,59]. It has been iterated that Carcinomas of the prostate gland tend to be frequently found near sensitive structures which might be permanently damaged by thermal treatments or radiotherapy [10]. With regard to carcinomas of the prostate gland, it has been iterated that the applicability of surgical treatment methods has often been limited by accessibility and precision [10]. It has also been stated that surgery also tends to be associated with a long period of healing time and a high rate of side effects. [10,60].
It had been conjectured that with utilization of Irreversible Electroporation (IRE), the urethra, bladder, rectum and neurovascular bundle and lower urinary sphincter could potentially be included within the treatment field without creating permanent-damage [10].
It has been pointed out that Irreversible Electroporation (IRE) has been utilized for the treatment of carcinoma of the prostate gland since 2011, and that IRE treatment of carcinoma of the prostate gland has partly in been in the form of clinical trials, compassionate care or individualized treatment approach. [10] It has additionally been pointed out that like for all other ablation treatment options, and also most conventional methods of treatment of prostate cancer, no studies had utilized a randomized multi-centre approach or targeted cancer-specific mortality as end-point [10]. Other summating iterations that had been made regarding treatment of carcinoma including the use of IRE include the following:
that was associated with up to 6-year follow-up has been limited as a heterogeneous retrospective analysis and no prospective clinical trial, was undertaken.
IRE for carcinoma of the prostate gland is at the moment not recommended in treatment guidelines [10].
Kidney
While nephron-sparing surgery has been regarded as the gold standard treatment option for small, malignant renal masses, ablative treatment options are also regarded as viable options in patients who have been assessed and found to be poor surgical candidates to undergo nephron-sparing surgery. Radiofrequency ablation (RFA) of kidney lesions and cryoablation of kidney lesions have been utilized since the 1990s; nevertheless, in lesions that are found to be larger than 3 cm, the efficacy of RFA and cryotherapy of kidney lesions is said to be limited [10]. It has been iterated that the newer ablation options of treatment including: IRE, microwave ablation (MWA), as well as high-intensity focused ultrasound, could help overcome the challenges related to the size of the kidney tumour [10,63].
It has been stated that the first human studies that had been undertaken had proven the safety of IRE for the ablation of kidney masses; nevertheless, the effectiveness of IRE based upon histopathology examination features of an ablated kidney tumour in human beings is yet to be known or confirmed [10]. Wagstaff and associates., had set out to investigate the safety and effectiveness of IRE ablation of kidney tumour masses and to evaluate the efficacy of ablation with utilization of MIR and contrast-enhanced ultrasound imaging. It has been pointed out that in accordance with the prospective protocol that was designed by the authors, the treated patients would later on undergo radical nephrectomy in order to assess the success of IRE ablation [64]. It has been pointed out that later phase 2 prospective trials had demonstrated good results in terms of safety and feasibility [64,65] for small kidney tumour masses but the cohort was limited in numbers and these cohorts had included 7 patients and 10 patients respectively; In view of this, it has been iterated that the efficacy of IRE had not yet been established sufficiently [10]. It has additionally been stated that IRE does appear to be safe for small kidney masses that measure up to 4 cm [10]. Nevertheless; the consensus opinion is that current evidence on utilization of IRE to treat kidney tumour masses is still not adequate in quality and quantity for a consensus opinion to be established regarding the safety and efficacy of utilizing IRE to treat kidney tumour masses [45].
Lung
It has been iterated that in a prospective, single-arm, multi-centre, phase II clinical trial, the safety and efficacy of IRE upon lung cancers had been evaluated and that the trial had included patients who had primary and secondary lung malignancies as well as preserved pulmonary (lung) functions. It was reported that the expected effectiveness of IRE in the treatment of malignancies of the lung had not been met during interim analysis of the results and the trial had been stopped prematurely. It was also reported that the complications of IRE of the lung had included: pneumothorax in 11 out of 23 patients, alveolar hemorrhage not resulting in significant haemoptysis, and needle tract seeding was found in 3 cases that amounted to 13% of the cases. Disease progression was noticed in 14 out of the 23 patients that amounted to 61% of the patients. Stable disease was observed in 1 patient which amounted 4% of the patients, partial remission of the tumour was observed in 1 patient which amounted to 4% of the patients and complete remission was found in 7 patients which amounted to 30% of the patients. The authors did conclude that IRE is not effective for the treatment of lung cancers/malignancies [66].
Likewise, some authors reported that they had found similarly poor treatment outcomes in their studies [67,68].
It has been pointed out that a major obstacle of IRE in the treatment of lung lesions is the difficulty in positioning of the electrodes; placing the probes in parallel alignment is made challenging by the interposition of ribs. Furthermore, the planned and actual ablation zones within the lung tend to be dramatically different because of the differences in conductivity between the tumour, lung parenchyma, as well as air [10,69].
Coronary arteries
It has been iterated that Maor and associates had illustrated the safety and efficiency of IRE as an ablation option of treatment for smooth muscle cells within the walls of large vessels in rat model [70].
In view of this IRE has been postulated as representing a preventive treatment for coronary artery re-stenosis pursuant to percutaneous coronary intervention procedure [10].
Pulmonary veins
It has been pointed out that many studies on animals had illustrated the safety and efficiency of IRE as a non-thermal ablation option of treatment for pulmonary veins with regard to the treatment of atrial fibrillation [10]. The advantages of IREs’ in comparison with radiofrequency ablation (RFA) and cryoablation do include: Well defined ablation area and the lack of peripheral thermal damage. In view of this, IRE has been promulgated as a part of novel option of treatment for atrial fibrillation (AF) [10,71].
Other organs
It has furthermore been iterated that IRE had also been investigated within ex-vivo human eye models for the treatment of uveal melanoma [10,72], as well as in thyroid cancer [10,73].
It has been pointed out that successful IRE ablations in animal tumour models had been undertaken for lung, [10,74,75] brain, [10,74,76,77], heart, [10,78] skin, [10,79,80] bone, [10,81,82] head and neck cancer [10,83], as well as blood vessels. [10,84]
[B] Miscellaneous studies on Irreversible electroporation of various organs in animals
Rubinsky et al. [11] made the following summations related irreversible electroporation:
Rubinsky et al. [11] undertook a study which was aimed to study their IRE tissue ablation methodology in the pig liver, to provide first experience results on long term histopathology of IRE ablated tissue, as well as to discuss the clinical implications of the findings. The study consisted of the following: a) the designing of an IRE ablation protocol via a mathematical analysis of the electrical field during electroporation; b) utilization of ultrasound scan to position the electroporation electrodes within the predetermined locations and subsequently to monitor the process; c) application of the predetermined electroporation pulses; d) the undertaking of histopathology examination on the IRE treated samples for up to two weeks pursuant to the procedure; and e) correlation of the mathematical analysis, ultrasound scan data, and histology. Rubinsky et al. [11] observed that electroporation does affect tissue in a way that could be imaged in real time with ultrasound scan, which should facilitate real time control of the electroporation during clinical applications. Rubinsky et al. [11] observed cell ablation to the margin of the treated lesion with several cells thickness resolution. There did appear to be complete ablation to the margin of blood vessels without compromising the functionality of the blood vessels, which had indicated that IRE is a promising method for the treatment of tumours that are near blood vessels which has been a significant challenge with current ablation methods. Consistent with the mechanism of action of IRE on the cell membrane only, Rubinsky et al. [11] demonstrated that the structure of bile ducts, blood vessels, and connective tissues had remained intact with IRE. Rubinsky et al. [11] stated the following:
Au et al. [85] stated that Irreversible electroporation (IRE) is a new ablation technique which tends to induce permanent membrane permeability and cell death and that they were interested in ultrasound B-mode and elastography in order to monitor IRE ablation within the liver. With regard to methods, Au et al. [85] reported that Yorkshire pigs had undergone IRE ablation of the liver and they were imaged with ultrasound B-mode and elastography. Histopathology evaluation of cell death by triphenyltetrazolium chloride and haematoxylin and eosin staining was undertaken. Au et al. [85] summarized the results as follows:
Au et al. [85] made the following conclusions:
Lee et al. [86] evaluated the effectiveness of irreversible electroporation (IRE) in hepatic (liver) tissue ablation and the radiology-pathology correlation of IRE-induced cell death. With regard to the materials and methods of their study, Lee et al. [86] reported that pursuant to an approval of the animal research committee, 16 Yorkshire pigs had undergone ultrasonography (US)-guided IRE of normal liver. A total of 55 ablation zones were created, that were imaged with US, magnetic resonance (MR) imaging, and computed tomography (CT) and evaluated with immunohistochemical analysis of the tissues were undertaken, including haematoxylin-eosin (H-E), Von Kossa, and von Willibrand factor (vWF) staining as well as terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay. Lee et aal. [86] summarized the results as follows:
Lee et al. [86] made the ensuing conclusions:
Duuki-Jacobs et al. [87] stated that Irreversible electroporation (IRE) is a new technique for tumour cell ablation which had been reported to involve non-thermal-based energy utilizing high voltage at short microsecond pulse lengths. They also stated that In vivo assessment of the thermal energy generated during IRE had not been undertaken and that Thermal injury could be predicted utilizing a critical temperature model. The aim of their study was to assess the potential for thermal injury during IRE in an in vivo porcine model. With regard to the methods, Duuki-Jacobs et al. [87] reported the following: In vivo continuous temperature assessments of 86 different IRE procedures were undertaken on porcine liver, pancreas, kidney and retroperitoneal tissue. They measured issue temperature continuously throughout IRE procedure by means of two thermocouples that were placed at set distances of 0·5 cm or less, and 1 cm from the IRE probes within the treatment field. They defined thermal injury as a tissue temperature of 54°C that lasted at least 10 seconds. They evaluated tissue type, pulse length, probe exposure length, number of probes and retreatment for associations with thermal injury. Additionally, IRE ablation was undertaken with metal clips or metal stents in the ablation field in order to determine their effect upon thermal injury. Duuki-Jacobs et al. [87] summarized the results as follows:
Duuki-Jacobs et al. [87] made the following conclusions:
Sugimoto et al. [88] undertook a study to assess various ultrasound (US) scan findings, including B-mode, shear-wave elastography (SWE), and contrast-enhanced US, in accurately assessing ablation margins pursuant to irreversible electroporation (IRE) based upon radiology-pathology examination feature correlation, and to compare these findings between IRE and radiofrequency (RF) ablation. With regard to the materials and methods of their study, Sugimoto et al. [88] reported that IRE was undertaken on nine (9) and radiofrequency ablation (RF ablation) on three (3) in vivo in three pig livers. Each ablation zone was imaged radiologically by each method immediately after the procedure and 90 minutes subsequently. They evaluated the ablation zones based upon gross pathological and histopathology findings within samples that were obtained from the animals that were euthanized 2 hours pursuant to the last ablation. They compared the characteristics and dimensions of the histologically ablation zones were qualitatively and quantitatively against each US finding. Sugimoto et al. [88] summarized the results as follows:
Sugimoto et al. [88] concluded that RE and RF ablation zones could be most accurately predicted by portal-phase contrast-enhanced US measurements which has been obtained immediately after the ablation.
Appelbaum et al. [89] undertook a study in order to characterize ultrasonographic (US) findings pursuant to irreversible electroporation (IRE) in order to determine the utility of these findings in the accurate assessment of ablation margins. With regard to the materials and methods of their study, Sugimoto et al. [89] stated the following: Their institutional animal care and use committee approval of the study was obtained. IRE ablation totalling 58) was performed in vivo in 16 pig livers by utilizing two 18-gauge electroporation electrodes with 2-cm tip exposure, 1.5- or 2.0-cm interelectrode spacing, and an electroporation generator. Energy deposition was applied at 2250-3000 V (pulse length, 50-100 μsec; pulse repetition, 50-100). Ablations were undertaken under the guidance of ultrasound (US) scan. Images had been obtained during ablation and at defined intervals from 1 minute to 2 hours pursuant to the procedure. Zones of ablation were examined during Macroscopic and histopathology examination of samples that had been obtained from the animals which had been sacrificed 2 hours to 3 hours following the IRE procedures. The dimensions of the histopathology necrosis zone and ultrasound (US) findings were compared and subjected to statistical analysis, with the inclusion of a “Student” t-test and multiple linear regression.
Appelbaum et al. [89] summarized the results as follows:
Appelbaum et al. [89] made the following conclusions:
Appelbaum et al. [90] undertook a study to prospectively ascertain the optimal parameters with which to achieve defined large target zones of coagulation by utilizing irreversible electroporation (IRE) with four-electrode arrays and the time that is needed to achieve this treatment effect in an in vivo animal model. With regard to the materials and methods, Appelbaum et al. [90] reported the following:
Appelbaum et al. [90] summarized the results as follows:
Appelbaum et al. [90] made the ensuing conclusions:
Faroja et al. [91] undertook a study in order to ascertain whether high-dose irreversible electroporation (IRE) ablation does induce thermal effects in normal liver tissue. With regard to materials and methods, Faroja et al. [91] stated the following: They had obtained animal care and use committee approval was preceding their experiments. IRE ablation that totalled 78 was undertaken by a single four-person team in vivo in 22 porcine livers by through the application of electric current to two 1.3-cm-diameter circular flat-plate electrodes that were spaced 1 cm apart. Cardiac-gated IRE pulses that ranged between 40 and 360 were systematically applied at varying voltages betwenn1500 volts and 2900 volts. They measured End temperatures at the ablation zone centre which were correlated with ablation time, energy parameters, and resultant treatment effect as was determined at macroscopic (gross) pathology and histopathology examination. Faroja et al. [91] then monitored temperatures at the centre as well as the periphery of four ablations that were created by the use of a four-electrode IRE array (3000 V, 90 pulses per electrode pair). Faroja et al. [91] analysed the data by utilising multivariate analysis of variance with multiple comparisons and/or paired t tests and regression analysis, as appropriate. Faroja et al. [91] summarised the results as follows:
Faroja et al. [91] made the ensuing conclusions:
Wagstaff et al. [92] stated that even though tissue ablation by irreversible electroporation (IRE) had been characterized as nonthermal, the application of frequent repetitive high-intensity electric pulses does have the potential of substantially heating the targeted tissue and causing thermal damage. Wagstaff et al. [92] undertook a study to evaluate the risk of possible thermal damage by measuring temperature development and distribution during IRE of porcine kidney tissue. With regard to the methods of the study, Wagstaff et al. [92] stated the following: The animal procedures were conducted after obtaining an approved Institutional Animal Ethics Committee protocol. IRE ablation was undertaken in 8 porcine kidneys. Out of them, 4 kidneys were treated with the use of a 3-needle configuration and the remaining 4 were treated with a 4-needle configuration. All IRE ablations had consisted of 70 pulses with a length 90 µs. The pulse frequency was set at 90 pulses/min, and the pulse intensity at 1,500 V/cm with a spacing of 15 mm between the needles. They measured the temperature internally utilising 4 fiber-optic temperature probes and at the surface by using a thermal camera. Wagstaff et al. [92] summarised the results of the study as follows:
Wagstaff et al. [92] made the following conclusions:
Agnass et al. [93] undertook a study which was aimed first to ascertain whether irreversible electroporation (IRE) is associated with heat generation in the liver and pancreas at clinical (≤1,500 V/cm) and supra-clinical (>1,500 V/cm) electroporation settings; second, and secondly to assess the risk of thermal tissue damage within and adjacent to the treated volume in highly perfused versus moderately perfused parts of both organs; as well as thirdly, to investigate the influence of perfusion and of the presence and the orientation of a metal stent on the maximal thermal elevation (ΔTSession,max) within the tissue during an IRE session at fixed IRE settings, and finally, to ascertain whether the maximum temperature elevation within the IRE-subjected organ during an IRE treatment (single or multiple sessions) is reflected in the organ's surface temperature. With regard to the methods of the study, Agnass et al. [93] stated the following: The aims had been investigated in 12 case studies which were undertaken in five female Landrace pigs. Many IRE settings had been applied for lateral (2), triangular (3), and rectangular (4) electrode configurations within the liver hilum, liver periphery, pancreas head, and pancreas tail. IRE series of 10-90 pulses had been applied with pulse durations which had varied from 70 μs to 90 μs and electric field strengths between 1,200 V/cm and 3,000 V/cm. In select cases, a metal stent was positioned in the bile duct at the level of the liver hilum. They measured temperatures before, during, and following the IRE in and adjacent to the treatment volumes using fibre optical temperature probes (temperature at the nucleation centres) and digital thermography (surface temperature). They assumed the occurrence of thermal damage to be at temperatures above 50 °C (ΔTSession,max ≥ 13 °C relative to body temperature of 37 °C). They compared the temperature fluctuations at the organ surface (ΔTLocSurf) to the maximum temperature elevation during an IRE treatment procedure in the electroporation zone. In select cases, they applied IRE to tissue volumes surrounding the portal vein (PV) and a constricted and patent superior mesenteric vein (SMV) in order to ascertain the influence of the heatsink effect of PV and SMV on ΔTSession,max. Agnass et al. [93] summarised the results as follows:
Agnass et al. [93] advised that appropriate IRE settings should be chosen based upon the tissue type and the presence of stents in order to avoid thermal damage within healthy peritumoral tissue and in order to protect anatomical structures. Agnass et al. [93] made the ensuing conclusions:
[C] Miscellaneous Narrations and Discussions Related to Some Case Reports, Case Series, And Studies Related to Irreversible Electroporation of Prostate Cancer.
Dong et al. [94] undertook clinical trials after they had obtained patients’ consent and approval from the Shanghai Changhai Hospital Ethics Committee (CHEC2017-075) and Good Clinical Practices. Dong et al. [94] reported that forty patients had received therapeutic HF bipolar pulses, and their ages had ranged between 51 years and 85 years. The patients underwent treatment within Shanghai Changhai Hospital in Shanghai, China. Significantly elevated serum prostate-specific antigen level was detected in patients, and the patients then underwent multiparametric MRI to identify the suspected tumours within their prostate glands; the maximum size of the tumour in all of the patients ranged between 1 cm and 3 cm. The patients’ treatment information has been illustrated in Table 1. A prostate needle biopsy was undertaken preceding the IRE procedure in order to illustrate the clinical significance of prostate cancer through histopathology examination of the specimens.
| No | Number of Electrodes | Maximum Size of Tumour, cm | Number of Patients | Patients Age | Treatment Time, min |
|---|---|---|---|---|---|
| 1 | 2 | <1> | 3 | 64, 76, 79 | <8> |
| 2 | 3 | 1.0-1.5 | 13 | 81, 71, 59, 71, 82, 74, 69, 59, 79, 67, 51, 58, 63 | <20> |
| 3 | 4 | 1.5-2.0 | 10 | 76, 68, 73, 57, 65, 81, 84, 85, 73, 78 | <30> |
| 4 | 5 | 2.0-2.5 | 8 | 68, 51, 65, 74, 68, 76, 82, 75 | <40> |
| 5 | 6 | 2.5-3.0 | 6 | 75, 66, 75, 64, 72, 77 | <45> |
Table 1: The Patients Treatment Information
Reproduced from: [94] Dong S, Wang H, Zhao Y, Sun Y, Yao C. First Human Trial of High-Frequency Irreversible Electroporation Therapy for Prostate Cancer. Technol Cancer Res. Treat. 2018 July 25; 17: 1533033918789692 PMCID: PMC6071159 PMID: 30045668 Doi: 10.1177/1533033818789692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6071159/
Copyright © The Author(s) 2018. This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Therapeutic Equipment
A composite steep pulse therapeutic apparatus was utilized in order to generate HF bipolar pulses, as illustrated in Figure 1A. The apparatus could produce bursts of HF bipolar pulses, constituting of individual pulses of duration which had ranged between 1 micro-seconds and 100 microseconds; the inter-burst delay was 1 second, and the rise time was less than 100 nanoseconds. The schematic of bipolar HF pulse bursts applied in the study has been illustrated in Figure 1B.
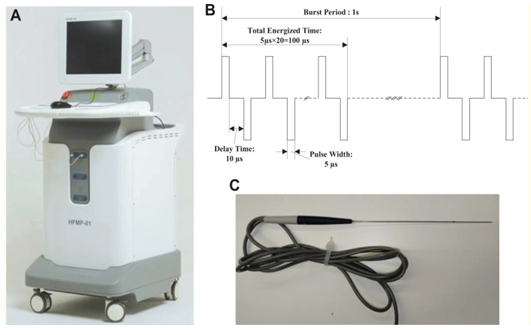
Reproduced from: [94] Dong S, Wang H, Zhao Y, Sun Y, Yao C. First Human Trial of High-Frequency Irreversible Electroporation Therapy for Prostate Cancer. Technol Cancer Res. Treat. 2018 July 25; 17: 1533033918789692 PMCID: PMC6071159 PMID: 30045668 doi: 10.1177/1533033818789692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6071159/
Copyright © The Author(s) 2018
This article is distributed under the terms of the Creative Commons Attribution-Noncommercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
In each trial, 2 to 6 needle electrodes had been inserted into the tumour region, and the distance between 2 electrodes was less than 2 cm. The diameter of the electrodes was 1 mm, and the exposure length was set to 1.0 to 3.0 cm (see figure 1B), depending upon the size of the tumour.
The Procedure
The patients were positioned in the dorsal lithotomy position and they were operated under aseptic conditions and under general anaesthesia. In order to provide a lower concentration of muscle relaxant to the patients, a muscle relaxant (cisatracurium besylate) at a dose of only 0.001 mg/ kg· min was injected, which was lower than the dose that is utilized during a conventional surgery (0.0015 mg/kg·min).
The therapeutic electrodes were then punctured transperineally at the margin of the cancer lesion under trans-rectal ultrasound scan-guidance, and the space between electrodes was measured utilizing the ultra-sound scan images.
High-frequency bipolar pulses were administered following determination of the position of the needle electrodes. The burst of HF bipolar pulses, which consisted of 20 pulses each of 5 microseconds, had a total energized time of 100 microseconds, with a 10-µs delay time between the positive and the negative pulses. The schematic of HF bipolar pulses is illustrated in Figure 1C. The initial voltage-to-distance ratio applied which was 1500 V/cm between the pairs of electrodes. The voltage was adjusted during the trial in order to avoid a very large pulse current greater than 40 A. Pulses were administered at a repetition rate of 1 burst/second in sets of 50 pulses, following a 10-second delay so as to avoid an increase in temperature within the tissues; the cycle was repeated for a total number of 250 bursts which were administered between each pair of electrodes. The electrodes were removed pursuant to the treatment, and the patient was catheterized through the urethra before the patient recovered from the anaesthesia.
The Therapeutic Effect Evaluation
Four weeks pursuant to the treatment, magnetic resonance imaging (MRI) scan was utilized to estimate the ablation area. Furthermore, the position of the electrodes in MRI scan image, which would be utilized to analyse the electric field threshold of ablation, was ascertained by matching the MRI scan image and the ultrasound scan image with the location of electrodes.
The efficacy of ablation at the cellular level was analysed in 8 patients who had undergone complete resection of the prostate gland after 4 weeks based upon voluntary principles. These prostate specimens were sectioned and processed for histopathology examination utilizing haematoxylin and eosin staining. Colour images of each tissue section were acquired utilizing the Aperio LV1 Digital Pathology Slide Scanner (Leica Biosystems Inc, Buffalo Grove, Illinois).
Numerical Simulations
The authors stated that it was difficult to reconstruct an accurate 3D model in view of the fact that only low-resolution MRI slices were acquired. Hence, a 2D finite element model of the prostate tissue was established utilizing COMSOL Multiphysics software (version 4.2a; COMSOL Inc, Burlington, Massachusetts). As has been illustrated in Figure 2, the ellipse does illustrate the prostate and the 3 small circles do depict the electrodes. The diameter of the needle electrode was set at 1 mm, and the electrode spacing was set according to the measured distance within the ultrasound scan image. The tumours were not considered in the model in view of the fact that the dielectric parameters of prostate cancer were not clear when HF bipolar pulses were applied.
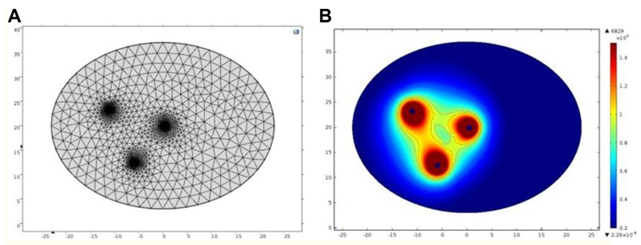
Reproduced from: [94] Dong S, Wang H, Zhao Y, Sun Y, Yao C. First Human Trial of High-Frequency Irreversible Electroporation Therapy for Prostate Cancer. Technol Cancer Res. Treat. 2018 July 25; 17: 1533033918789692 PMCID: PMC6071159 PMID: 30045668 Doi: 10.1177/1533033818789692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6071159/
Copyright © The Author(s) 2018
This article is distributed under the terms of the Creative Commons Attribution-Non-commercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
The electric field distribution in the biological tissue was stated to be closely related to the electrical conductivity and permittivity. The electrical conductivity and permittivity changes during the process of electroporation, but the dynamic response of tissue to HF bipolar pulses had been poorly researched; hence, in the study, the static model was utilized for an initial analysis. The fundamental frequency of the burst in the study was 33.3 kHz, and the corresponding permittivity and conductivity of the prostate tissues, which could be observed from the (reference 22) were 7162.9 and 0.43292 S/m, respectively.
The Laplace equation was utilized to solve the electric field distribution within the tissue region. Within the solution domain, the electric current module was utilized to solve the following equations:
∇⋅J=Q[Am3],---------------1
J=(σ+∊0∊r∂∂t) E[Am2],-------------2
E=−∇U[Vm],--------------------3
where U represents the electric potential, E represents the electric field, J represents the current density, Q represents the current source, σ represents the conductivity, ∊r represents the relative permittivity, and ∊0 represents the permittivity of free space. The boundaries encompassing 1 electrode were assigned a constant electrical potential:
U = U[V].---------------4
The boundaries of the other electrode were assigned as a relative ground:
U = 0[V].--------------5
The remaining boundaries were defined as electrical insulation:
n⋅J=0[Am],-----------6
where n represents the normal vector to the surface and J represents the electrical current density.
The electric field distribution with iso-contours could be computed utilizing COMSOL software through electric field simulation. The electric field lethality threshold could be determined preliminarily by comparing the calculated electric field intensity contours and the ablation zone in MRI section as well as finding the electric field intensity closest to the ablation boundary.
Dong et al. [94] summarized the results as follows:
Reproduced from: [94] Dong S, Wang H, Zhao Y, Sun Y, Yao C. First Human Trial of High-Frequency Irreversible Electroporation Therapy for Prostate Cancer. Technol Cancer Res. Treat. 2018 July 25; 17: 1533033918789692 PMCID: PMC6071159 PMID: 30045668 doi: 10.1177/1533033818789692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6071159/
Copyright © The Author(s) 2018
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage
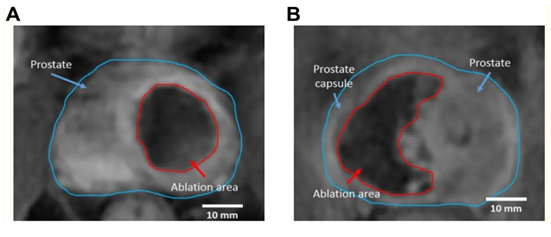
The location of prostate cancer was determined utilizing MRI scan preceding the treatment (see figure 4A). The therapeutic electrodes were then punctured transperineally at the margin of the cancer lesion under trans-rectal ultrasound scan-guidance (see Figure 4B). The authors pointed out that by comparing MRI scan images with ultrasound scan images facilitated the determination of the positions of the electrodes positions in MRI scans as has been demonstrated in figure 4C. The electrode needles were all positioned within the ablation area, and the tissue between the electrodes had been completely ablated. The shape of the ablation area was closely related to the position of electrodes.

Reproduced from: [94] Dong S, Wang H, Zhao Y, Sun Y, Yao C. First Human Trial of High-Frequency Irreversible Electroporation Therapy for Prostate Cancer. Technol Cancer Res. Treat. 2018 July 25; 17: 1533033918789692 PMCID: PMC6071159 PMID: 30045668 doi: 10.1177/1533033818789692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6071159/
Copyright © The Author(s) 2018
This article is distributed under the terms of the Creative Commons Attribution-Non-Commercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
After determining the position of electrodes in MRI scans, the contours of the electric field distributions between each pair of electrodes were drawn as shown out as illustrated in Figure 5. The authors iterated that by comparing the ablation boundaries as well as the electric field distribution allowed the preliminary ascertaining of the electric field lethality threshold with regard to the case of constant conductivity, and the average lethality threshold of the treatment protocol that was utilized in the trial was 522 ± 74 V/cm.
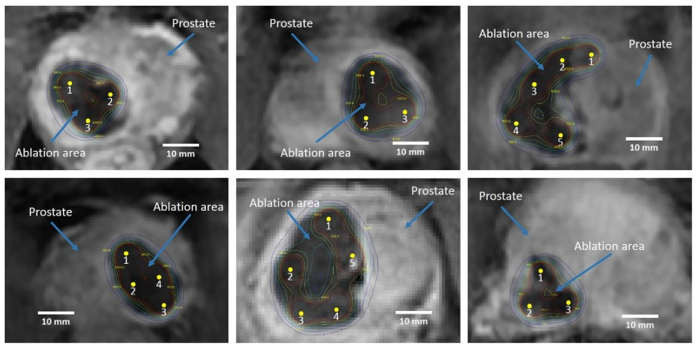
Reproduced from: [94] Dong S, Wang H, Zhao Y, Sun Y, Yao C. First Human Trial of High-Frequency Irreversible Electroporation Therapy for Prostate Cancer. Technol Cancer Res. Treat. 2018 July 25; 17: 1533033918789692 PMCID: PMC6071159 PMID: 30045668 doi: 10.1177/1533033818789692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6071159/
Copyright © The Author(s) 2018
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Dong et al. [94] reported that the prostate glands of 8 patients were excised and utilized for histopathology examination 4 weeks pursuant to their treatment. Histopathology examination of the excised prostate demonstrated that the ablated area had diffuse necrotic glandular tissue without any obvious viable tissue within the ablated zone (see Figure 6A). They also stated that even though Figure 6B demonstrated that large vessels within the tissue were intact, some amount of bleeding was visualised near the electrodes with the demonstration of scattered blood cells in the tissue which might have been caused capillary damage. The ablated zone had been well demarcated from the immediately adjacent unaffected parenchyma of the prostate gland as well as the transition zone between the necrotic glandular tissue in the ablation area as well as the adjacent normal glandular tissue was found to be abrupt (see Figure 6C). Furthermore, necrotic glandular tissue was observed adjacent to the urethra as illustrated in Figure 6D. Nevertheless, the integrity of the urethral structure had remained intact without any evidence of necrosis within the submucosa, even in the scenario when the urethra had been subjected to direct ablation during the safety portion of the study.

Reproduced from: [94] Dong S, Wang H, Zhao Y, Sun Y, Yao C. First Human Trial of High-Frequency Irreversible Electroporation Therapy for Prostate Cancer. Technol Cancer Res. Treat. 2018 July 25; 17: 1533033918789692 PMCID: PMC6071159 PMID: 30045668 doi: 10.1177/1533033818789692 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6071159/ ]
Copyright © The Author(s) 2018
This article is distributed under the terms of the Creative Commons Attribution-Non-Commercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
With regard to the outcome of the treatment procedures, Dong et al. [94] reported the following:
Dong et al. [94] made the ensuing conclusions:
Colletini et al. [95] stated that Irreversible electroporation (IRE) is a nonthermal ablative method which is based upon the formation of nanoscale defects within cell membranes leading to cell death and that clinical experience with the technique for the treatment of prostate cancer had been limited. Collettini et al. [95] evaluated the urogenital toxicity and oncology outcome of MRI–transrectal US fusion–guided IRE of localized prostate cancer. With regard to the materials and methods of their study, Colletini et al. [95] reported that in their prospective study, men who had biopsy-proven, treatment-naive, low- to intermediate-risk carcinoma of the prostate gland with serum prostate-specific antigen [PSA] of equal to or less than 15 ng/mL; Gleason score of equal to or less than 3 + 4 = 7; clinical stage of equal to or less than T2c; lesion size at multiparametric MRI scan of equal to or less than 20 mm, had undergone focal MRI/transrectal US fusion–guided IRE between July 2014 and July 2017. The primary end point of the study was the urogenital toxicity profile of focal IRE by utilizing participant-reported questionnaires. The secondary end points of the study were biochemical, histopathology, and imaging measures of oncology control. Colletini et al. [95] undertook analyses of their data by utilising nonparametric and χ2 test statistics. Colletini et al. [95] summarised the results as follows:
Colletini et al. [95] concluded that after a median follow-up of 20 months, they had found out in their study that focal irreversible electroporation of localized carcinoma of the prostate gland was associated with low urogenital toxicity as well as promising oncology outcomes. Colletini et al. [95] made the ensuing summation as well as Key Points:
Guenther et al. [61] stated that Irreversible Electroporation (IRE) is a new image-guided tissue ablation technology which does induce cell death through very short but strong pulsed electric fields and that IRE had been demonstrated to have preserving properties towards vessels and nerves as well as the extracellular matrix. They also stated that the aforementioned points do make IRE an ideal candidate to utilize for the treatment of prostate cancer (PCa) where other treatment modalities frequently unselectively tend to destroy encompassing structures which induce severe side effects like incontinence or impotence. Guenther et al. [61] reported their retrospective assessment of 471 IRE treatments in 429 patients who had all grades and stages of prostate cancer (PCa) with 6-year maximum follow-up time. With regard to the material and findings in the study, Guenther et al. [61] stated the following:
None
Dong S, Wang H, Zhao Y, Sun Y, Yao C. and Technol Cancer Res. Treat, for granting permission for reproduction of contents and figures of their journal article under Copyright © The Author(s) 2018. This article is distributed under the terms of the Creative Commons Attribution-Non-Commercial 4.0 License (http://www.creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
