AUCTORES
Globalize your Research
Case Report
*Corresponding Author: Sonia De-Miguel-Manso. Department of Pediatrics and Immunology, Obstetrics and Gynecology, Nutrition and Bromatology, Psychiatry and History of Science, Faculty of Medicine, University of Valladolid, Spain. International Hospital.
Citation: Sonia De-Miguel-Manso, Blanca Heras-Pérez, Victoria Pascual-Escudero, Dakota Viruega-Cuaresma, Álvaro Sanz-Díaz-Heredero.(2022). Gonococcal Pelvic Inflammatory Disease with Sepsis Criteria: Review of 2 Cases, J. Women Health Care and Issues, 5(5) DOI: 10.31579/2642-9756/123.
Copyright: © 2022 Sonia De-Miguel-Manso. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 01 June 2022 | Accepted: 12 June 2022 | Published: 15 July 2022
Keywords: neisseria gonorrhoeae; pelvic inflammatory disease; sepsis
Background: Infection caused by Neisseria Gonorrhoeae increases the risk of pelvic inflammatory disease (PID). Gonococcal PID tends to be clinically more severe than non-gonococcal ones. The main is to present two cases of gonococcal PID, with rapid clinical and analytic progression, leading to severe sepsis, but without imaging manifestations.
Clinical presentation:
1. 41-year-old patient with replacement of intrauterine releasing levonorgestrel device (IUD), presented abdominal pain and green vaginal discharge. Abdominal examination revealed signs of peritoneal irritation and blood test showed leukocytosis, increased C Reactive Protein and procalcitonin, as well as coagulation abnormalities. Imaging tests (vaginal ultrasound/tomography) revealed no structural pathology, without collections. Given the criteria of severe sepsis, broadspectrum intravenous (iv) antibiotic therapy was started and laparoscopy and IUD removal were performed. Cervical and IUD cultures were positive for Neisseria gonorrhoeae.
2. 20-year-old woman, with an IUD, consulted for abdominal pain, low-grade fever and green vaginal discharge. Abdominal examination suggested peritoneal sensitivity and laboratory tests leukocytosis, increased C Reactive Protein and procalcitonin with coagulation abnormalities. Imaging tests (vaginal ultrasound/tomography) showed no structural pathology, without collections. Despite analgesia and broad-spectrum iv antibiotics, the patient worsened, proceeding to remove the IUD. Given the criteria compatible with severe sepsis, laparoscopy was decided. Endocervical and IUD cultures revealed Neisseria gonorrhoeae.
Conclusions: Facing the situation of an acute PID with severe and fast clinical worsening even without findings in imaging tests, we should consider gonococcal ethiology as a possible cause. Surgical approach shouldn’t be delayed in order to control the infection and rule out other possible diagnosis.
Gonorrhea, an infection caused by gram negative cocobacillus Neisseria Gonorrhoeae, is a major cause of morbidity among sexually active men and women worldwide. It represents one of the main causes of urethritis in men and cervicitis in women. It increases the risk of pelvic inflammatory disease (PID), infertility, ectopic pregnancy and chronic pelvic pain, as well as complications during pregnancy [1].
PID is an acute infection of internal genital tract, involving uterus, fallopian tubes and ovaries. Frequently, it spreads to adjacent pelvic organs. A sexually transmitted pathogen triggers the infection, which secondarily rises to the superior genital system [2].
PID occurs in approximately 15% of women with cervical gonorrhea, and N. Gonorrhoeae is estimated to be the causative microorganism in 40 percent of PID cases [3]. Gonococcal PID tends to be clinically more severe than non-gonococcal ones [4], but the extent of tubal inflammation and scarring appears to be similar.
The main objective of this work is to present two cases of gonococcal PID, with rapid clinical and analytic progression, leading to severe sepsis, but without findings in imaging tests.
Case 1 :
41-year-old women, smoker, with a history of 3 vaginal deliveries and carrier of an intrauterine releasing levonorgestrel device (IUD) for 5 years ago. She didn’t use any barrier contraceptive method since she has a stable sexual partner. She consulted for lower abdominal pain, that has appeared sharply in the last 24 hours. It was associated with green vaginal discharge, loss of appetite and bilious vomiting within the last few hours. Two days ago, her IUD was replaced by her gynecologist.
During abdominal examination, she complained of intense hypogastric and mesogastric pain, as well as generalized defense. Also, positive Blumberg sign was present, suggesting peritoneal irritation. In vaginal examination, grayish vaginal discharge was noticed as well as correctly placed IUD threads. We took vaginal and endocervical microbiologic samples. Cervical motion was painful and no adnexal masses were palpable.
Vital signs were taken and blood and urine samples collected. Results are shown in table 1 and 2 respectively.


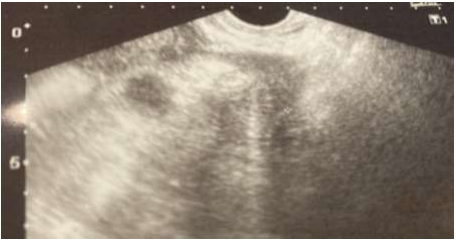
Vaginal ultrasound revealed regular uterus with normally positioned IUD (figure 1) and both ovaries without any ecographic findings (figures 2,3). A slight amount (23 x 18 mm) of free anechoic fluid with internal echos was noted in Douglas pouch (figure 4).



An abdominal CT was performed, with no findings in superior abdominal cavity as well as uterus and both ovaries, and correctly placed IUD. Small bowel dilatation was described from jejunum, with ileum loops in pelvis, showing 40 x 6 mm of mural thickening. This was attributed to a patched ileitis, with normal large bowel and small amount of free pelvic fluid.
We then suspected a pelvic inflammatory disease (PID), stage two (acute salpingitis associated with peritonitis) (5), without being able to rule out ileitis.
The patient was also evaluated by a general surgeon, who dismissed surgical approach at this moment.
Considering the presence of severe sepsis criteria (both clinical and analytic), pathologic abdominal and pelvic examination and the background of IUD replacement 48 hours ago, we started intravenous (i.e.) antibiotic treatment with Piperacillin-Tazobactam 4 g every 6 hours.
Diagnostic laparoscopic exploration was also performed, showing purulent pelvic fluid, omental inflammatory reaction and right fallopian tube edematous and hyperemic. We confirmed the presence of small bowel dilated loops in the proximity of right tube. Both uterus and left fallopian tube were macroscopically normal, such as the rest of the abdominal cavity. A bilateral salpingectomy was completed after profuse abdominal washing and aspiration and an abdominal drain was placed. We removed IUD after first antibiotic i.e. dose and it was sent for microbiological further studies.
Postoperative evolution was favourable. Endocervical and IUD cultures were positive for Neisseria Gonorrhoeae. After 48 hours of intravenous Piperacillin/Tazobactam, we switched antibiotic treatment to 500 mg ceftriaxone + 2 g azithromycin single oral dose. We alerted our patient that her sexual partner needed to be treated as well. He had a previous course of antibiotic 10 days ago, prescribed by his general doctor due to a possible urethritis. We recommended to avoid sexual intercourse during recovery.
At 30 days post operative check-up, patient was completely asymptomatic and new endocervical sample was negative for sexually transmitted germs.
20-year-old smoker and nulliparous woman. She was using since 4 years ago IUD as her contraceptive method and had a stable sexual partner at the moment of consultation.
She presented in the emergency room (ER) complaining of abdominal tenderness associated with greenish vaginal discharge for the last 4 days, as well as nausea and vomiting.
During abdominal examination, the patient complained of intense pain in left iliac fossa, along with signs of peritoneal irritation. Bilateral costovertebral angle percussion was negative.
In vaginal exam, IUD threads and pathological discharge were noticed and vaginal and endocervical samples we taken for microbiological testing. Palpation of left adnexal area showed tenderness as well as cervical painful motion.
Vital signs, blood and urine test results are shown in table 1 and 2, respectively.
Vaginal ultrasound showed regular uterus with normally positioned IUD and both ovaries without any sonographic findings (figures 5 and 6). A slight amount of free anechoic fluid with internal echo's was noted in Douglas pouch (figure 7).



Superior abdominal cavity as well as uterus, IUD and both ovaries were described as normal in CT abdominal scan. Thickened and enhancing pelvic peritoneum was observed without neither suspicious collection nor signs of bowel perforation. In addition, non-dilated but enhanced bowel loops were noted, with normal cecum and minimum amount of free pelvic fluid.
Stage II PID was suspected and patient was then admitted for observation and antibiotic treatment (ampicillin 2 g every 6 hours, clindamycin 900 mg every 8 hours and gentamicin 240 mg daily). A significant clinical and analytical worsening occurred during the following hours, leading to a severe sepsis. We then decided to remove IUD (sent to microbiological testing) and laparoscopic abdominal exploration. Patient was informed and consented the procedure.
Findings of laparoscopic examination consisted in hyperemic uterus, slightly swollen fallopian tubes but no pelvic abscesses. In addition, moderate amount of purulent free fluid was noted and important dilatation of bowel loops. At the end of the procedure, we placed an abdominal drain.
Postoperative evolution was without further complication. Both endocervical and IUD microbiological cultures were positive for Neisseria Gonorrhoeae and Chlamydia Trachomatis. We suspended antibiotic intravenous treatment. At the time of discharge, we prescribed both our patient and her sexual partner treatment with single oral dose of azithromycin 2 g and doxycycline 100 mg every 12 hours for 14 days. We advised them not to have sexual intercourse till the end of antibiotic course, and to switch to barrier method as contraception.
At 30 days postoperative check-up, patient was completely asymptomatic and endocervical sample resulted negative.
Ethical approval: for the preparation of this manuscript, both patients were informed of the scientific interest of their processes and their verbal consent was obtained, both for the publication of their data and images (Figures 1-7).
Genital infections, particularly cervicitis, are the most commonly associated with N. Gonorrhoeae and might spread to upper genital tract, causing PID.
Uterine cervix is the most frequent site of mucosal gonococcal infection in women. Up to 70 percent of these infections are asymptomatic [6,7]. Thus, the incubation period of gonorrhea is less well characterized in women than men. When present, genital symptoms tend to develop within ten days after exposure [8]. Symptomatic infection typically manifests as vaginal pruritus and/or a mucopurulent discharge. In rare cases, intermenstrual bleeding or menorrhagia can appear. The presence of abdomino-pelvic pain or dyspareunia should raise suspicion for upper genital tract involvement [9,10].
Given the high incidence of asymptomatic gonococcal infections, PID can be the first sign and these patients can end up being severely ill [4].
It is frequent that symptoms start with the beginning of menstruation [1]. This was first described back in 1979, when female rats were inoculated with N. Gonorrhoeae. A comparison between the pattern of infection was conducted, regarding if germs were suspended or not in mucine and hemoglobin. Those hanging in mucine and hemoglobine lead more frequently to gonococcal bacteremia due to phagocytosis interference and intracellular death of N. Gonorrhoeae. This model mimics the progression in women with PID from local peritonitis to blood spread with factors (mucine and hemoglobine) increasing infection [11].
More recent references also link menstruation to a higher risk of gonococcal dissemination, due to:
❖ Phenotypical switching of N. Gonorrhoeae from opaque strains to transparent ones (modified expression of transmembrane proteins) [12]. These modifications can reduce sensibility to trip sine lysis, neutrophil adhesion as well as increased adherence to fallopian tubes [13].
❖ Alkalinization of genital discharge, stimulating gonococcal growth [14].
❖ Increased mucosal concentration of transferrin and hemoglobin. This can be used as an iron source by N. Gonorrhoeae [16].
Normally, superior genital tract is protected by endocervix from germs of vaginal ecosystem. Endocervical infection by N. Gonorrhoeae can break this natural barrier, allowing the compromise of superior genital organs and adjacent ones. The resultant infection can be subclinical or in the way of pelvic inflammatory disease. Immune system response genetic variations, estrogen levels compromising viscosity of cervical mucus and bacterial charge, can explain this variable expression [9,17].
N. Gonorrhoeae and C. Trachomatis are frequently identified pathogens in PID among premenopausal sexually active women.
Nevertheless, in the majority of diagnosed cases, we are not able to clarify microbiological etiology. Despite the germ that triggers infection, we usually consider PID as a polimicrobian infection [2].
N. Gonorrhoeae is also a frequent cause of urethritis in men. Up to 60% of these patients can be asymptomatic or experience slight symptoms [18,19]. Among symptomatic ones, incubation period takes between 2 to 5 days [20].
Sexual intercourse is the main PID risk factor, especially in case of multiple partners. Younger patients, previous Chlamydia infection or PID episode and a sexual partner with a history of sexually transmitted disease (STI) are other significant risk factors. Contraception is also important in the prevalence of PID. The use of barrier method constitutes a protective factor [2].
There is a clear relation between PID and other contraceptive methods, as described below:
❖ Oral contraceptives (OCs) and PID have a complex interaction. Several publications have stated that OC use nearly doubles the prevalence of both chlamydia and gonococcal cervical infection [21,22]. Nevertheless, OC have traditionally been associated with a significant reduction of PID. Apparently, women using OCs tend to develop PID as frequently as other women, but the severity of the infection is substantially inferior [23,24].
❖ Modern intrauterine devices (IUD) don’t increase PID risk and this one is limited to the first 3 weeks after its insertion. There is evidence supporting leaving IUD inside the uterine cavity during the first 48 to 72 hours of acute PID antibiotic treatment, with close follow-up. If there is no response to treatment or in case of high-risk patients, IUD should be removed and microbiological studies can be performed to guide antibiotic regimen selection [25-27]. Although a case of infection of the IUD by actinomyces has been reported, leading to bilateral tubo-ovarian abscess in a postmenopausal woman with an IUD of 12 years of evolution [28].
❖ Tubal ligation may protect the distal oviducts from involvement, but the clinical syndrome of PID is otherwise unaffected.
Taking into account risk factors in our cases, we noted that patient 1 had a recent IUD replacement. We suggest that it is possible that cervical infection was already present at the day of cervical manipulation. This statement is based in her sexual partner previous symptoms (suspected urethritis) for which he was treated with oral antibiotics 7 to 10 days before patient admission.
Regarding patient 2, she was a young women aged 20, with several sexual partners in the past and IUD user, without barrier contraception associated.
In case 1, considering childbearing was completed, even though no tubal abscesses were present, we agreed with our patient to perform bilateral salpingectomy. This way we assured posterior contraception and reduced severity in case of PID relapse.
In both of our cases, we removed IUD after first dose of intravenous antibiotics (case 1 removal performed during surgical procedure, case 2 after no evidence of improvement with antibiotics), because of clinical severity. They both required hospital admission and parenteral antibiotics, being most frequent indications for this:
• Clinical severity (high fever > 38.5º, nausea, vomiting, intense abdominal pain…)
• PID complicated with the presence of pelvic abscess. • Surgical approach considered because of suspicion of ruptured pelvic abscess or confirming alternative diagnosis (appendicitis, ovarian torsion…).
• Inability to take oral medication because of intense nausea or vomiting. • Lack of response to oral antibiotics.
• Concern for non-adherence to therapy.
Antibiotic therapy is the cornerstone of PID treatment. For hospitalized patients, initial treatment consists in a parenteral regimen that provides antimicrobial coverage against a wide range of bacteria, including C. trachomatis and N. gonorrhoeae (most frequent STIs associated with acute PID), streptococci, gram-negative enteric bacilli (Escherichia coli, Klebsiella spp, and Proteus spp), and anaerobic organisms (bacterial vaginosis-associated flora) [29].
United States Centers for Disease Control and Prevention (CDC) recommends these following regimens [30]:
• Cefoxitin (2 g i.e., every six hours) or Cefotetan (2 g i.v. every 12 hours) plus doxycycline (100 mg every 12 hours oral or i.e.).
• Clindamicine (900 mg every 8 hours) plus gentamicin (3-5 mg/kg daily i.v. or 2 mg/kg i.v. followed by 1.5 mg/kg every 8 hours).
Regimens based on second generation cephalosporin plus doxycycline are preferred because of their tolerability and security. They also show excellent in vitro activity against N. gonorrhoeae and C. trachomatis. Regimen with gentamicin combined with clindamicine has only moderate in vitro activity against these bacteria [30,31]. However, both regimens have shown in several trials short-term clinical cure rates of more than 80 to 90 percent of cases [32,33].
Alternative regimens have more limited clinical data to support their use for hospitalized patients and less gonococcal activity
• Ampicillin-sulbactam (3 g i.v. every six hours) doxycycline (100 mg twice daily). This combination results in a similar clinical cure rate as cefoxitin plus doxycycline [33,34].
• Azithromycin (500 mg i.v. daily for one to two days followed by 250 mg orally daily to complete a five to seven-day course) with or without metronidazole (in case of pelvic abscess), lead to similarly high clinical and microbiologic cure rates (>95 percent) for mild to moderate PID compared with a combination beta-lactam and doxycycline regimen. Azithromycin was not evaluated in severe PID cases [35].
In patient 1, we combined penicillin with a beta lactamase inhibitor because diagnosis remained unclear, considering either grade II PID or ileitis. This regimen was not optimal in case of PID diagnosis. Doxycycline association would have been ideal in order to cover most frequent pathogens in PID, including STIs.
In contrast, parenteral treatment in patient 2 was adequate, combining ampicillin, clindamicine and gentamicin.
Both patients experienced a similar and adverse clinical evolution, suggesting severe sepsis because of the presence of the following criteria (table 3) [36]:
• White cell count over 12.000/mm3
• C- reactive protein (CRP) and procalcitonin (PCT) increase
• Coagulation disfunction (INR > 1.5)
• Systolic blood pressure < 90>

Even though neither structural nor organic pathology was observed in imaging tests, we decided that surgical approach was necessary because of adverse clinical evolution within the first hours of hospital admission and severe sepsis criteria. After at least 24 hours of clinical improvement, patients can usually be switched from parenteral therapy to oral antibiotics, consisting in administration of 100 mg doxycycline twice daily in order to complete a 14-day course. In case of not tolerating doxycycline, azithromycin (500 mg for 1 or 2 days followed by 250 mg once daily in a 7-day course) is an adequate option [37]. In our patients, after a consistent 48 hours clinical improvement and considering endocervical and IUD microbiological results, we stopped parenteral treatment. Patient 1 received intravenous extra 500 mg ceftriaxone and 2 g azithromycin single oral dose. In patient 2, we combined this same azithromycin single dose with 100 mg doxycycline twice daily for 14 days.
Patients diagnosed and treated for acute PID should be carefully advised on the following topics:
• Long antibiotic course of treatment: compliance with this kind of treatment can be problematic [37]. Patients should be educated about the importance of medication adherence and clinical outcomes.
• Sexual activity: patients with PID diagnosis should avoid sexual intercourse until they have completed therapy, their symptoms have disappeared and partners have been screened and treated for STIs. We should explain STIs way of transmission and counsel safe sex practices.
• STIs screening and prevention: patients should also be tested for HIV, syphilis… [37].
• Evaluation and treatment of sex partners: they should be treated in case of sexual intercourse with the patient during 60 days prior to the onset of symptoms, regardless of the woman's STI test results. Treatment regimens should include antibiotics with activity against N. gonorrhoeae and C. trachomatis [37]. If the patient denies sexual activity during previous 60 days, most recent sexual partner should be tested and treated [38]. Sexual partners, frequently showing no symptoms, are capable of reinfecting the index patient or spreading the infection to other sexual contacts. Expedited partner therapy (EPT) is a strategy to secure treatment of sexual partners of STI positive patients. Without any medical evaluation, we provide prescriptions or medication to the patient, who will deliver it to the partner(s) [38,39]. It is always preferable to evaluate before treatment, but EPT can be helpful in cases in whom clinical evaluation is unlikely. The benefits of EPT implementation are reduced rates of reinfection and increased number of patients receiving treatment. In randomized trials, EPT was more effective than traditional partner notification (the patient communicates his/her partner the need for clinical evaluation and treatment) in reducing persistent or recurrent urogenital gonococcal infection [40, 41]. Nevertheless, we can lose the chance for other STIs/HIV screening and it is possible that adverse effects caused by antibiotic treatment won’t reach a health-care professional [41,42].
First-line treatment for non-complicated gonococcal infections consists in third generation cephalosporins, due to increasing resistance rates to other antibiotics (penicillin, fluoroquinolones, tetracycline, sulfonamides) [43]. Among them, ceftriaxone is the most frequently used in a single high dose regimen. CDC recommendations are:
• 500mg intramuscular ceftriaxone, single dose if weight < 150>
• 1000 mg intramuscular ceftriaxone, single dose if weight > 150 kg.
These ceftriaxone regimens include higher doses in order to face rising gonococcal minimum inhibitory concentrations (MICs). Ceftriaxone + azithromycin was a frequent combination not long ago [43], but consistent data have demonstrated decreased susceptibility of N. Gonorrhoeae to azithromycin [43,44].
If concurrent C. trachomatis infection has not been ruled out by tests, we should prescribe treatment for Chlamydia at the same time as gonococcal regimen. Following CDC recommendations, we suggest doxycycline 100 mg orally twice a day during 7 days. Single-dose azithromycin is also a valid option. Nevertheless, considering the already mentioned decreased susceptibility of N. Gonorrhoeae to azithromycin, doxycycline regimen is preferred [44].
• Notification of N. Gonorrhoeae and C. Trachomatis infection as mandatory reported infectious diseases: these two infections are reported to public health system many countries. In Spain, cases are notified to “Sistema de Information Microbiological”. Spanish incidence rate per 100.000 inhabitants during 2008 was 13.78 for gonococcal infection and 12.81 for chlamydia [45].
• Reinsertion of IUD: in case previous IUD was removed during acute infection, the optimal moment for re-insertion remains unclear. We suggest to wait until antibiotic treatment is completed, all symptoms have disappeared and cervical screening is negative. Because of high rates of reinfection, retesting for N. gonorrhoeae and C. trachomatis is counseled within 3 months of the original infection [46].
• Test of cure: Asymptomatic patients following treatment for uncomplicated urogenital or anorectal gonococcal infections do not need to return for a microbiological culture [43]. This test is the preferred one and it should be performed at least 7 days after treatment [47,48]. Nucleic acid amplification tests (NAATs) are also a valid test of cure, but should be conducted at the minimum 14 days following therapy. If NAAT is performed too soon after treatment, false-positive results (from detection of nonviable organisms that may not represent persistent infection) can appear [49,50].
In our cases, we provided our patients with a recommendation of the antibiotic regimen their partners should follow (via EPT), considering microbiological tests results. Patient 1 sexual partner was treated with ceftriaxone (with activity proved against N. Gonorrhoeae) and azithromycin (useful for other germs such as C. trachomatis). In case 2, sexual partner was treated with azithromycin and doxycycline (first-line option for gonococcal infection would have been ceftriaxone, due to reduced susceptibility to azithromycin, but optimal coverage for C. trachomatis was assured by doxycycline).
Both our patients presented with gonococcal infection + acute pelvic inflammatory disease (PID), so we decided to perform endocervical culture as test of cure. This test was carried out one month after treatment and resulted negative. In patient 2, sexual counseling was particularly important ir order to avoid STIs reinfections (age, multiple sexual partners…). We didn’t perform other STIs (HIV, syphilis) testing.
• Gonococcal infection is an STI that can be asymptomatic in up to 70% of patients. This infection can lead to an acute PID that tends to be clinically more severe than non-gonococcal ones.
• We have resumed two cases of gonococcal PID with a fast clinical worsening, even meeting severe sepsis criteria.
• Therefore, facing the situation of an acute PID with severe and fast clinical worsening even without findings in imaging tests, we should consider gonococcal ethiology as a possible cause. Surgical approach shouldn’t be delayed in order to control the infection and rule out other possible diagnosis.
The authors have no relevant financial or non-financial interests to disclose
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
