AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Priya Jeyaraj, Classified Specialist (Oral & Maxillofacial Surgery), Commanding Officer Military Dental Centre (Gough Lines), Secunderabad, India.
Citation: Priya J Effectiveness of ‘Preauricular-Retroparotid’ and ‘Retromandibular-Transparotid’ Approaches in the Management of Displaced and Dislocated Condylar Head and Neck Fractures.Problems in the Estimation of the Key Parameters using MLE in Lung Cancer Screening. J Clinical Research and Reports, 5(4); DOI:10.31579/2690-1919/122
Copyright: © 2020 Priya Jeyaraj. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 26 August 2020 | Accepted: 07 September 2020 | Published: 10 September 2020
Keywords: condylar head and neck fractures; preauricular-retroparotid approach; retromandibular-transparotid approach; open reduction & internal fixation (ORIF)
Introduction: Management of fractures of the condylar head, neck and base regions can be quite tricky, owing to differences in the morphology and location of the fracture, degree & direction of displacement, extent of comminution, and position of condylar head in relation to glenoid fossa. Hence, choosing an ideal surgical approach for each individual case, is both difficult as well as important.
Aim: To assess the effectiveness of two major surgical approaches, the ‘Preauricular-Retroparotid’ and ‘Retromandibular-Transparotid’ approaches in the management of different types of displaced and dislocated condylar head and neck fractures.
Patients and Methods: This retrospective study includes 56 patients operated over a period of four years from Jan 2016 to Dec 2019, of whom 14 had bilateral and 42 had unilateral displaced condylar head or neck fractures. 22 surgeries were for condylar head or high condylar neck fractures, treated using the Preauricular-Retroparotid approach. 48 surgeries were for low condylar neck fractures, managed using the Retromandibular-Transparotid approach. Intraoperative and postoperative complications, and detailed objective, subjective and functional treatment outcome assessments, were recorded over a postoperative follow up period ranging from one to three years.
Results & Conclusion: Both surgical approaches were found effective in achieving good esthetic and functional results with no major complications, other than occasional transient neurological deficits and few instances of salivary fistulas and sialocoeles. Depending upon the level of the condylar fractures, a preauricular approach is ideal for the condylar head and high condylar neck fractures, providing direct and easy visualization to the region, for retrieval and repositioning of the medially displaced and dislocated proximal fracture fragment. The retromandibular approach is more suited for the lower level condylar neck fractures, providing a direct visual field and a wide, straight line access for implant fixation at this region.
Management of condylar process fractures can often be challenging, as they are hard to access, and comprise of small and slender fragments that are difficult to anatomically realign, precisely reposition, and effectively fix in a stable manner. Implant hardware placement is intricate and difficult as well, given the restricted access and limited visibility of the region [1]. Furthermore, medial angulation and displacement of the proximal fragment, dislocation of the fractured condyle out from the glenoid fossa, and often, antero-medial displacement into the infratemporal fossa, makes the displaced fragment difficult to locate, retrieve, manipulate, reduce and fix. Presence of vital anatomic structures such as the Facial nerve and Parotid gland in the immediate vicinity of the surgical field, further complicates the already complex surgical procedure.
The primary objective of any treatment protocol for condylar fractures is to restore function and aesthetics, that is, to achieve a stable occlusion, satisfactory masticatory efficiency and full range of mandibular movements, as well as to restore the lower facial height and to correct any facial symmetry resulting from jaw deviation, if present. This is achieved by restoring lost ramal height, repositioning the dislocated condyle back within the glenoid fossa thus restoring integrity of the Temporomandibular joint (TMJ), and ensuring an optimum reapproximation of the proximal and distal fracture fragments of the condylar process [2].
Though the debate between open versus closed treatment of condylar region fractures is ongoing [3, 4], open treatment seems to outscore the latter by producing a faster and more predictable outcome. Other advantages of open treatment are that it permits repair of the soft tissues of the TMJ region, enabling the capsule and ligaments to regenerate, allows repositioning of the displaced articular disc into its proper position, restores the function of the lateral pterygoid muscle and thus restores and reconstructs the entire TMJ. This enables the condyles to immediately return to their optimal function, performing unhindered, smooth and synchronous translatory and rotational movements [3]. Open reduction and internal fixation (ORIF) enables precise reapproximation of the proximal and distal fracture fragments of the fractured condylar process [2], which in turn, leads to direct bone repair at the fracture gap without formation of fibrous connective tissue. It also reduces the risk of future ankylosis of the joint. The need for maxillomandibular immobilisation is obviated, which is a major advantage from the patient’s perspective.
In order to achieve anatomic reduction of condylar fractures, it is essential to gain adequate exposure of the surgical field for direct visualization of the fractured ends, as well as for mobilisation, retrieval and repositioning of the displaced segment. A large distance between the incision line and the fracture level often necessitates excessive and forceful retraction of tissues, leading to nerve injuries, haemorrhage from severed vessels and tissue damage. Hence choice of the surgical approach is of paramount importance in reducing intra- and post-operative complications [5, 6].
Over the years a number of surgical routes and approaches have been used to access the TMJ area and apply the osteosynthesis fixation system, for e.g. the submandibular, retromandibular, preauricular, coronal, endoscopic and intraoral approaches [7-9].
Our study was conducted to retrospectively assess the clinical effectiveness of the preauricular-retroparotid and retromandibular-transparotid approaches in the management of 56 patients (a total of 70 condylar process fractures), with displaced and dislocated condylar head or neck fractures.
The aim of this study was to assess the clinical effectiveness of the preauricular-retroparotid and retromandibular-transparotid approaches, for managing different types and levels of displaced or dislocated condylar head and neck fractures. This was to be determined by pursuing the following objectives:
The retrospective analytical study included cases operated from Jan 2016 to Dec 2019. It included 56 patients, between 08 and 70 years of age. 14 patients had sustained bilateral condylar fractures, while 42 had unilateral fractures, amounting to a total of 70 condylar surgeries performed. The choice of access was primarily based on the level of the fracture. 22 of the condylar process fractures, which were either condylar head or high condylar neck fractures (Group ‘A’), were managed using a preauricular-retroparotid approach. The remaining 48 fractures which were low level condylar neck fractures (Group ‘B’), were managed by the retromandibular-transparotid approach.
The demographic data recorded, included age and gender of the patients, mode of injury and type of the condylar fracture based on uni-or bilateral involvement (Table 1). Details of the levels of the condylar fractures, presence of associated and concomitant injuries, surgical approach and treatment modality employed were recorded (Tables 2 &3). Complications encountered, both intra- and postoperatively, were recorded and compared between the two surgical groups (Table 4, Graphs 9-11). Objective, subjective as well as functional outcomes of treatment, were assessed and compared between the two treatment groups (Table 4, Graphs 12-14).
1. | Condylar Fractures | 70 (57 Patients) |
| Bilateral | 14 |
| Unilateral | 42 |
2. | Sex |
|
| Male | 48 |
| Female | 08 |
3. | Mode of Injury |
|
| Road Traffic Accident | 19 |
| Fall | 25 |
| Interpersonal violence | 06 |
| Sports related injury | 05 |
| Occupational injury | 01 |
4. | Age groups (Years) |
|
| ≤10 | 03 |
| 11-20 | 05 |
| 21-30 | 14 |
| 31-40 | 27 |
| 41-50 | 05 |
| 51-60 | 01 |
| 61-70 | 02 |
Table 1: Demographic Data of the Study
Patients with clinical and radiographic evidence of displaced or dislocated condylar head or neck fractures, presenting with any of the following criteria were included in the study:
(a) Derangement in occlusion
(b) Restriction of interincisal mouth opening to 25mm or less
(c) Restriction in excursive mandibular movements
(d) Concomitant fractures of the Maxillofacial skeleton requiring ORIF
(e) Cases contraindicated for Maxillomandibular fixation
(f) Ramal foreshortening with resulting mandibular and facial asymmetry
(g) Uni- or bilateral premature occlusal contact with open bite
The following patients were excluded from the study:
(a) Medically compromised patients, contraindicated for surgery under general anaesthesia
(b) Undisplaced condylar fractures with no functional and aesthetic deformity.
Diagnostic Imaging and Grouping of Cases:
Orthopantomograms (OPG) and Non-contrast computed tomographic (NCCT) scans were the diagnostic imaging modalities of choice to assess the type, morphology, displacement, dislocation and angulation of the condylar fractures.
Based on the level of the condylar fractures, the cases were placed into two groups (Table 2). Condylar head fractures (Neff’s fractures) [7] and high condylar neck fractures were placed into Group A. All low condylar neck fractures were placed in Group B. The grouping of the 70 cases of condylar fractures was carried out based on individual condylar fracture level, irrespective of whether the patient had sustained a unilateral or bilateral condylar fracture. Hence, some of the patients with bilateral condylar fractures, who had different levels of fractures on the two sides, fell into both groups.
1. | Condylar Fracture Classification |
| |
| Condylar Head # | 06 16 | (Group A) |
| High Condylar Neck # | ||
| Low Condylar Neck # | 48 (Group B) | |
2. | Concomitant Maxillofacial & Head Injuries |
| |
| Mandible # (Angle / Body/ Parasymphysis) | 14 | |
| Maxilla # | 03 | |
| Zygomatic Complex # | 05 | |
| Naso-orbito-ethmoid (NOE) # | 01 | |
| Head Injury | 02 | |
3. | Surgical Approach employed for the Condylar # |
| |
| Preauricular Retroparotid approach | 22 (Group A) | |
| Retromandibular Transparotid approach | 48 (Group B) | |
4. | Operative procedure employed |
| |
| Fragment retrieval and removal | 02 Condylar head #s | |
| Open Reduction & Internal Fixation (ORIF) | 68 | |
Table 2: Details of the condylar fractures, grouping of cases and management
Treatment protocols employed:
The management protocol was based on the level of the fracture and other features like the status of the proximal fragments etc. 07 cases (03 of them bilateral and 04 unilateral condylar fractures) have been illustrated (Fig 1-12).

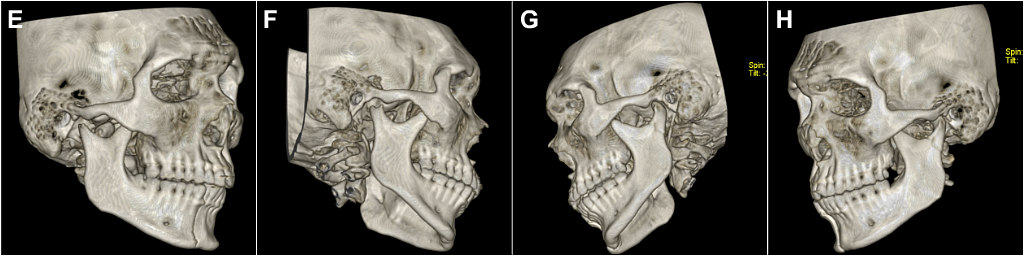

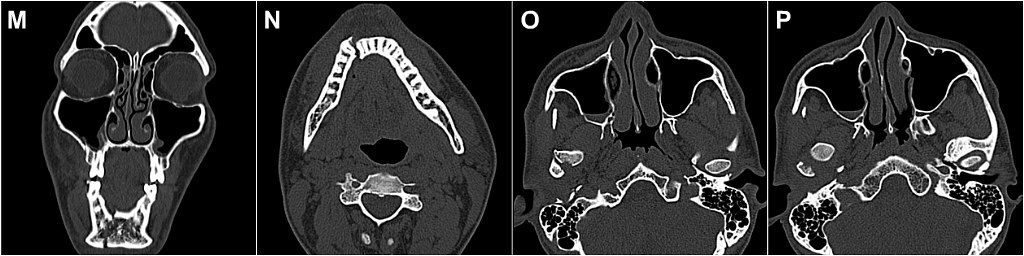


Fig 1: (Case 1) (A-B) Bilateral condylar and right parasymphyseal fracture in a 24yr old male. (C-P) NCCT showing right parasymphyseal fracture, right condylar head fracture with its anteromedial displacement into the infratemporal fossa, and mildly displaced left condylar neck fracture. (Q) ORIF of right parasymphyseal fracture. (R-T) Retromandibular transparotid approach for fixation of left condylar neck fracture using 3-D Delta Titanium miniplate. (U-X) Preauricular retroparotid approach for retrieval and fixation of medially dislocated right condylar head.
The following management strategies were used
Surgical approaches employed:
The surgical approach for each case was selected on the basis of the level of the factures and proximity of the fracture site to the respective incision lines of the two approaches. The preauricular-retroparotid approach was used for all condylar head and high neck (Group A) fractures. (Table 3). The retromandibular-transparotid approach was employed for the low condylar neck (Group B) fractures. (Table 3). 07 cases (03 of them bilateral and 04 unilateral condylar fractures) have been illustrated (Fig 1-12).
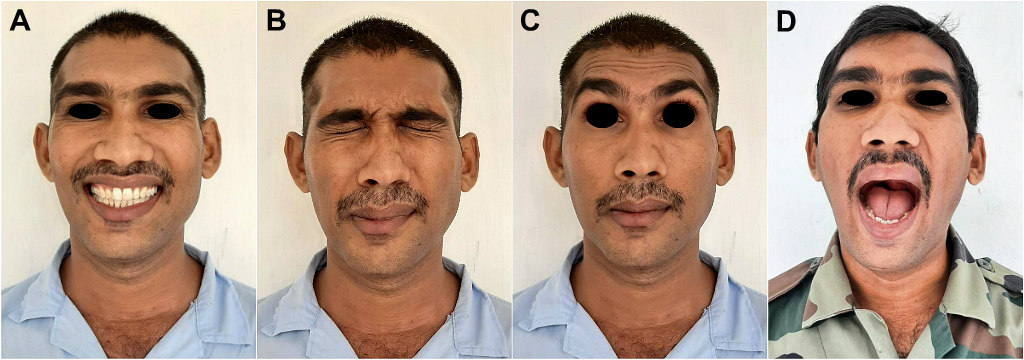

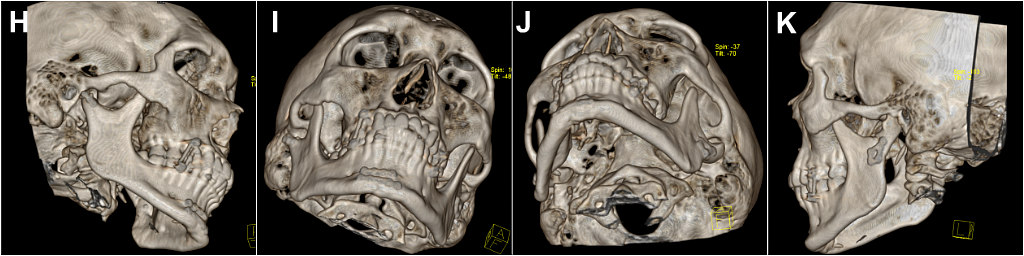

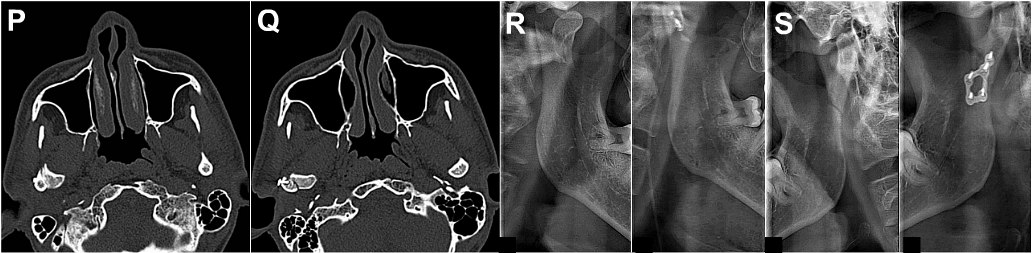
Fig 2: (Case 1)(A-F) Stable postoperative occlusion, nil neurological deficits, normal mouth opening and well healed operated sites, with barely perceptible scars. (G) Pre- and postoperative OPGs, showing precise reduction and fixation of all fractures. (H-Q) NCCT showing successful repositioning of dislocated right condylar head back within the glenoid fossa and three dimensional realignment and ideal fixation of fractures of bilateral condylar and parasymphyseal fractures. (R,S) TMJ view before and after ORIF of condylar fractures.
Table 3: Grouping of condylar surgeries based on fracture level and surgical approach employed
Level of Condylar Fractures | Number of Cases | Grouping of Cases | Surgical Approach employed | |
Condylar Head fractures |
06 | Total
22 |
Group A |
Preauricular-Retroparotid approach |
High Condylar Neck fractures |
16
| |||
Low Condylar Neck fractures |
48
|
Group B | Retromandibular-Transparotid approach | |
The preauricular-retroparotid approach was carried out through a vertical incision placed in a preauricular skin crease just anterior to the tragus, which was extended inferiorly until the earlobe. A ‘hockey-stick’ or ‘question-mark’ shaped temporal extension was added for greater visibility and access (Figs 1, 5, 6, 10 & 11). The TMJ was exposed with retraction of the developed flap. At no point was the parotid gland traversed or its capsule incised or breached, and all dissection remained posterior to and beneath it. The dissection was carried out retrogradely underneath the parotid gland to the joint to expose the capsule of the TMJ, which was then incised to expose the fracture site.
The Retromandibular-Transparotid approach was carried out using a vertical incision below the ear lobe which extended inferiorly parallel to the posterior border of the ramus, (Figs 1, 3, 8 & 10). The parotid capsule which appeared as white, glistening layer, was reached, which was then sharply incised. The gland was blunt dissected in an anteromedial direction between the marginal and buccal branches of the facial nerve, towards the posterior border of the mandible. The periosteum was then incised through the relatively avascular zone. This was followed by wide subperiosteal stripping to adequately mobilise the soft tissues and to expose and visualise the ramal stump and subcondylar region. A braided wired threaded through a hole drill through the angle of the mandible was sometimes used to apply downward traction for ease of visualization, retrieval, and fixation. A periosteal elevator was then used to scoop up the fragment as well as the articular disc and retrieve and reposition them.
Extracorporeal plate fixation was carried out when indicated. Those fragments which were too small to be fixed, were removed, and the articular disc repositioned. Wound closure was performed in layers, using resorbable Vicryl 3-0 and silk/ proline sutures were used for the skin closure. Postoperative antibiotics, analgesics, and anti-inflammatory medications were prescribed. Few patients required a brief period of IMF using light elastic traction to guide the teeth in occlusion. The patients were placed on a soft diet for the first 3 weeks. Imaging studies, including Orthopantomogram and/or NCCT were carried out after the surgery for all patients. The patients were reassessed regularly at 1, 3, 6, and 12 months after the surgery. The minimum follow-up period was 12 months.

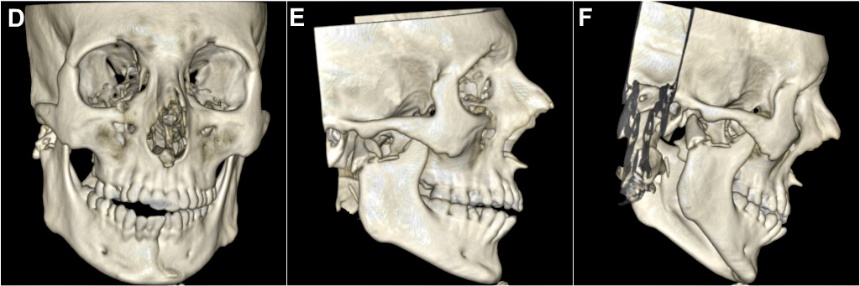





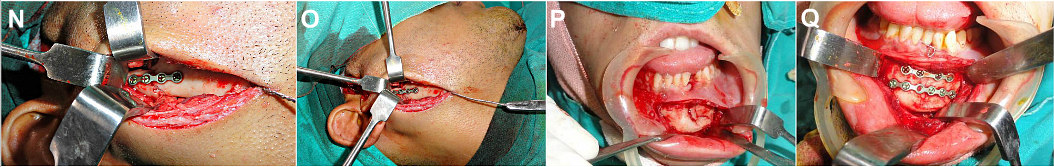
Fig 3: (Case 2) (A-F) 23yr old male with right condylar neck and left parasymphyseal fractures. Deranged occlusion, restricted mouth opening and deviation of dental midline to the right. (G-I) NCCT showing medial dislocation of the proximal condylar segment, and loss of its bony contact with the distal ramal stump. (J-M) Retromandibular transparotid approach to expose the fracture. Braided wire threaded through angle of the mandible for inferior traction. (N,O) Displaced proximal condylar fragment retrieved, repositioned and fixed. (P,Q) ORIF of left parasymphyseal fracture.
Parameters for Treatment Outcome Assessment:
A comparison of the Intraoperative and Postoperative Complications encountered in the 70 Condylar surgeries carried out in this study, employing the two different Surgical approaches, are presented in Table 4, Graphs 1 & 2. A comparison of the subjective, objective and functional treatment outcomes achieved, using the two approaches has also been presented in Table 4, Graphs 3, 4 & 5.
(A) Assessment of Intra-operative Complications | |||
|
| Preauricular Approach (for Condylar head & high Condylar neck #s) 22 Surgeries (Gp A) | Retromandibular Approach (for low Condylar neck #s) 48 Surgeries (Gp ‘B’) |
1. | Limited Access and Visibility of Operative Field | 08 | 04 |
2. | Mean Operating Time | 90 to 150 minutes | 80 to 120 minutes |
3. | Prolonged Operating Time (≥120 minutes) | 06 | 00 |
4. | Severe haemorrhage & Requirement of Blood Transfusion | 00 | 00 |
5. | Procedural difficulty in -
|
03 08
03
08 |
04 05
06
02 |
6. | Other Complications (Anaesthetic difficulties, Airway compromise etc.) | 00 | 00 |
| |||
|
| Preauricular Approach (Gp ‘A’) | Retromandibular Approach(Gp‘B’) |
1. | Pain at Optd site | 02 | 06 |
2. | Hematoma, Edema & Swelling | 01 | 05 |
3. | Infection / Wound Dehiscence at Optd site | 00 | 04 |
4. | Salivary fistula formation | 00 | 02 |
5. | Sialocoele formation | 00 | 02 |
6. | Neurological deficits (Facial Nerve, Greater Auricular nerve, Auriculotemporal Nerve, Temporal or Marginal mandibular divisions of Facial Nerve) | 03 Cases (Transient paresis Temporal division of Facial Nerve) 12 Cases (Transient Auricular & Preauricular hypoesthesia due to involvement of branches of the Auriculotemporal / Greater Auricular nerve, which resolved spontaneously after 2-3 months) | 11 Cases (Transient weakness of Marginal mandibular branch of Facial Nerve) 02 Cases (Transient weakness of all branches of Facial Nerve) |
7. | Unesthetic visibility of Scar of Incision | 03 | 02 |
8. | Hypertrophic Scar | 01 | 02 |
9. | Frey’s Syndrome | 00 | 00 |
10 | Seroma | 00 | 00 |
11 | Condylar head resorption | 00 | 01 |
12 | Implant Failure: Screw loosening; Plate bending / fracture / exposure necessitating implant removal
| 00 | 00 |
| |||
| Preauricular Approach (Gp A) | Retromandibular Approach(Gp B) | |
1. | Occlusion (Unstable/ Deranged) | 01 | 02 |
2. | Persisting Uni- or Bilateral Open Bite | 00 | 00 |
3. | Dental & Mandibular midline shift | 01 | 02 |
4. | Radiographic evaluation- Unsatisfactory precision in repositioning, alignment & approximation of fractured fragments | 03 | 01 |
5. | Radiographic evidence of persisting Ramal foreshortening or asymmetry | 00 | 00 |
6. | Smooth & Bilaterally Synchronous movement of Condyles | 21 | 47 |
7. | Mandibular deformity / Facial asymmetry | 00 | 00 |
8. | Bone resorption / Condylar necrosis
| 00 | 01 |
| Preauricular Approach (Gp A) | Retromandibular Approach(Gp B) | |
1. | Perception of teeth not occluding / meeting equally bilaterally | 01 | 02 |
2. | Pain & Discomfort at Operated site | 04 | 06 |
3. | Clicking / Popping / Grating sounds in the TMJ region on opening or chewing | 01 | 02 |
4. | Pain or Difficulty in mouth opening
| 01 | 05 |
| Preauricular Approach (Gp A) | Retromandibular Approach (Gp B) | |
1. | Deranged Occlusion | 00 | 00 |
2. | Premature Occlusal Contacts | 01 | 03 |
2. | Unsatisfactory Masticatory Efficiency | 01 | 02 |
3. | Restriction in Mandibular movements - Jaw opening & Excursive movements (lateral & protrusive) | 01 | 05 |
4. | Jaw deflection / deviation on opening or chewing | 00 | 01 |
5. | Temporomandibular Dysfunction persisting beyond 3 months | 01 | 00 |
7. | Unstable Fixation | 00 | 00 |
8. | Mean Maximum Interincisal Mouth opening | 44mm | 47mm |
9. | TMJ Ankylosis | 00 | 00 |
Table 4: Comparison of the Complications encountered and Treatment Outcomes (Subjective, Objective & Functional) achieved following ORIF of 70 Surgeries of Condylar Head and Neck fractures, using two different Surgical Approaches.
Management of condylar process fractures is an interplay of three factors, namely, the nature and magnitude of injury, patient’s choice of treatment (surgical / non-surgical) and operator’s expertise. Severe cases with displacement or dislocation of the fractured fragments, as described our study, are indicated for an ORIF procedure.
Minor or non-displaced, non-dislocated condylar process fractures suggest the presence of periosteal support for stability and hence may not require open treatment [10, 11]. Where indicated, ORIF has been found to provide better functional reconstruction of mandibular condylar fractures than closed reduction and maxillomandibular fixation [12, 13, 14,15]. It prevents development of undesirable long-term effects such as shortening of the mandibular ramus, mandibular deformity, facial asymmetry, osteoarthritis, ankylosis and masticatory and articular dysfunction [16, 17, 18]. In contemporary practice, in addition to displaced and dislocated condylar process fractures, which could be condylar head (diacapitular), condylar neck (above the sigmoid line, or subcondylar (below the sigmoid line) fractures, all those fractures with a deviation of more than 10o, or a shortening of the ascending ramus by more than 2 mm, are recommended to be treated with open reduction and fixation, irrespective of level of the fracture [12].
Surgical approach is an important variable which influences and determines the treatment outcome. An ideal surgical approach enables the operator to gain sufficient exposure and access to the fracture site in order to effectively debride, retrieve, reduce and fix the fracture fragments. Although theoretically, it might appear to be a simple decision, the actual procedure of choosing an ideal surgical approach for each individual case requires careful consideration of a number of factors.
In our experience the Preauricular approach was found to provide an easier access to the condylar head / intracapsular / diacapitular fractures as well as high condylar neck fractures (Fig 1, 5, 6, 10 & 11). A second smaller incision may however be required below the angle of the mandible for drawing a braided wire through the bone for inferior traction, to aid locating and retrieving the dislocated and displaced proximal condylar fragment, if this cannot be achieved by using an interdental mouth prop. This approach was also found useful for exploring the injured / deranged soft tissues in the TMJ region, restoring a displaced articular disc to its proper position, and repairing it and the fibrous capsule in cases where they were torn.

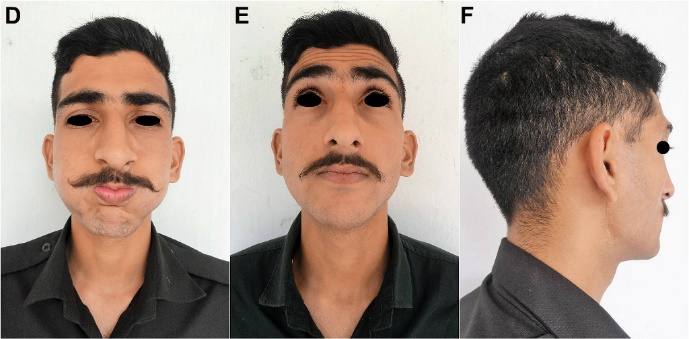
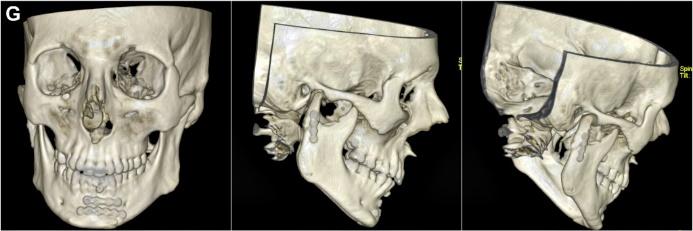

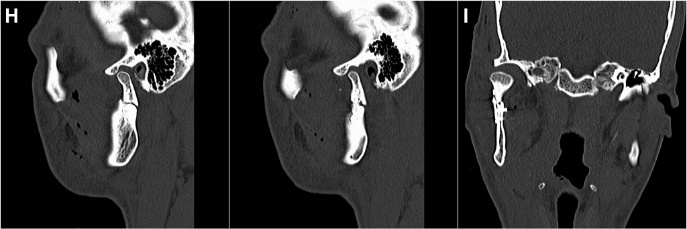

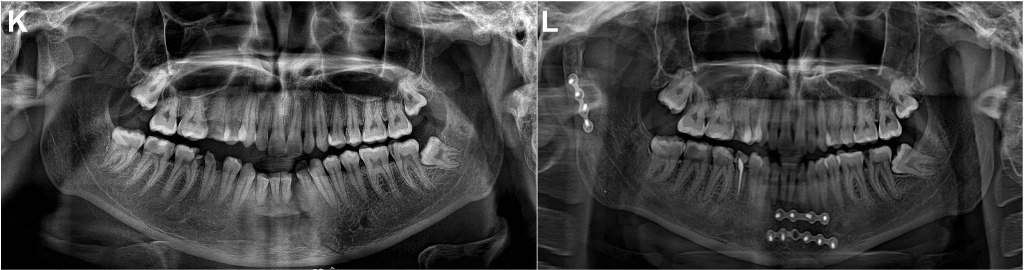
Fig 4: (Case 2) (A-F) Restoration of stable occlusion and normal mouth opening, with nil neurological deficits and a barely perceptible incision scar. (G-J) Post-surgery NCCT showing stable fixation of the left parasymphyseal fracture, and good realignment and fixation of the displaced & dislocated right condylar fracture. Achievement of bony continuity evident along posterior border of ramus, condylar neck & head, and the sigmoid notch. (K,L) Pre- and postoperative OPGs showing successful reduction, reapproximation and fixation of the fractures.

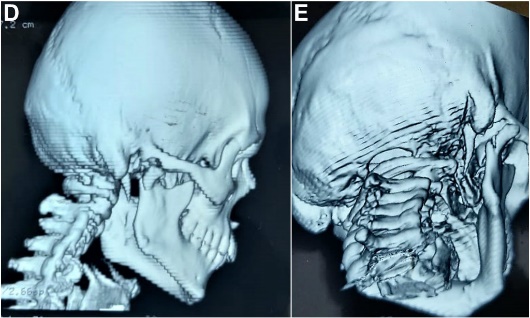
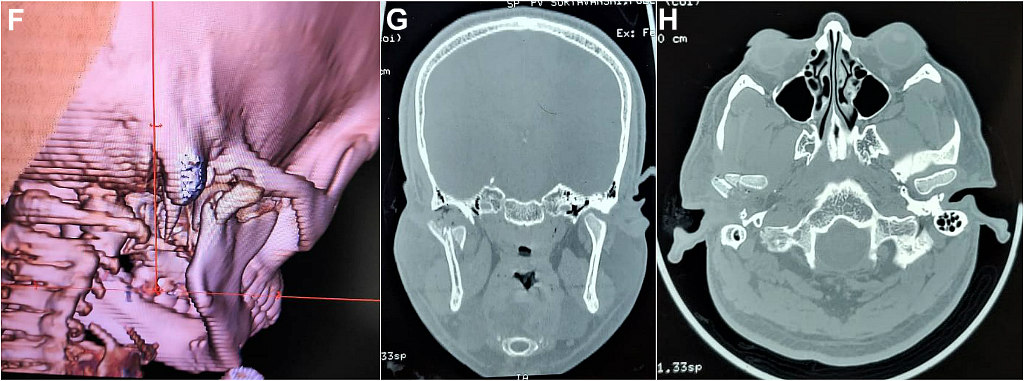

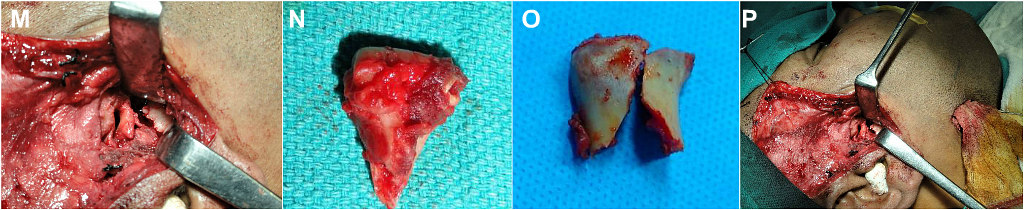
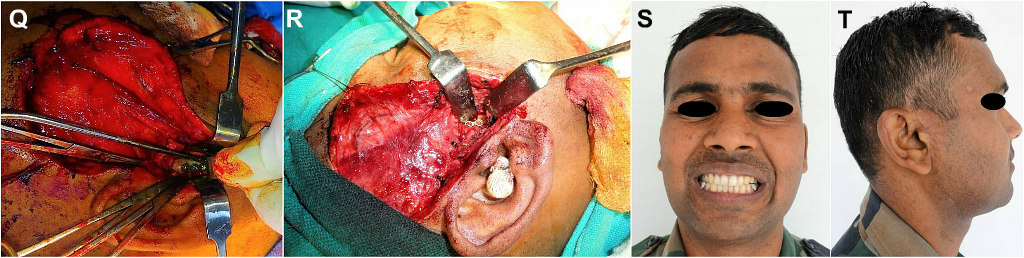

Fig 5: (Case 3) (A-C) Right condylar head fracture in a 30yr old male. (D-H) NCCT showing displaced and dislocated right condylar head, with a vertical/sagittal fracture running through it separating it into a smaller lateral and larger medial fragment. (I-M) Preauricular approach for retrieval of condylar head. (N-R) Larger, medial pole fragment flipped sideways and fixed to ramal stump, restoring ramal height. (S-U) Stable postoperative occlusion, normal mouth opening, well camouflaged incision scar. (T-W) NCCT showing stably fixed condylar fracture, with continuity at posterior ramal border and sigmoid notch.
The Preauricular approach was found to have three limitations. Firstly, there could be intraoperative haemorrhage, which usually results from accidental injury to, or severance of the superficial temporal vessels, transverse facial artery or the internal maxillary artery. Secondly, during fixation of condylar neck fractures, hardware / implant (minibone plates and screws) placement is sometimes difficult, often entailing excessive inferior traction of the soft tissues while fixing the distal screws, because of poor inferior exposure of the mandibular ramus. This occasionally results in transient deficit of the temporal or zygomatic branches of the Facial nerve. Thirdly, the preauricular approach is unable to provide adequate surgical access to low condylar neck or sub sigmoid / subcondylar fractures.
The Retromandibular approach, on the other hand, gives better access and exposure of the distal condylar neck and ramal area, and is therefore better suited for the low condylar neck/ subsigmoid /subcondylar fractures (Fig 1, 3, 8 & 10). This approach, almost directly overlying the upper ramus, needs to traverse less distance in dissection, and is hence ideal for these injuries, allowing a direct access for visualization, reduction, and fixation. It allows an easier application and adaptation, with screws placed at 90◦to the bony surface, giving maximum mechanical advantage. However, fixation of the proximal (upper) screws sometimes entails excessive upward traction of the soft tissues, occasionally resulting in transient paresis of the marginal mandibular, buccal and zygomatic branches of the Facial nerve. Unlike the preauricular approach, this approach provides limited access to the condylar head and upper neck, thereby making it unsuitable for the intracapsular/ diacapitular fractures especially when in-situ fixation is attempted. The approach may however be useful to a certain extent for mid/ high condylar neck fracture if an extracorporeal fixation is opted (Case 5, Fig 8). Intraoperative haemorrhage is another limitation of this approach, which can ensue from injury to the retromandibular vein.

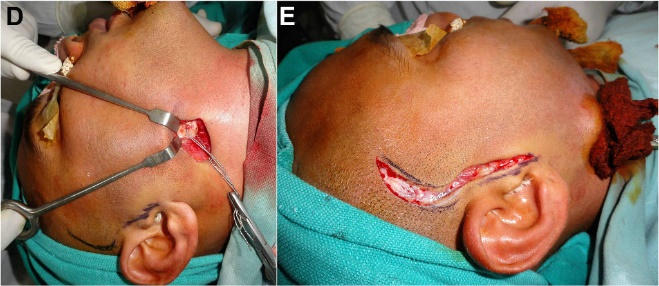
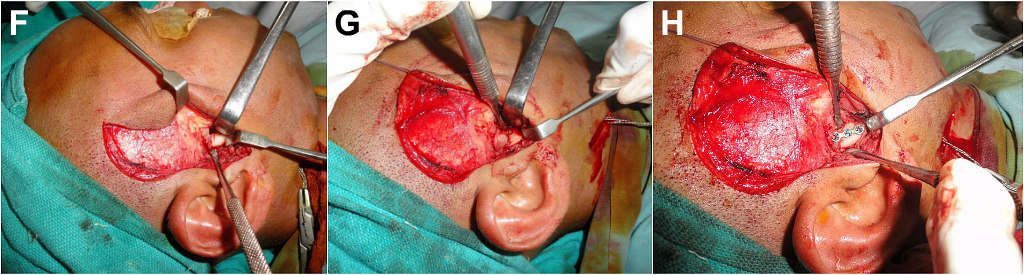

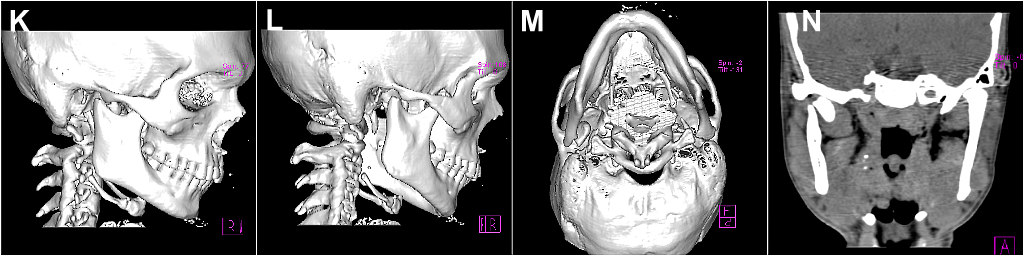
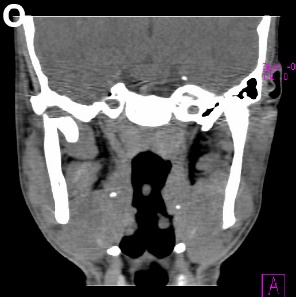
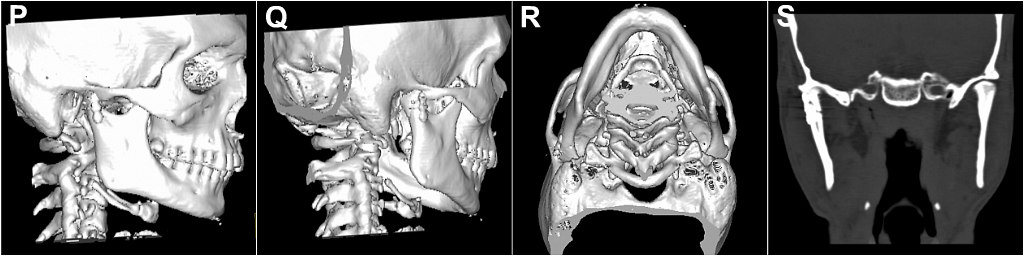
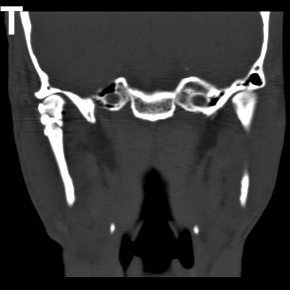


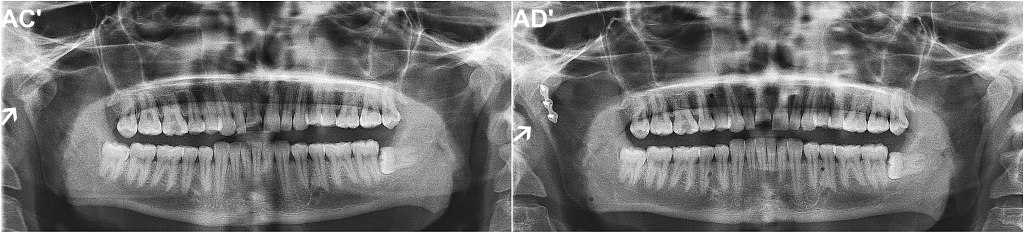
Fig 6: (Case 4) (A-C) 23 yr old patient with right condylar fracture. (D) Braided wire threaded through right angle of mandible to aid inferior traction. (E-J) Preauricular approach exposing ramal stump. Medially dislocated condylar head retrieved, repositioned and fixed. (K-O) Preoperative NCCT showing dislocated right condylar head lying upside-down, medial to ramal stump. (P-T) Postoperative NCCT showing precise repositioning and fixation of condylar head, restoring mandibular symmetry &ramal height. (U-X)(Y-AB’) Pre-& postoperative axial sections and TMJ views. (AC’-AD’) Pre-& postoperative OPGs.

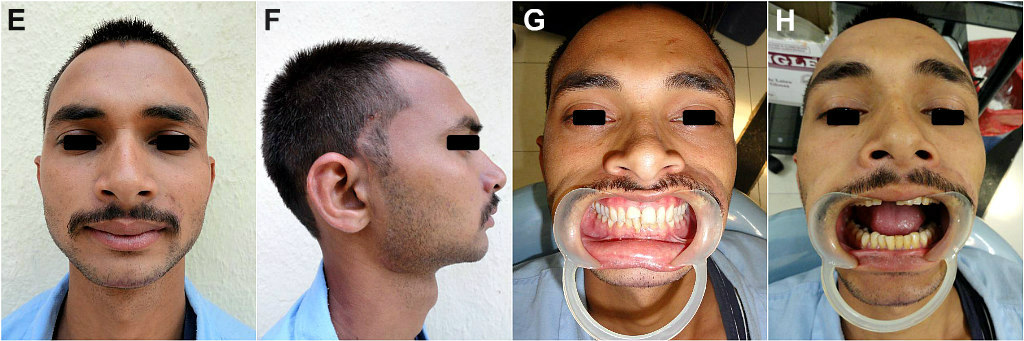
Fig 7: (Case 4) (A-C) Early Post-operative photographs showing absence of forehead wrinkling on the right side, indicative of a mild neurological deficit involving the frontal division of the Facial nerve, possibly attributable to intraoperative traction injury of the nerve filaments. (D) Well healing scar of the preauricular incision. (E-F) Barely perceptible incision well within the hairline, and camouflaged by the preauricular skin crease. Restoration of a stable occlusion and normal interincisal mouth opening.
Inadvertent injury to the Internal Maxillary Artery or the Inferior alveolar artery, while attempting to retrieve a medially displaced condylar fragment by either of the approaches, can also be a cause of worrisome intraoperative haemorrhage. However, in our study, no major incidence of haemorrhage or blood loss was encountered intraoperatively, which could be attributed to a meticulous surgical technique, careful dissection and timely identification and ligation / cauterisation of vessels in the operative field.
Three out of the fifty-six cases in our study presented with postoperative infection. All three were road traffic accident cases, with other associated mandibular fractures. The post-operative infection in these cases could be attributed to contamination during injury or the presence of the other concomitant fractures, which were treated by an intraoral approach in the same procedure as the condylar surgery [21]. The infections were mild, easily managed and resolved quickly with postoperative injectable antibiotics.
Condylar head resorption was observed approximately 13 months following surgery in one patient of Group B, in whom extracorporeal fixation of the condylar process as a free graft had been carried out. The condylar head resorption could be attributed to the loss of viable blood supply to the proximal fragment.
The use of two mini bone plates with mono or bicortical screws have been advocated for improved mechanical stability in ORIF of condylar fractures [22, 23]. In our study, it was not always possible to fix two plates, due to the limited bone available at the fracture sites, especially in cases of condylar head and high neck fractures. Nevertheless, it was found that that single plate fixed at these regions provided the required stability, and allowed good bony union, with no late post-operative complications. Ease in carrying out internal fixation differed significantly between the two groups. The relatively wider surgical field and a near straight line access to the fracture site in the retromandibular approach permitted easy miniplate osteosynthesis, as the drill, screws and screw driver could be positioned exactly perpendicular to the bone surface instead of obliquely. In the preauricular approach, placement of the lowest / most distal screw on the plate was often difficult and time consuming, and entailed significant soft tissue retraction, with resultant traction injury to the temporal and zygomatic branches of the Facial nerve.
Our experience with two cases paediatric condylar trauma have been described in this study (Case 5, Fig 8). One case of extracorporeal fixation in an 8-year-old child with a sagittal split through the left condylar head, was managed successfully by surgical retrieval of the condylar fragments, fixation of the fragments together and reconstituting the whole condylar head, and then repositioning the reconstructed head within the glenoid fossa (Fig 8). Open Surgical intervention in this case helped obviate the likelihood of future ankylosis and assured an unhindered mandibular growth in the young child. The second case was that of a 12-year-old child managed conventionally by the Retromandibular approach. Until recently, medical literature has stated that mandibular condylar fractures in patients younger than 12 to 14 years should not be treated surgically. This assertion was based on the intrinsic healing potential of the growing condyle, which was believed to lead to good functional healing, even with non-surgical management [25]. While this concept certainly holds true for incomplete, green-stick fractures, intra-articular fractures, and those with minimal displacement, we propose that much better results can be achieved with surgical treatment in fractures with major displacement and dislocation or loss of contact between bony stumps.
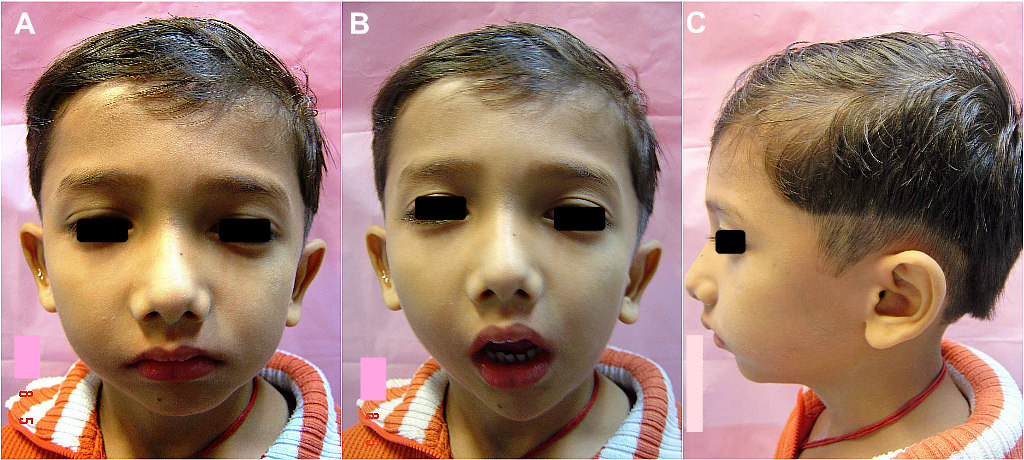
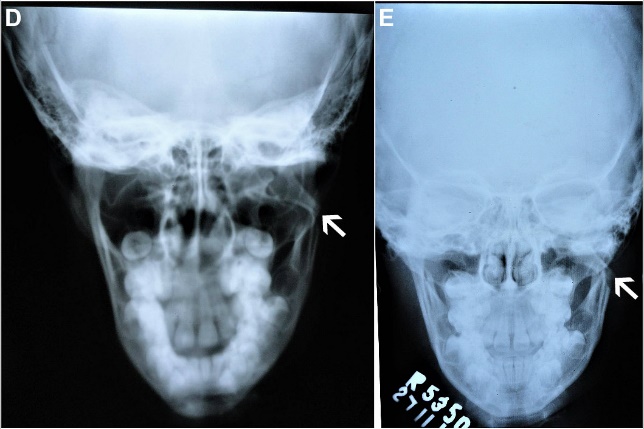

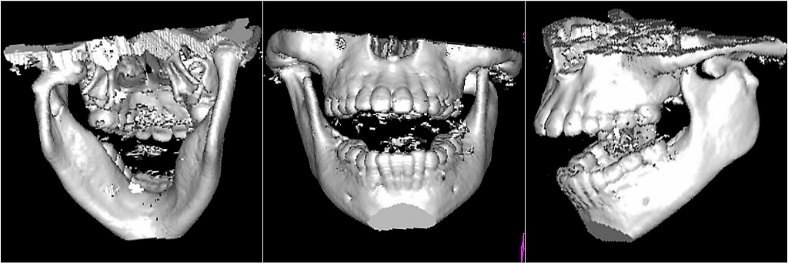


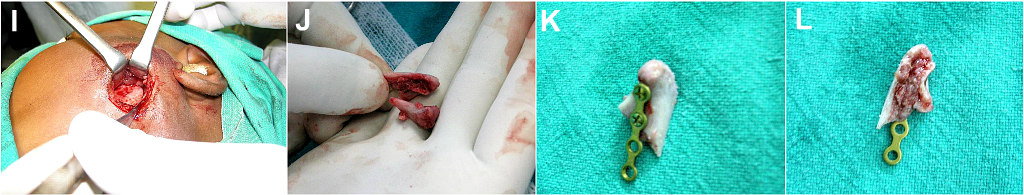


Fig 8: (Case 5) (A-C) 8yr old child with left condylar neck fracture. (D-H) Radiographs and NCCT showing the medially deviated condylar neck fracture, with a sagittal split through the dislocated condylar head. (I-J) Retromandibular approach to expose ramal stump and retrieve the medially displaced condyle head fragments. (K-M) Condylar fragments fixed together extracorporeally. (N-P) Reconstructed condyle fixed to the distal ramal segment by screws through the two lower holes of the miniplate. (Q) Occlusion restored. (M,N) Postoperative radiographs showing successfully realigned condylar fracture.
In the cases of the Retromandibular Transparotid approach (Group B), breach of the parotid gland capsule and subsequent dissection through the gland parenchyma, or disruption of the ductal system sometimes resulted in a sialocoele or fistula formation. In this study, two cases of salivary fistula and two cases of sialocoele formation were observed among the patients. These complications could probably have been avoided by a more watertight closure of the capsule following surgery. The two patients with sialocoele formation were treated conservatively by the application of occlusive / compression dressings and administration of antibiotics and anti-sialagogues, and resolution was seen 15 to 20 days after surgery. A silastic drain was used for each of the patient with salivary fistula, and was removed on the 10th day after complete resolution of salivary leakage.
Neurological deficits were found to be marginally more with the retromandibular approach, with transient paresis of the marginal mandibular division of the Facial nerve observed in 11 cases, due to traction injury to the nerve. However, the temporary weakness reversed spontaneously within three months of surgery. Deficit of the Facial nerve affecting all its branches, was encountered in one case operated using the Retromandibular approach. Resolution was slow, but complete at 5 months following the surgery. Paresis of the Temporal division of the Facial nerve was encountered in three of the cases operated using the Preauricular approach (Fig 7, Case 4), which too were transient and reversed spontaneously a month following surgery. Vitamin B complex, methylprednisolone, and methcobalamine was prescribed to these patients, to promote and hasten recovery of the injured nerve function. Auricular Paraesthesia / anaesthesia was noted in 50% of the patients operated using the Preauricular approach. This seems in accordance with previous studies on comparison of different surgical approaches for Condylar process fractures [24]. However, this was not troublesome and patients did not notice or complain of the altered sensation in the preauricular region, which spontaneously resolved over a period of three to six months.

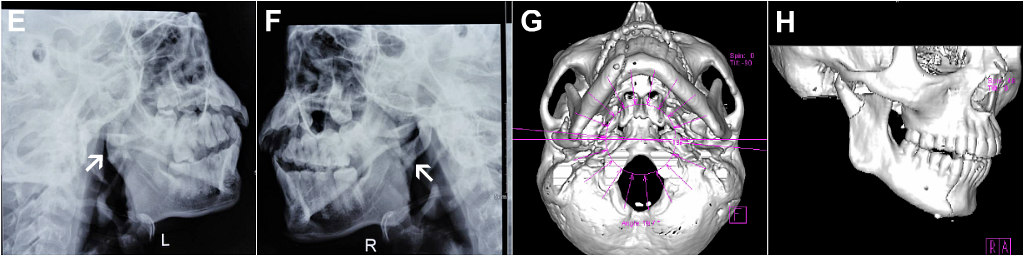
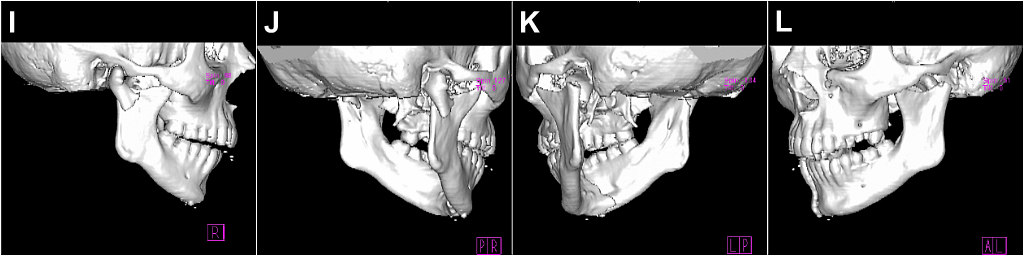

Fig 9: (Case 6) (A-C) 24 yr old male with bilateral condylar fracture. (D-F) Radiographs showing bilateral condylar neck fractures (white arrows) and right parasymphysis fracture. (G-P) NCCT showing laterally displaced low right condylar neck fracture and a medially displaced high left condylar neck fracture, with dislocation of both condylar heads. Right condyle seen lying against the lateral surface of the ramal stump, and left condyle seen lying medial to the ramal stump, in the infratemporal fossa.
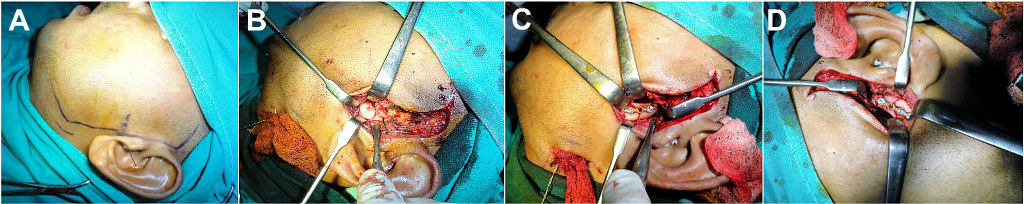



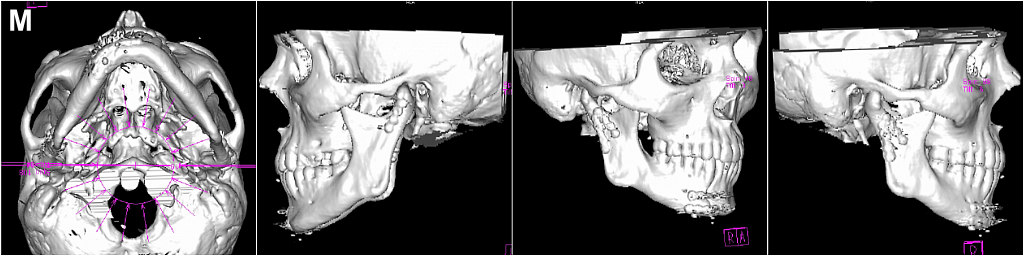

Fig 10: (Case 6) (A-G) Left preauricular and right retromandibular approaches to expose, reposition and fix the left, high and right, low condylar neck fractures respectively. (H) ORIF of parasymphyseal fracture via an intraoral vestibular approach. (I-L) Postoperative radiographs showing precise realignment and fixation of the bilateral condylar neck fractures and right parasymphyseal fracture of the mandible. (M,N) Postoperative NCCT showing precisely reduced and fixed bilateral condylar neck fractures, with successful restoration of the dislocated condylar heads back within their glenoid fossae.
In this study, it was found that the Retromandibular approach left a slightly more aesthetically acceptable scar than the Preauricular approach. The scar of incision was placed in a skin crease behind the posterior border of the ramus, which was barely visible four months after surgery (Fig 2F, 4). The Preauricular incision scar, although also located in a skin crease in front of the ear, and found acceptable by all patients, was slightly more visible and noticeable as it was on the face. Its temporal extension was always well camouflaged within the hairline (Fig 2, 5, 7 & 12). Careful placement of a skin incision is important to have a less perceptible, camouflaged scar.

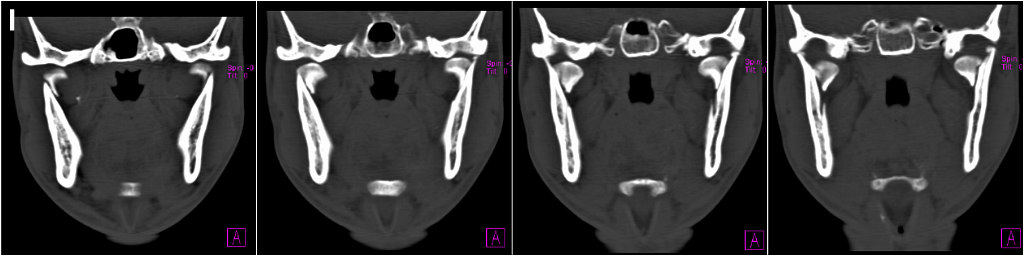
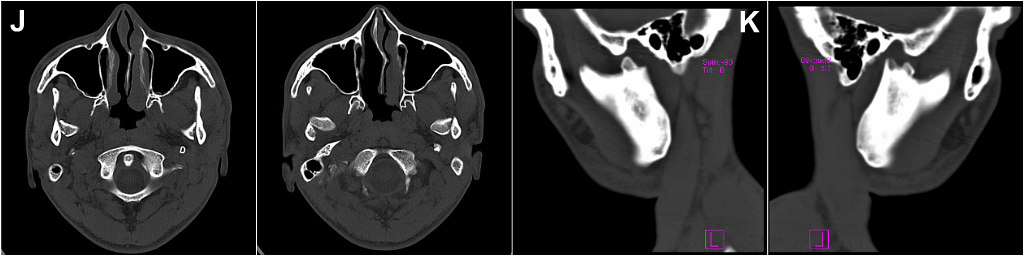

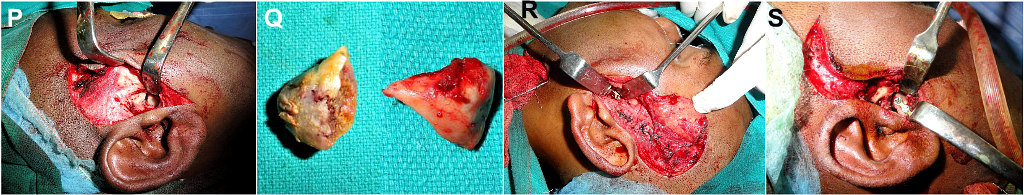
Fig 11: (Case 7) (A,B) 25 yr old male with bilateral condylar fractures. (C-K) NCCT showing comminuted symphyseal and bilateral condylar head fractures. A bilaterally symmetrical pattern of dislocation of the condylar heads out of their glenoid fossae and their uniform positioning against medial surfaces of the ramal stumps, was observed. (L,M) ORIF of symphyseal fracture. (N-S) Preauricular approach employed on both sides, to retrieve the medially dislocated condylar heads, which were then fixed to the ramal stumps as free grafts, thus restoring ramal height.
Functional outcome following surgery, was similar in both groups. Irrespective of the surgical approach employed, good approximation and alignment of the fracture fragments with stable fixation was achieved. Bilaterally smooth and synchronous condylar movements were achieved post operatively in all cases, with unrestricted mouth opening and mandibular excursive movements with optimum masticatory efficiency. There was no residual mandibular deviation or deformity in any of the cases.


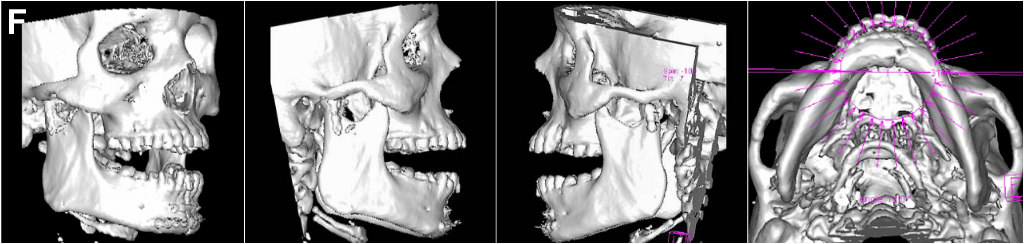
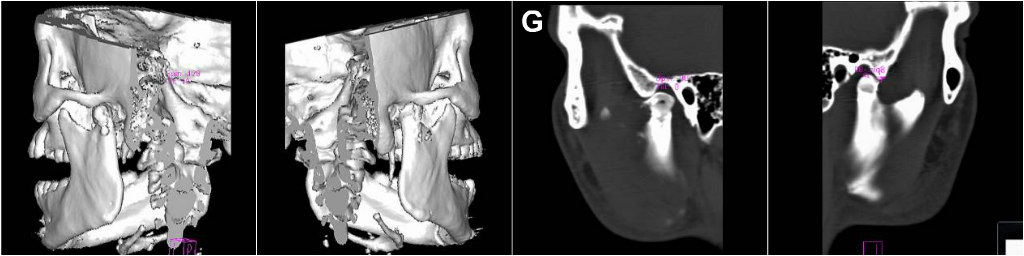
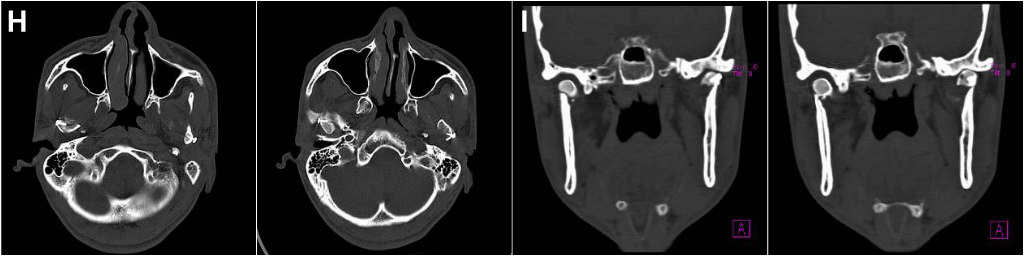
Fig 12: (Case 7) (A-E) Restoration of stable occlusion and normal interincisal mouth opening. Well healed and barely noticeable scars of the preauricular incisions. (F) Postoperative NCCT showing stable fixation of condylar heads to ramal stumps bilaterally, with restoration of lost ramal height. (G-I) Sagittal, axial and coronal sections showing successful repositioning of the medially displaced and dislocated condylar heads back within their glenoid fossae and in alignment with the ramal stumps bilaterally.
Both the Preauricular-Retroparotid as well as Retromandibular-Transparotid surgical approaches were found to be clinically effective when meticulously employed in correctly indicated cases, in achieving good aesthetic as well functional results. Depending upon the level of the condylar fractures, a preauricular approach is ideal for the condylar head and high condylar neck fractures, providing direct and easy visualization to the region, for retrieval and repositioning of the medially displaced and dislocated proximal fracture fragment. The retromandibular approach is more suited for the lower level condylar neck fractures, providing a direct visual field and a wide, straight line access for implant fixation at this region.
Both techniques are safe, and with careful case selection, yield comparable results with a low complication rate. A meticulous operative technique, with care taken to carefully identify and preserve anatomic structures such as nerves and vessels in the respective operative fields, goes a long way in preventing complications such as intraoperative haemorrhage and post-operative neurological deficits. Careful attention to detail and precise anatomic reduction, alignment and stable fixation of the fracture fragments yield good functional and aesthetic outcomes with minimal morbidity.
Disclosure of potential Conflicts of Interest:
The authors of this article has not received any research grant, remuneration, or speaker honorarium from any company or committee whatsoever, and neither owns any stock in any company.
The authors declare that they do not have any conflict of interest.
Research involving human participants and /or animals:
All procedures performed on the patients (human participants) involved were in accordance with the ethical standards of the institution and/or national research committee, as well as with the 1964 Helsinki declaration and its later amendments and comparable ethical standards.
Ethical approval: This article does not contain any new studies with human participants or animals performed by the author.
Informed Consent: Written Informed Consent was obtained from all the individual participants in this study.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
