AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Andrey Belousov, Kharkiv National Medical University, Ukraine.
Citation: Andrey Belousov, (2024), Comparing Drug Handling Efficiencies and Expenses for Short-Acting Granulocyte-Colony Stimulating Factor Injection Originators and Biosimilars from the Perspective of Hospital Resource Management in Formulary Decision-Making, J. General Medicine and Clinical Practice, 7(6); DOI:10.31579/2639-4162/141
Copyright: © 2024, Andrey Belousov. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 08 January 2024 | Accepted: 21 March 2024 | Published: 27 March 2024
Keywords: anticoagulants; antiplatelets; thrombosis; hemostasis assessment; regulation
Statement of the Problem: Impairment of the blood coagulation system remains a relevant issue in clinical practice. A striking example of this is the fact that despite the administration of anticoagulant therapy, up to 35% of COVID-19 patients were hospitalized in the intensive care unit with thromboembolic complications. Prophylactic and therapeutic methods for the hemostatic system, recommended by various protocols, have a general nature. Moreover, they introduce dissonance into the clinical clarity of appropriate anticoagulant and antiplatelet use and fail to provide practitioners with the necessary fundamental knowledge to understand the aspects of clinical tactics for correcting the hemostatic system. Uncertainties remain regarding how to correctly choose a specific anticoagulant and determine its effective dose based on individual clinical and laboratory data, which laboratory markers of the coagulation system should be investigated, and whether they always reflect the true picture of hemostasis. Methodology and Theoretical Orientation: This article briefly presents the main aspects of the functioning of the blood coagulation system, points of application for pharmacological agents, and provides objective information for clinicians about the mechanisms of action of major anticoagulants and antiplatelets. Effective and practical methods for assessing the hemostatic system are recommended. Findings: The proper correction of the hemostatic system can only be carried out by a highly qualified specialist - a clinical transfusiologist, who possesses a comprehensive understanding of the functioning of the coagulation and anticoagulation systems, the platelet and fibrinolysis systems, knows the points of application and mechanisms of action of the pharmacological agents and blood components used, and takes into account internal and external factors that influence hemostasis. Conclusion and Significance: Empirical prescription of anticoagulant and antiplatelet therapies, based solely on instructions and clinical protocols without objective comprehensive analysis of the hemostatic components, is not only ineffective but also life-threatening for the patient. Cholangiogram and D-dimer measurements cannot serve as the sole determining markers for monitoring the coagulation system. Evaluation of the blood coagulation system should only be carried out based on a comprehensive analysis of cholangiogram data, complete blood count, thromboelastographic (TEG), and data from all relevant systems
Statement of the Problem. Despite the availability of a wide variety of anticoagulants and antiplatelet agents in the market, the impairment of the blood coagulation system remains a relevant issue in clinical practice. One example of this is the numerous publications dedicated to the novel coronavirus infection (COVID-19), which, despite the administration of anticoagulant therapy, often leads to systemic activation of blood coagulation and thrombotic complications [1–4]. Initial studies of COVID-19 patients demonstrated a high frequency of venous thromboembolism, including pulmonary embolism (PE). Despite receiving anticoagulant therapy, up to 35% of COVID-19 patients required admission to the intensive care unit due to thromboembolic complications. Severe complications of COVID-19 were associated with disturbances in coagulation processes and characterized by elevated levels of D-dimers and fibrinogen. An increased risk of developing PE was observed, which directly contributed to the death of approximately 30% of patients with COVID-19 [5].
In a prospective observational study by J. Helms et al., PE was observed in 16.7% of patients despite receiving anticoagulant therapy [6]. Interestingly, there were no signs of deep vein thrombosis or other sources of thromboembolism. According to the findings of R. Beun et al. (Netherlands), among 75 patients admitted to the intensive care unit (ICU), the incidence of PE was 26.6% [7]. In the study by J. Poissy et al., out of 107 patients hospitalized in the ICU and receiving anticoagulant therapy, 22 (20.6%) developed PE [8]. In a retrospective cohort study conducted by F.A. Klok et al., among 184 patients admitted to the ICU, PE occurred in 13.6% of patients despite receiving anticoagulant therapy [9]. According to a systematic review and meta-analysis by L. Roncon et al., conducted on a sample of 7178 COVID-19 patients, the overall frequency of thromboembolic complications (PE) among those hospitalized in general wards and ICUs was 14.7% and 23.4%, respectively [10].
Currently, several different pathophysiological mechanisms are considered to contribute to the development of PE in patients with COVID-19, including increased systemic inflammatory response, disruptions in the hemostatic system, the development of pulmonary intravascular coagulopathy, and endothelial dysfunction [11]. A study by H. Han et al. conducted at Wuhan University (China, 2020) confirmed the development of a hypercoagulable state in patients with COVID-19, characterized by elevated levels of D-dimers, fibrinogen, and fibrinogen degradation products [12]. M. Oudkerk et al. suggest that the high level of D-dimers observed in COVID-19 patients is a consequence of systemic inflammation and reflects the true thrombotic state induced by the virus [13]. Sakr Y. et al. (2020) believe that the thrombosis occurring in COVID-19 patients despite anticoagulant therapy is a result of insufficient data on the epidemiology and pathophysiological mechanisms obtained from randomized clinical trials [14]. Meanwhile, Z. Zhai et al. (2020) recommend the use of low molecular weight heparins (LMWH) as first-line therapy for patients with mild or moderate COVID-19 who have a high or moderate risk of developing PE. The duration of prophylactic therapy should be at least 7-10 days or continued until the elimination of venous thrombosis risk factors [15].
The American Society of Hematology (ASH) and the International Society on Thrombosis and Haemostasis (ISTH) recommend the administration of prophylactic doses of LMWH (4000 IU twice daily) to all hospitalized patients with confirmed diagnosis of COVID-19. Pharmacological prophylaxis with LMWH is recommended as the first-line approach for patients with low or moderate risk of bleeding and no contraindications to antithrombotic agents. In cases of severe renal insufficiency (creatinine clearance <30>
The choice of the appropriate medication and correct dosage requires taking into account comorbidities such as renal or hepatic dysfunction, thrombocytopenia, and gastrointestinal conditions. As a first-line therapy, Z. Zhai et al. recommend the use of parenteral LMWH, such as enoxaparin (100 IU/kg twice daily) or enoxaparin (150 IU/kg once daily) or nadroparin (86 IU/kg twice daily) [15]. The examples provided in the given information create dissonance and confusion in the clinical clarity of the proper use of anticoagulants and antiplatelet agents, as it fails to provide healthcare professionals with the necessary fundamental knowledge to choose the correct strategy for correcting the hemostatic system. Several important questions arise:
1. How to correctly choose a medication and determine its effective dosage considering individual clinical and laboratory data of the patient?
2. Which laboratory and instrumental methods of investigation reflect the true state of hemostasis?
3. Is it accurate to assess the hemostatic condition based solely on coagulation profile and D-dimer levels?
These questions highlight the need for providing objective information to clinicians in order to ensure the proper and effective use of anticoagulants and antiplatelet agents.In clinical practice, drugs that affect the blood coagulation system are widely used by physicians of various specialties, often as part of comprehensive therapy and symptomatic treatment. However, in order to effectively and appropriately utilize such medications, it is imperative to possess profound knowledge regarding the functioning of the coagulation and anticoagulation systems, fibrinolysis mechanisms, the influence of the body's internal environment in maintaining their balance, and a comprehensive understanding of the overall pharmacological effects of the drugs employed. Proper use of hemostatic agents is impossible without adequate assessment of the blood coagulation system and a balanced, comprehensive approach to therapy. Ignoring this fact increases the risk of serious complications related to disruptions in the blood coagulation system, which can be life-threatening for the patient.
The objective of this study is to provide clinicians with objective information on the mechanisms of action of major types of anticoagulants and antiplatelet agents, based on fundamental knowledge of the functioning of the blood coagulation system. Additionally, the study aims to recommend effective methods for assessing the state of the hemostatic system.
Methodology and Theoretical Orientation.
Factors Influencing the Development of Venous Thrombosis. Key Causes of Thrombosis in COVID-19.
The occurrence of venous thrombosis can be attributed to various factors, which are encompassed by Virchow's triad [16]:
- reduced blood flow velocity;
- endothelial dysfunction;
- activation of the blood coagulation system.
With the emergence of COVID-19, Sakr Y. et al. (2020) presented their concept of hypercoagulability pathogenesis in this disease [17]. The main causes of blood coagulation abnormalities are as follows:
1.Severe hypoxia, associated comorbidities, and organ dysfunction predispose individuals to hemostatic disturbances. Hypoxia increases blood viscosity, thereby promoting thrombosis.
2.Endothelial dysfunction, elevation of von Willebrand factor, toll-like receptor activation, and tissue factor activation can induce proinflammatory and procoagulant effects through complement activation and cytokine release. This leads to dysregulation of the coagulation cascade, resulting in the formation of pulmonary intravascular or systemic thrombi.
3.he "cytokine storm" induces secondary development of hemophagocytic lymph histiocytosis with coagulation activation, increasing the risk of intravascular micro thrombosis and secondary coagulopathy, which contribute to the occurrence of thromboembolism.
It should be noted that the presented list of thrombogenesis causes in COVID-19 by Sakr Y. et al. is pathogenetically predictable and fully aligns with the classical Virchow's triad. The development of systemic endothelial dysfunction in COVID-19 accounts for the loss of certain physiological properties of the endothelium, including its ability to stimulate vasodilation, fibrinolysis, and antiplatelet aggregation. Additionally, viral and cytokine-induced endothelial cell damage leads to excessive release of von Willebrand factor, triggering thrombus formation. Consequently, CT-pulmonary angiography reveals widespread cases of obliteration and thrombosis in small and medium-sized vessels, which are secondary manifestations of COVID-19 [18].
The Peculiarities of Using Various Types Of Anticoagulants And Their Points Of Application.
The implementation of anticoagulant therapy and the selection of anticoagulants should be based not on recommendations derived from controversial statistical data analysis of meta-analyses, subjective and constantly changing treatment protocols, but on objective, fundamental knowledge about the functioning of the hemostatic system, the pharmacological mechanisms of action of the drugs, and a personalized approach to assessing the state of the coagulation system. Let us begin by examining the points of application of major types of anticoagulants. The application points of major types of anticoagulants and their mechanisms of action are illustrated in Figures 1-4, based on the blood coagulation scheme developed by Paul Morawitz (1905) [19,20].
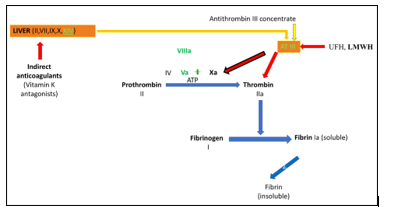
Figure 1. Points of application of indirect and direct anticoagulants.
Figure 1 illustrates that indirect anticoagulants inhibit the activation of prothrombin (II), proconvention (VII), antihemophilic globulin B (IX), and thrombotropin (X) by suppressing the reduction of Vitamin K1 epoxide, which are synthesized in the liver and play a crucial role in the formation of fibrin clots [21]. However, it should be noted that simultaneously, antagonists of Vitamin K hinder the activation of proteins C (XIVa) and S, which possess anticoagulant activity and are also synthesized in the liver. In light of this, practicing physicians should pay attention to the danger of hypercoagulation occurring within the first three days after initiating the administration of indirect anticoagulants (especially neodicoumarin). This is due to the fact that when indirect anticoagulants are prescribed, there is a more rapid decrease in the levels of proteins C and S, which have a shorter half-life compared to factors II, VII, IX, and X. Therefore, in acute situations (such as myocardial infarction, etc.), it is essential to administer heparin concurrently with Vitamin K antagonists in the first three days as a preventive measure against thrombosis. Ignoring this can lead to a decrease in the levels of proteins C and S, which can cause the development of so-called "coumarin" necroses in soft tissues (buttocks, mammary glands, cheeks, genitalia), resulting from capillary and small venule thrombosis. These necroses typically appear 4-10 days after starting the medication, more frequently in women. To address the onset of complications, transfusion of frozen blood plasma rich in protein C is performed [22].
Also, Figure 1 shows the points of action of unfractionated heparins (UFH) and low molecular weight heparins (LMWH). The difference in their action lies in the fact that UFH inhibits the activation of plasma factors II and X, while LMWH primarily inhibits the activation of factor X. Importantly, all heparins act indirectly on plasma factors through a protein mediator called antithrombin III. Antithrombin III is an anticoagulant protein, with the average reference values of normal ranging from 80% to 120%. Antithrombin III inactivates coagulation factors (IIa, VIIa, XIa, Xa, IXa, XIIa). Specific regions of heparins bind to the positively charged amino groups in the antithrombin III molecule. As a result, the reactivity of argil groups in antithrombin III increases. Interacting with the active sites of serine proteases (factors IIa, VIIa, IXa, Xa, XIa, XIIa), arginine groups of
antithrombin III inhibit the activity of plasma factors and prevent the formation of fibrin clots [23, 24]. Antithrombin III is primarily synthesized by the liver and vascular endothelium.
Therefore, practicing physicians should understand that in the presence of endothelial dysfunction and signs of liver dysfunction, situations may arise where the level of antithrombin III falls below 80%. In such cases, the use of heparins may become ineffective in the presence of clinical and laboratory signs of thrombosis. Thus, it becomes crucial and necessary to determine the level of antithrombin III in the blood through laboratory testing. If the level of antithrombin III is below 80%, the administration of heparins is not indicated. The level of antithrombin III can be increased through the transfusion of human antithrombin III concentrate ("Catenative") [25].
Another important aspect that clinicians should consider is that heparins belong to the class of proteoglycans. In response to their administration, the immune system can activate the production of antibodies against the heparin-calcium complex. This leads to the development of an immune type of heparin-induced thrombocytopenia (Fig.2). In immune type of heparin-induced thrombocytopenia, increased platelet aggregation occurs on days 9-14, along with thrombocytopenia (less than 50% of the baseline), decreased blood clotting time, and the presence of antibodies against the heparin-calcium complex in the blood [26]. The inability of clinicians to diagnose immune type of heparin-induced thrombocytopenia at early stages leads to erroneous tactics of increasing the dosage of heparins. Ultimately, this becomes the main cause of "rebound" thrombosis. It should be noted that the risk of developing "rebound" thrombosis is very high in patients with COVID-19. This is due to the fact that in many patients, viral-induced endothelial damage triggers an autoimmune inflammatory process [27]. Consequently, in the presence of heparin administration, typically on days 9-14, the clinical manifestation of venous thrombosis or pulmonary embolism rapidly occurs. In the event of clinical and laboratory signs of immune type of heparin-induced thrombocytopenia, heparin therapy should be immediately discontinued and replaced with fondaparinux. Fondaparinux belongs to the class of pentasaccharides and does not induce immune type of heparin-induced thrombocytopenia [28]. However, it should be noted that fondaparinux, similar to heparins, exerts its effects through antithrombin III, but unlike heparin, it exhibits selective action towards factor Xa.
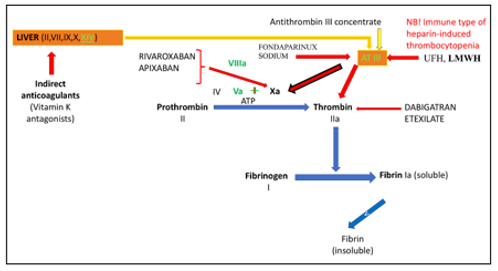
Figure 2. Development of heparin-induced thrombocytopenia in response to the administration of heparins. Figure 2 demonstrates that the action of heparins and fondaparinux requires antithrombin III [29]. In cases where it is not possible to determine the level of antithrombin III or if it is low, the following anticoagulants are prescribed - rivaroxaban, apixaban, and dabigatran.
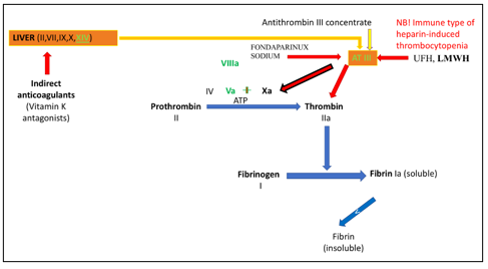
Figure 3 complements the points of application of these anticoagulants.
Figure. 3. Points of application of rivaroxaban, apixaban, and dabigatran. Unlike heparins and fondaparinux, these anticoagulants directly inhibit activated plasma coagulation factors without the need for the protein mediator antithrombin III [30]. The difference in their action lies only in the fact that rivaroxaban and apixaban target factor Xa, while dabigatran targets factor IIa. For the appropriate use of anticoagulants, clinicians should also have knowledge of the function of protein C. Protein C is an anticoagulant protein. Under the action of thrombomodulin on the surface of endothelial cells, protein C is converted into an active protease and, after interaction with protein S, exhibits pronounced anticoagulant activity. The main function of activated protein C is the hydrolysis of plasma factors Va and VIIIa, preventing the chain reaction of thrombin and fibrin formation [31]. For example, one of the causes of recurrent venous thrombosis in 20-50% of
cases is the mutation in factor V (known as Leiden mutation) [32]. In this case, the mutated factor V becomes resistant to hydrolysis by protein C. Therefore, clinicians must consider this fact when deciding on the discontinuation of anticoagulants.
Laboratory Screening and Monitoring of Anticoagulant Therapy.
The screening and monitoring of antithrombotic therapy are presented in Table 1.
Table 1 illustrates the points of action of major anticoagulants and laboratory screening indicators. Special attention should be given to rivaroxaban and apixaban. The effectiveness of their action is assessed by determining the prothrombin time (PT) using the Neoplastin kit and the anti-Xa calibration test [33].
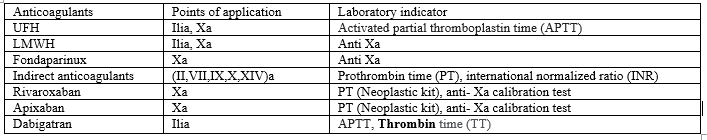
Table 1. Laboratory Screening and Monitoring of Antithrombotic Therapy.
Key Aspects of the Application of Various Antiplatelet Agents and Their Points of Application.
Antiplatelet agents are primarily used for the prevention and treatment of arterial thrombosis. The points of application for major types of antiplatelet agents are presented in Table 2.
Table 2 demonstrates the major types of antiplatelet agents based on their mechanism of action. Each of the presented antiplatelet agents has its own
points of application, indications, contraindications, and side effects. Typically, when deciding on the prescription of antiplatelet therapy, clinicians rely on clinical data, protocols, and pharmacological instructions for use. However, they do not consider the actual activity state of different types of receptors on the surface of platelets, nor do they objectively monitor their functions. Ultimately, this not only contributes to the low effectiveness of antiplatelet therapy but also becomes the main cause of life-threatening conditions for the patients.
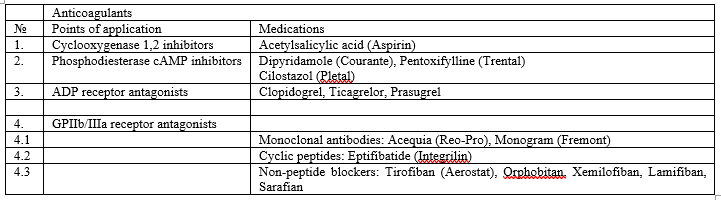
Table 2: Points of Application for Major Types of Antiplatelet Agents.
To address this issue, clinicians need to choose an effective and practical method for the objective assessment and monitoring of platelet aggregation function. One such method is Thromboelastographic (TEG). TEG allows for rapid and efficient monitoring of the state of key factors in the blood coagulation system. This method can provide an objective assessment of platelet aggregation function and enable clinicians to dynamically observe the measured parameters. Additionally, TEG can easily and quickly evaluate the effectiveness of different antiplatelet agents. However, it is important to note that the interpretation of TEG data should be performed by a qualified physician, specifically a clinical transfusion specialist. Among all the types of antiplatelet agents used, particular attention should be given to the mechanism of action of acetylsalicylic acid, which is commonly prescribed by practicing physicians for the prevention and treatment of arterial thrombosis, according to widely used protocols and recommendations [34]. Clinicians should be aware that the mechanism of action of acetylsalicylic acid is not straightforward. The pharmaceutical manufacturers provide only one aspect of the mechanism of action of acetylsalicylic acid in the product instructions, which is the inhibition of cyclooxygenases (COX), leading to a reduction in thromboxane A2 synthesis in platelets. In turn, thromboxane A2 stimulates the activation of new platelets and their aggregation by increasing the expression level of the glycoprotein complex GP IIb/IIIa on the platelet membranes. Circulating plasma fibrinogen binds to this complex, thereby strengthening the thrombus [35]. It is believed that platelets only contain COX-1 [36]. Therefore, COX-1 inhibitors reduce the synthesis of thromboxane A2 in platelets. Ultimately, this reduces the activity of thrombus formation. It was this one-sided spectrum of action that was the determining factor in prescribing acetylsalicylic acid.
However, it should be noted that acetylsalicylic acid does not belong to selective COX-1 inhibitors. In addition to COX-1, it inhibits COX-2 as well [35]. COX-2 synthesis occurs in macrophages, monocytes, fibroblasts, chondrocytes, and endothelial cells. As a result of COX-2 inhibition, the synthesis of prostacyclin is reduced. This contributes to the formation of arterial thrombi and increases the risk of thrombosis in patients in the "at-risk" group [37]. This mechanism also underlies the pathogenesis of reducing inflammation, pain, and fever when using acetylsalicylic acid. Many authors in their scientific publications, using traditional nonsteroidal anti-inflammatory drugs (NSAIDs) as an example, claim that simultaneous inhibition of the two isoenzymes, COX-1 and COX-2, does not disrupt the balance from a hemostatic perspective [38]. In this regard, a logical question arises: how does acetylsalicylic acid, which simultaneously inhibits both isoenzymes (COX-1 and COX-2), selectively provide an antiplatelet effect? A meta-analysis of data from 16 trials involving 171,215 individuals with an average age of 64 years revealed new evidence that casts doubt on the usefulness and effectiveness of low-dose aspirin for the prevention of cardiovascular events. It was shown that in the majority of patients who regularly took acetylsalicylic acid, the antiplatelet effect was completely absent [39, 40].
Such studies are not new. Previously, there has been a hypothesis that there are patients who are genetically insensitive to the action of acetylsalicylic acid. This hypothesis may only partially hold true. The balance of hemostasis depends not only on the activity of the drug to inhibit COX-1 and COX-2 but also on the quantitative content of polyunsaturated fatty acids (PUFAs), which are components of cell membrane phospholipids. Two classes of PUFAs are of practical interest to clinicians - omega-3 and omega-6. There are two main metabolic pathways for PUFAs - cyclooxygenase and lipoxygenase pathways (see Figure 4).

Figure 4. Scheme of eicosanoid synthesis from omega-6 and omega-3 PUFAs.
Figure 4 demonstrates that the cyclooxygenase pathway of PUFA metabolism leads to the formation of prostaglandins, prostacyclin, and thromboxane. The lipoxygenase pathway leads to the formation of leukotrienes. The key representative of omega-6 PUFAs is arachidonic acid (AA). Arachidonic acid is a polyunsaturated fatty acid present in the
phospholipids (especially phosphatidylethanolamine, phosphatidylcholine, and phosphatidylinositides) of membranes of the body's cells, and is abundant in the brain, muscles, and liver. The cyclooxygenase pathway of AA metabolism results in the formation of prostaglandins and prostacyclin of series 2, as well as thromboxane A2. The lipoxygenase pathway leads to the formation of leukotrienes of series 4. The key representative of omega-3 PUFAs is eicosapentaenoic acid (EPA). The cyclooxygenase pathway of EPA metabolism leads to the formation of prostaglandins and prostacyclin of series 3, as well as thromboxane A3. The lipoxygenase pathway leads to the formation of leukotrienes of series 5 [41].
The functional properties of eicosanoids synthesized from omega-6 and omega-3 PUFAs are diametrically opposite. Prostaglandins and prostacyclin of series 3, derived from omega-3 PUFAs, promote platelet disaggregation and exert vasodilatory effects. In contrast, prostaglandins and prostacyclin of series 2, synthesized from omega-6 PUFAs, inhibit platelet disaggregation and induce vasoconstriction. It should also be noted that prostaglandins are formed in virtually all organs and tissues. Thromboxane A3, synthesized from omega-3 PUFAs, exhibits anti-aggregatory effects. Conversely, thromboxane A2, synthesized from omega-6 PUFAs, activates platelet aggregation. Similar differences are observed in the synthesis of leukotrienes. Leukotrienes of series 5, synthesized from omega-3 PUFAs, exert pronounced anti-inflammatory effects. Meanwhile, leukotrienes of series 4, synthesized from omega-6 PUFAs, potentiate inflammation [42]. On average, the omega-3/omega-6 ratio in the human body is 1:4 [43].
However, it should be noted that in certain tissues, the omega-3/omega-6 ratio shifts towards an increase in omega-3 polyunsaturated fatty acids (PUFAs). For instance, in the cells of the brain and hepatocytes, this ratio is 1:2 [44-47].
Taking the above into consideration, it becomes clear that the clinical effects of acetylsalicylic acid and other NSAIDs directly depend on the initial ratio of PUFA quantities present in cell membrane phospholipids. This fact is the main reason for the paradoxical clinical effects observed with the use of NSAIDs and must be taken into account by clinicians. Furthermore, for the effective and safe use of COX inhibitors, it is essential to have knowledge of the comprehensive mechanism of action of NSAIDs, rather than relying solely on pharmacological instructions, recommendations, and protocols. The selection and monitoring of anticoagulant and antiplatelet therapies should be based on comprehensive data from laboratory and instrumental research methods, enabling the efficient and safe correction of the hemostatic system.
One Of the Common Methods Used In Clinical Practice To Assess The Hemostatic System Is Cholangiogram.
Clinicians often attempt to evaluate the state of hemostasis based solely on cholangiogram parameters and use pharmacological agents to correct it. However, this laboratory method of monitoring the blood coagulation system primarily reflects the potential capabilities of plasma factors to support hemostasis and often does not reflect their implementation in action.
Therefore, an analysis of the hemostatic system based solely on cholangiogram data cannot fully characterize the true state of the blood coagulation system.
An effective method that allows for a rapid assessment of the implementation of main components of the blood coagulation system is thromboelastographic (TEG) [48]. Unlike the cholangiogram, TEG is an instrumental laboratory diagnostic method that reflects the process of thrombus formation and fibrinolysis in real-time. The interpretation of TEG data allows for an objective evaluation of the state of the plasma and platelet components of hemostasis, as well as the fibrinolysis system. The confirmation of the above is supported by common clinical examples of discrepancies between cholangiogram data and thromboelastographic (TEG) parameters, as illustrated in Figures 5-8.
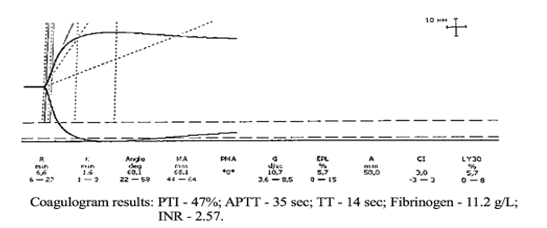
Figure 5. TEG parameters against the background of coagulogram data of patient K.
The coagulogram data presented in Figure. 5 indicate pronounced hypocoagulation (high INR values and low PTI) in the presence of hyperfibrinogenemia. In contrast, the thromboelastogram (TEG) objectively registers a high risk of hypercoagulation due to hyperfibrinogenemia.
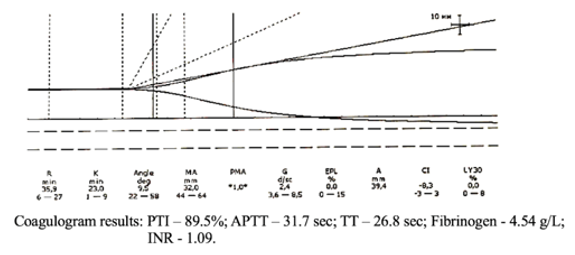
Figure. 6. TEG parameters against the background of cholangiogram data of patient R.
In Figure. 6, the coagulogram data only indicate a risk of hypo coagulation. At the same time, the thromboelastogram (TEG) shows pronounced hypo coagulation that requires immediate correction.
The next clinical case scenario is presented in Figure 7.
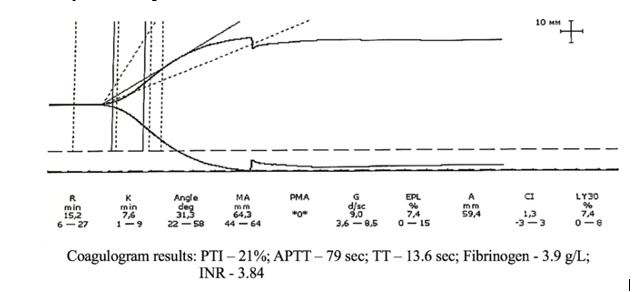
Figure. 7. TEG parameters against the background of coagulogram data of patient M.
In Figure 7, the coagulogram parameters indicate pronounced signs of hypocoagulation that require urgent pharmacological correction. Conversely, the thromboelastogram (TEG) data demonstrate increased platelet aggregation. However, the hemostatic system remains balanced.

Figure 8. TEG parameters against the background of cholangiogram data of patient S.
Figure 8 demonstrates that the cholangiogram parameters are mostly within the normal range. However, the TEG clearly registers a decrease in the coagulation index due to platelet aggregation inhibition. Thus, the presented clinical examples vividly demonstrate that based solely on cholangiogram parameters, a physician cannot adequately assess and perform effective hemostasis correction. Ignoring this fact can lead to the rapid development of life-threatening complications for the patient. Evaluation of the clotting system and monitoring of antiplatelet and anticoagulant therapies should be based solely on a comprehensive analysis. Analysis of the hemostatic system, along with cholangiogram data, must necessarily include TEG parameters, which are crucial. Additionally, other clinical and laboratory indicators, as well as immunological and biochemical research data, should be taken into account. These indicators characterize the state of the body's internal environment and directly or indirectly influence hemostasis. For example, this includes liver enzyme activity, platelet count, homocysteine level, immunoglobulins, acute-phase proteins, blood oxygen levels, and so on.
About D-Dimer Levels.
Recently, especially during the COVID-19 period, there has been widespread use of D-dimer level analysis among clinicians. Based on D-dimer levels, clinicians attempt to assess the effectiveness of anticoagulant therapy. However, it is important to clarify certain key aspects of this study and provide clarity on the interpretation of the obtained data. Firstly, it should be noted that D-dimers are products of the breakdown of fully formed blood clots, which are formed as a result of fibrinolysis [49]. Moreover, the key word here is "breakdown." Elevated levels of D-dimers appear only when a large number of fully formed blood clots, resulting from fibrinolysis activation, start to rapidly break down rather than form. This means that during acute thrombosis (such as in pulmonary embolism, myocardial infarction, stroke, etc.), for a certain period of time ranging from several tens of minutes to hours, D-dimer levels may remain within the normal range, and the anticoagulant therapy conducted according to protocol may be considered adequate. As the D-dimer levels increase, often in the absence of fibrinolysis activity data, clinicians mistakenly believe that it is necessary to increase the dosage of anticoagulants. In doing so, they overlook the fact that D-dimers inhibit the polymerization process of fibrin monomer complexes, and their rapid increase can lead to a transition from hypercoagulation to hypo coagulation and the development of bleeding [50]. Blindly following
protocols and instructions, doctors fail to consider the fact that many pharmacological agents can also influence fibrinolysis activity to varying degrees.
It is also important to emphasize that in cases of thrombosis, the platelet count does not correlate with their functional activity. Therefore, thrombocytosis or thrombocytopenia are not absolute indications or contraindications for the use of pharmacological hemostatic agents (not to be confused with platelet transfusion!).
Findings.
Proper correction of the hemostatic system can only be carried out by a highly qualified specialist - a clinical transfusiologist, who possesses a comprehensive understanding of the functioning of the coagulation and anticoagulation systems, platelet and fibrinolysis systems, knows the points of application and mechanisms of action of the pharmacological agents and blood components used, and takes into account the factors of the internal and external environment that influence hemostasis.
Empirical administration of anticoagulant and antiplatelet therapies, based solely on instructions and clinical protocols without considering objective analysis of the state of the hemostatic components, is incorrect, ineffective, and most importantly, dangerous for the patient's life. Coagulation profile parameters cannot serve as independent markers for monitoring the hemostatic system. Evaluation of the hemostatic system should only be done based on a comprehensive analysis of coagulation profile data, complete blood count, thromboelastography (TEG), and data from all relevant systems involved.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
