AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Universidade Federal do Rio de Janeiro1, Rio de Janeiro, RJ
Citation: Mauro Alves. (2023), North Manchester General Hospital, Department of Urology, Manchester, United M8 5RB. Kingdom, J, Surgical Case Reports and Images 6(4); DOI:10.31579/2690-1897/153
Copyright: © 2023, Mauro Alves. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 05 May 2023 | Accepted: 21 May 2023 | Published: 02 June 2023
Keywords: condyloma acuminatum of penis; the buschke-lowenstein tumour; histopathology, koilocytosis; oral sex; genital sex; anal sex; hpv genotypes 6 and 11; hpv 16, 18, 30 - 32, 42 – 44; hpv 51 – 55; medical treatment, surgical treatment; recurrence
Condyloma Acuminatum which is also referred as genital warts is a terminology that is utilized for Contagious HPV related lesion with a clear predilection for the anogenital region of the body. Condyloma Acuminatum tends to be transmitted through skin-to-skin contact during the undertaking of oral, genital or anal sex. Condyloma Acuminatum is most frequently caused by HPV genotypes 6 and 11. Other genotypes that had been identified in Condyloma Acuminatum include HPV 16, 18, 30 - 32, 42 - 44 and 51 – 55. Condyloma acuminatum is a benign lesion. Malignant transformation of condyloma Acuminatum is very rare. The Buschke-Lowenstein tumour emanates from the confluence of multiple condyloma acuminata and it clinically tends to manifest presentation of warty, exophytic, ulcerated lesions that portend an aggressive biological behaviour, rapid growth, invasion, as well as destruction of adjacent structures. Gross examination of specimens of Condyloma Acuminatum tends to demonstrate: Papillary, fungating, wart-like, often multiple lesions and which tend to measure1 mm or larger. Microscopy pathology examination features of condyloma acuminatum include: Arborescent (tree-like, complex) "condylomatous" spiky papillae that contain prominent central fibrovascular cores, Surface koilocytosis (koilocytes that have hyperplastic epithelium with wrinkled hyperchromatic nuclei, perinuclear halos and frequent bi and multinucleation; sharply defined base without invasion; preservation of orderly maturation of epithelial cell; presence of T lymphocytes with (CD4+ finding; evidence of reactive atypia but no evidence of invasion; variable acanthosis and hyperkeratosis. A number of treatments options are available to treat condyloma acuminatum of the penis including: Medical treatment of Condyloma Acuminatum with utilization of: imiquimod cream, 20% podophyllin antimitotic solution, 0.5% podofilox solution, 5% 5-FU cream and trichloroacetic acid (TCA). Other forms of treatment of Condyloma Acuminatum: freezing, burning (electrocautery), CO2 laser, or surgical excision (if large). Pursuant to treatment of Condyloma Acuminatum, the Condyloma Acuminatum does tend to recur but it does not evolve recurrence into invasive cancer. Some of the differential diagnoses of condyloma acuminatum of the penis include: Pearly penile plaques, Verruciform tumours (verrucous, papillary, and warty carcinomas): Tuberculosis of the penis and Squamous cell carcinoma of penis could also be considered as differential diagnoses of condyloma acuminata especially confluents ones including “The Buschke-Lowenstein tumour”. Considering that condyloma acuminatum is very rare, clinicians need to have a high index of suspicion for this clinical entity which can also be encountered in children and not only in adults.
Condyloma Acuminatum is a terminology that is used for Contagious HPV related lesion with a clear predilection for the anogenital region of the body [1] [2]
Condyloma Acuminatum tends to be encountered in sexually active young men, among whom HPV infections tend to be at epidemic proportions. Majority of cases of condyloma acuminatum are sexually transmitted, as has been underlined by the higher incidence of condyloma among men whose partners have HPV-related cervical lesions. The incidence of condyloma was documented to be about 5% among adults who are aged between 20 years to 40 years. Nevertheless, condyloma acuminatum of the penis has been reported sporadically. If condyloma of the penis is encountered in a child, sexual abuse would need to be strongly considered as well as investigated. Condylomas manifest as either flat or cauliflower-like lesions which usually tend to be found upon the corona of the glans penis, fossa navicularis, or urethral meatus, but involvement of scrotal or perineal skin may also occur. Considering that condyloma acuminatum of the penis is not common and may simulate more common lesions of the penis, there is the possibility that many clinicians globally may not be familiar this uncommon clinical entity. The ensuing article on condyloma acuminatum of the penis has been divided into two parts: (A) Overview which has summated salient features of the General Aspects of Condyloma Acuminatum; and (B) Miscellaneous Narrations and Discussions from Some Case Reports, Case Series and Some Studies Related to Condyloma Acuminatum with a Focus on Condyloma Acuminatum of the Penis.
Internet data bases were searched including: Google; Google Scholar; Yahoo; and PUBMED. The search words that were used included: Condyloma Acuminatum of Penis; Penile condyloma acuminatum; Condyloma Acuminatum of urethra. Sixty-seven (67) references were identified which were used to write the review and update of the literature on condyloma acuminatum of the penis which has been divided into two parts: (A) Overview which has summated salient features of the General Aspects of Condyloma Acuminatum; and (B) Miscellaneous Narrations and Discussions from Some Case Reports, Case Series and Some Studies Related to Condyloma Acuminatum of the Penis.
[A] Overview
Definition / general statements
It has been stated that Condyloma Acuminatum is a terminology that is utilized for Contagious HPV related lesion with a clear predilection for the anogenital region of the body [1] [2]
Terminology
It has been pointed out that an alternative terminology which tends to be used for Condyloma Acuminatum is genital wart. [1]
Epidemiology
It has been explained that Condyloma Acuminatum tends to be transmitted through skin-to-skin contact during the undertaking of oral, genital or anal sex.[1]
It has been iterated that Condyloma Acuminatum most commonly affects young males in teenage years and 20s (third decade of life). [1]
It has been pointed out that Human Papilloma Virus (HPV) represents the most common sexually transmitted disease within the United States of America (U.S A). but many HPV infections do not lead to the development of condyloma acuminatum. [1]
Sites
It has been pointed out that the most common sites for the development of Condyloma Acuminatum in decreasing frequency are the glans penis, foreskin, meatus and shaft the shaft of the penis. [1]
Furthermore, it has been documented that Condyloma Acuminatum has often tended to afflict areas near the coronal sulcus and inner surface of the foreskin. [1]
Aetiology
It has been iterated that Condyloma Acuminatum is most frequently caused by HPV genotypes 6 and 11 [1]
It has been iterated that other genotypes that had been identified in Condyloma Acuminatum include HPV 16, 18, 30 - 32, 42 - 44 and 51 – 55. [1]
It has been pointed out that Condyloma Acuminatum is related to verruca vulgaris which is a common wart [1]
Clinical features of Condyloma Acuminatum
Summations related to the salient features of Condyloma Acuminatum include: [1]
Condyloma Acuminatum is a benign lesion. [1]
Condyloma Acuminatum lesions tend to be small lesions that are detected with utilization of topical acetic acid
It has been pointed out that malignant transformation of condyloma Acuminatum is very rare. [1]
Treatment
Summations related to the treatment and outcome following treatment of Condyloma Acuminatum had been outlined as follows: [1]
Medical treatment of Condyloma Acuminatum includes utilization of: imiquimod cream, 20% podophyllin antimitotic solution, 0.5% podofilox solution, 5% 5-FU cream and trichloroacetic acid (TCA). [1]
Other forms of treatment of Condyloma Acuminatum that had been pointed out include: freezing, burning (electrocautery), CO2 laser [1] [3] or surgical excision (if large)
It has been pointed out that following treatment of Condyloma Acuminatum, the Condyloma Acuminatum does tend to recur but it does not evolve recurrence into invasive cancer. [1]
Macroscopy Gross Features
It has been pointed out that macroscopy gross examination of specimens of Condyloma Acuminatum tends to demonstrate the ensuing features: [1]
Papillary, fungating, wart-like, often multiple lesions and which tend to measure1 mm or larger
It has been advised that lesions that depict the aforementioned gross features upon examination should be sectioned and the lesions should be examined thoroughly to exclude verrucous carcinoma based upon their pathology examination features.
Microscopic (histology) description
The pathology examination features of condyloma acuminatum have been summated as follows: [1]
Pathology microscopy examination of specimens of condyloma acuminatum tends to demonstrate: Arborescent (tree-like, complex) "condylomatous" spiky papillae that contain prominent central fibrovascular cores [1]
Pathology examination of specimens of Condyloma Acuminatum also tends to reveal Surface koilocytosis (koilocytes have hyperplastic epithelium with wrinkled hyperchromatic nuclei, perinuclear halos and frequent bi and multinucleation) [1]
Pathology examination of specimens of Condyloma Acuminatum also tends to reveal sharply defined base without invasion. [1]
Pathology examination of specimens of Condyloma Acuminatum also tends to reveal preservation of orderly maturation of epithelial cells. [1]
Pathology examination of specimens of Condyloma Acuminatum also tends to reveal T lymphocytes (CD4+) present. [1]
The lesion on microscopy pathology examination may be found to demonstrate evidence of reactive atypia but no evidence of invasion. [1]
Pathology examination of specimens of Condyloma Acuminatum also tends to reveal variable acanthosis and hyperkeratosis. [1]
It has been pointed out that in condyloma acuminatum koilocytosis is not evident in some cases but the histological pattern tends to be otherwise characteristic of condyloma acuminatum. [1]
Cytology description
It has been pointed out that cytopathology examination detection of HPV infection in penile samples collected for liquid-based cytology tends to be low [1] [4]
Molecular / cytogenetics description
It has been pointed out that with regard to the molecular and cytogenetics features of condyloma acuminatum specimens, lesions with HPV 6 and 11 by in situ hybridization are usually found to have perinuclear halos and nuclear atypia. [1]
It has also been pointed out that lesions with HPV DNA by PCR only may contain only a focally thickened granular layer associated with epithelial crevices [1] [5]
Differential diagnosis
Some of the differential diagnosis of condyloma acuminatum that had been documented include: [1]
Pearly penile plaques: These lesions had been stated to be HPV negative, and in the lesions, hyperkeratosis may be present bot no koilocytosis tends to be seen upon microscopy examination and no significant inflammation tends to be seen. [1]
Verruciform tumours (verrucous, papillary, and warty carcinomas): invasion is stated to be evident upon pathology microscopy examination. [1]
It would be envisaged that some clinicians would consider the following to have features upon macroscopy examination that could provisionally be considered to constitute differential diagnoses of condyloma acuminatum:
Tuberculosis of the penis.
Squamous cell carcinoma of penis.
[B] Miscellaneous Narrations And Summations From Some Case Reports, Case Series And Studies Related To Condyloma Acuminatum.
Weis et al. [6] reported a 46-year-old man who had human immunodeficiency virus who had manifested with a condyloma that had formed over a period of 6 months and which had encased his penis, scrotum, and perineum. Visible condyloma growth began when the patient who was an immunocompromised patient started highly active antiretroviral therapy, and it grew rapidly as his viral load plummeted. The patient did undergo resection and reconstruction with skin grafting. Pathology examination findings of the surgical specimen revealed benign condyloma acuminatum. This rapid progression of condyloma growth was documented to represent a cutaneous manifestation of immune reconstitution inflammatory syndrome.
Iturralde Codina et al. [7] reported an uncommon case of giant penile condyloma. The patient was treated surgically by denudation and fulguration due to the extent of the penile lesion before the undertaking of treatment with topical podophyllin. The histopathological examination of the specimen was determinant in the diagnosis of giant condyloma of the penis and the postoperative results were excellent. Iturralde Codina et al. [7] concluded that they would recommend to commence treatment with topical podophyllin and that if the lesion does not improve, resection and fulguration of the condyloma should be undertaken as well as that the patient should be followed closely for recurrence.
Uchida et al. [8] reported two cases of giant condyloma of the penis which treated with penis-sparing methods. In the first case, the papillomatous tumour had disappeared with topical utilization of fluorouracil ointment. In the second case, the tumour was treated with topical use of fluorouracil or bleomycin hydrochloride, which was followed by the resection of tumour.
Dupin et al. [9] stated that genital warts are an epidermal manifestation attributed to the epidermotropic human papillomavirus (HPV) and that over 100 types of double-stranded HPV had been isolated and completely sequenced thus far by the time of publication of their article in 2004. Dupin et al. [9] also iterated that HPVs are grouped into low-risk (non-oncogenic) types such as type 6 and type 11, which cause benign anogenital warts (condyloma accuminata), and high-risk (oncogenic) types, such as types 16, 18, 31, and 45, which occasionally lead to cancer.
Bryan et al. [10] Cancer-associated human papillomavirus (HPV) types are detected in genital warts that had been removed from immunosuppressed individuals more commonly in comparison with those occurring in otherwise healthy individuals. They also stated that the prognosis of genital warts containing cancer-associated HPV types was not known. Because it had been assumed that genital warts are benign lesions, they are usually treated by destructive therapies without prior knowledge of histopathology report of the lesion. Bryan et al. [10] undertook a study which was aimed to determine whether genital warts from individuals with or without human immunodeficiency virus (HIV) contain high-risk HPV types or areas of dysplasia. The study design was reported to be a non-randomized analysis of genital warts which had been removed by excision biopsy from 15 HIV-infected patients and 15 HIV-negative patients. The tissue was analysed for HPV DNA by hybrid capture, and microscopy pathology sections of each biopsy were examined for areas of dysplasia. With regard to the results, Bryan et al. [10] reported that Genital warts from HIV-infected patients contained cancer-associated ("high risk") HPV types in 9 of 15 cases, including 1 that contained only a high-risk type. High-grade dysplastic abnormalities were found present in 2 of the 15 lesions from this group, both of which had contained high-risk HPV types. Four genital warts removed from HIV-negative patients were found to have contained high-risk HPV types; however, none contained dysplastic abnormalities. Bryan et al. [10] iterated that genital warts from HIV-infected patients often contain high-risk HPV types and that such lesions may exhibit dysplastic changes. They also pointed out the following:
The frequency of dysplastic changes in genital warts from HIV-infected patients was not known.
Biopsy of genital warts might be indicated preceding additional therapy in HIV-infected patients, and surgical removal should be considered as a preferred treatment option in these patients.
Voltz et al. [11] undertook a study to ascertain the prevalence of the Human Papillomavirus (HPV) in Human Immunodeficiency Virus (HIV) infected men, using clinical examination and molecular hybridization in situ. With regard to the patients and methods, Voltz et al. [11] reported that from May 1995 to May 1997, they had studied the prevalence, clinical and histological characteristics, the types and the evolution of the HPV lesions among 121 HIV-infected men. The HPV DNA was determined by molecular hybridization in situ, using biotinylated probes which recognized HPV types 6/11, 16/18 and 31/33/35 in 79 p. 100 (5/19) of the patients (17 biopsies). Voltz et al. [11] summarized the results as follows:
Sixteen per cent (19/121) of the patients were HPV infected: genital warts in 37 patients. 100 (7/19), anal warts in 37 patients. 100 (7/19), and ano-genital warts in 26 patients. 100 (5/19) of the patients.
In every case of anal condyloma, intracanalar lesions were found.
In 47 patients. 100 (9/19) of the cases, histological examination showed an intra-epithelial neoplasia.
The HPV types 6/11, 16/18 and 31/33/51 were positive in 53 patients. 100 (9/17), 35 patients. 100 (6/17) and 35 patients. 100 (6/17) biopsies respectively.
High-risk types of HPV had been noted in 71 patients. 100 (12/17) of the biopsies.
The evolution of the clinical lesions was: recovering in 47 patients. 100 (9/19) of the patients (after 3 months of treatment), recurrence in 16 patients. 100 (3/19) of the anal warts (after 1 to 3 months of treatment), stabilization in 16 patients. 100 (3/19) of the genital warts (after 6 months of treatment) and extension in 11 p. 100 (2/19) of the anogenital warts (after 3 months of treatment).
Voltz et al. [11] made the following conclusions:
The high prevalence of condyloma and dysplasia emphasizes the importance of the anogenital exam in HIV-positive patients
In the case of anal lesions, anuscopy and biopsy would be required.
They do insist on the need to closely follow these patients with HPV lesions in order to adapt the treatment.
Anal cytology and HPV-DNA detection by Hybrid Capture Assay, should be developed for the screening and prevention of the malignant transformation of HPV lesions in this population.
Kang et al. [12] reported a 72-year-old man who had a genital mass, which appeared to be composed of multiple papillomatous masses, who was referred for surgical resection. The lesion was first noticed 6 months earlier and had grown rapidly. CO2 ablative laser therapy was undertaken twice at a primary clinic, but the mass had recurred. With regard to intervention and outcomes, Kang et al. [12] reported that excisional biopsy of the mass had revealed the presence of coexistent EMPD and CA. Additional wide excision was undertaken, and postoperative biopsy of the specimen confirmed no residual tumour. Two years after surgery, no recurrence had occurred. With regard to lessons that should be learnt, Kang et al. [12] stated the following:
CA could co-occur with several types of skin malignancies, and a skin malignancy coexisting with CA is difficult to diagnose visually.
In view of this, even if a skin lesion in the genital region is considered to be CA, they recommend the undertaking of punch biopsy before treatment because it can benefit the prognosis.
Kang et al. [12] made the ensuing iterations:
It has been stated that extramammary Paget’s disease (EMPD) is a rare skin cancer which does arise by epidermotrophic spread from an in situ or invasive neoplasm arising in an adnexal gland within dermis. [13]
In view of this, the sites that are most commonly afflicted by EMPD are rich in apocrine glands, such as perineum, vulva, axilla, scrotum, and penis. [13], [14], [15]
The commonest manifesting symptom of EMPD is pruritis, and clinically it is usually visualized as a demarcated, thickened, eczematoid, or crusted lesion with an irregular border.[13]
It had been pointed out that the lesions had been noted to be occasionally hyper- or hypo-pigmented.[13]
In addition, EMPD has tended to be difficult to distinguish visually from other skin lesions such as eczema, contact dermatitis, or Bowen’s disease, [13] [16] and therefore, its diagnosis is quite often delayed.
Pathologically, neoplastic cells that depict glandular differentiation tend to be observed in the form of intraepithelial (usually intraepidermal) infiltrations, [13] and thus cytokeratin 7, which is expressed in sebaceous glands and the secretory coils of eccrine glands, is a specific immunohistochemical marker for EMPD.[17]
Condyloma acuminata (CA; anogenital warts) had usually been caused by human papillomavirus strains 6 or 11, though uncommonly by strains 16, 18, 31, 33, or 35. [18]
CA had usually tended to be asymptomatic, even though this depends upon the size of the lesion as well as the anatomical location; however, it could be pruritic or painful. [9], [18], [19], [20]
Clinically, CA has usually been encountered as a papillomatous eruption in genital mucosa and it is usually diagnosed by visual inspection.
Only on rare occasions its diagnosis is confirmed by biopsy.
At the time of publication of their article, available treatments for CA had focused upon wart removal rather than eradication of the underlying viral infection. [19]
CA is treated utilizing topical agents (podophyllotoxin, imiquimod cream, or sinecatechins), by destructive or surgical treatments (trichloroacetic acid, cryotherapy, CO2 laser ablation, or surgery), or by systemic interferon treatment. [9], [18], [19], [20]
Only 3 cases of coexistent CA and EMPD had been reported. [21], [22], [23]
They were reporting a rare case of coexistent EMPD and CA.
Kang et al. [12] reported a 72-year-old Asian male patient who had hypertension and who visited their urology department with multiple papillomatous masses of his penis and scrotum. The patient had reported that he first noticed the lesion 6 months preceding his presentation and that the lesion later had increased considerably in size. Initially, he visited a primary clinic where the masses were diagnosed as CA by visual inspection. CO2 ablative laser therapy was administered twice, but the mass had recurred. Accordingly, he was referred to their institute for excision and reconstruction. Physical inspection had demonstrated a hypopigmented eczematoid plaque lesion (that measured about 8 cm × 6 cm in size) and a verrucous papule above the lesion (Fig. 1). Excision of the lesion and defect coverage with a local flap was planned, and his surgery was undertaken under spinal anaesthesia. Nevertheless, postoperative biopsy results following pathology examination of the excised penile lesion revealed the presence of coexistent CA and EMPD (Fig. 2), the presence of residual tumour in all excised margins, and that the tumour was confined to the epidermis. Chest and abdominopelvic computed tomography were undertaken to exclude possible distant metastasis, but none was found. An oncologist who was consulted regarding the need for adjuvant therapy recommended that additional lymph node dissection and adjuvant therapy were not required and that treatment could be terminated after complete resection. Kang et al. [12] decided to excise remaining EMPD with a margin of 2 cm, and the excision was undertaken until examination of frozen biopsy showed that the surgical resection margins were negative for EMPD (Figure. 3A). In addition, defects in scrotum and abdomen were covered utilizing a scrotal dartos musculocutaneous flap, and the penile shaft was covered utilizing a full-thickness skin graft (Figure. 3B and C). No recurrence was identified 2 years after the undertaking of the surgery (Figure. 4A), and no wound complication was encountered. In addition, full-thickness skin graft reconstruction of the penile shaft had provided sufficient elasticity to preserve erection function (Figure. 4B).

Figure 1: Preoperative photograph. 8.0 × 6.0 cm lesion on penis and scrotum with hypopigmented plaque and multiple papillomatous masses.
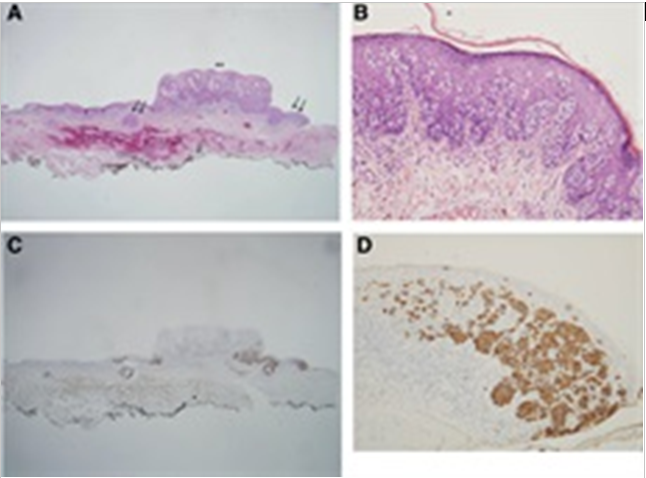
Figure 2: Histologic features. (A) A polypoid lesion of condyloma acuminatum was noted (asterisks), and the adjacent surface and follicular epithelium were thickened (arrows) (H&E, ×40). (B) At high magnification, large, atypical cells with abundant cytoplasm (Paget cells) were observed in thickened epithelium (H&E, ×200). (C, D) Immunohistochemical staining for allowed Paget cells, which presented as single cells or nests, to be easily identified at the periphery and base of the condyloma and adjacent thickened epithelium (CK7, ×40/CK7, ×200). CK7 = cytokeratin 7.
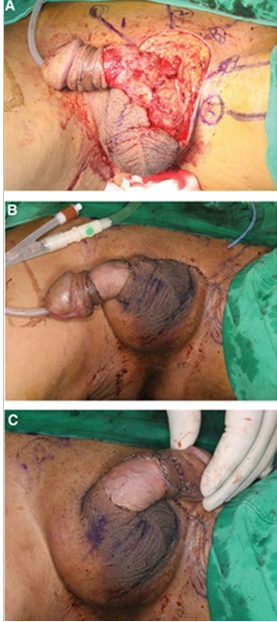
Figure 3: Intraoperative photographs. (A) Wide excision was performed with a margin of 2 cm. Excision was performed until the entire margin was negative, as determined by frozen biopsy. (B, C) Defects in the scrotum and abdomen were covered using a scrotal dartos musculocutaneous flap, and the penile shaft was covered using a full-thickness skin graft.

Figure 4: Postoperative photographs. (A) No recurrence occurred during 2 yr of postoperative follow-up, and no wound complication was encountered. (B) FTSG reconstruction of the penile shaft provided sufficient elasticity to preserve erection function. FTSG = full-thickness skin graft.
Reproduced from [12] under Creative Commons Agreement Licence which permits reproduction of figures and contents of the Journal articles.
Kang et al. [12] made the ensuing summating discussions:
Only 3 cases of coexistent condyloma acuminatum and EMPD had been previously reported by the time of the report of their case. [21], [23], [23]
EMPD is a slowly insidiously progressive intraepithelial skin cancer, and if it is left untreated and distant metastasis occurs the prognosis had tended to be poor.
EMPD is difficult to differentiate from other skin lesions visually and it should be diagnosed based upon the undertaking of biopsy. [13], [15]
Various treatment modalities had been suggested, including wide excision, laser ablation, radiotherapy, chemotherapy, and topical agent application, [1,3,13] but in non-invasive EMPD cases, wide local surgical excision with an adequate resection margin (2–3 cm) is the treatment of choice. [15], [24]
If distant metastasis is suspected, sentinel lymph node biopsy and lymph node dissection may be undertaken, [24] [13] and depending upon the situation, radiotherapy or chemotherapy may be utilized.
Non-invasive EMPD could be cured by wide local excision alone, but the prognosis of invasive EMPD is dismal.
According to a recent study, the 5-year mortality rate of EMPD exhibiting deep dermal invasion was noted to be 85.71%. [25] In view of this, early detection and treatment are critical.
CA could be treated with topical agents, laser ablation, cryotherapy, or surgery, even though most primary clinics initially adopt a method that is less invasive than surgery.
Biopsies are rarely undertaken. Nevertheless, though less invasive methods destroy do CA and the encompassing tissues, they may mask a coexistent skin malignancy. In view of this, in cases of coexistent CA and skin cancer (EMPD, Bowen’s disease, basal cell carcinoma, or squamous cell carcinoma), a diagnosis of skin cancer is likely to be delayed.
Many reports of Bowen’s disease, basal cell carcinoma, or squamous cell carcinoma accompanying CA had been issued. [14], [22], [26]
The Centers for Disease Control and Prevention guidelines for anogenital warts had recommend that biopsy should be performed when a lesion is atypical (e.g., pigmented, indurated, affixed to underlying tissue, bleeding, or ulcerated) [18]
When skin cancer is missed, the diagnosis had tended to be inevitably made in a more advanced state.
In addition, visual diagnosis of a skin malignancy coexisting with CA without a biopsy is difficult to make, and thus, they would recommend the undertaking of a biopsy before treating condyloma non-surgically.
In previous case reports, authors had discussed the possibility that CA and EMPD may interact synergistically during disease progression. [21], [22], [23]
In their case, a pathology examination had shown CA and EMPD lesions were clearly demarcated, which had suggested it was unlikely that CA influenced the occurrence of EMPD, but as EMPD weakens nearby cell immunity, human papillomavirus infection may have initiated CA. [21], [27]
Kang et al. [12] made the ensuing conclusions:
CA could co-occur with several types of skin malignancies, but it is difficult to diagnose a skin malignancy coexisting with CA visually.
In view of this, even if a skin lesion in the genital region is considered to be CA, they would recommend the undertaking of punch biopsy before treatment because it could substantially benefit the prognosis.
Chuang et al. [28] stated the following:
The understanding of condylomata acuminata (genital warts) had been enhanced by the recent development of diagnostic methods.
Forty-two types of human papillomavirus had been identified up to 1985, and at least sixteen types were noted to be involved in genital warts.
The incidence of genital warts is about 0.1% in the general population and more than 0.5% in young persons.
The incidence is known to be increasing rapidly and exceeding the incidence of genital herpes.
Females are more prone to be affected.
The epidemiology evidence supporting the relationship between genital warts and genital cancer has been overwhelming.
The evidence had also spoken for a strong correlation between genital warts and verrucous carcinoma of the genitalia, bowenoid papulosis, and laryngeal papilloma.
The person having genital warts might also have other cutaneous warts. This observation is compatible with the finding that types of human papillornavirus involved in other cutaneous warts were found in genital warts.
In view of the newer and easier ways of diagnosing non-conspicuous condyloma acuminatum and the potential for the malignant transformation of condyloma acuminatum, it as been strongly recommended that patients should be followed up periodically for early detection of neoplasia.
Atabay et al. [29] stated the following:
The diagnosis of condyloma acuminatum generally relies upon the presence of characteristic clinical features.
Nevertheless, atypical cases of condyloma acuminatum could cause diagnostic problems.
With the development of the molecular biological techniques, the condyloma acuminatum disease can be readily diagnosed.
Atabay et al. [29 reported a case of atypical condyloma acuminatum in a 25-year-old male who had manifested with mid-penile hypospadias and a mass which had extended from his scrotum to his corona through his chordee deformity. The clinical diagnosis was condyloma acuminatum. A tissue specimen obtained from the mass was obtained for histopathological examination and in-situ hybridization assay for human papilloma virus. Histopathological examination of the specimen revealed papilloma. The immunohistochemical staining studies of the mass was negative for human papilloma virus. Nevertheless, in-situ hybridization for human papilloma virus was found to be strongly positive. Atabay et al. [29] stated and the following:
Condyloma acuminatum should be suspected in hypospadias patients who have atypical papillomatous lesions on their chordee deformity.
In-situ hybridization is extremely useful for the establishment of the diagnosis.
In view of the fact that condyloma acuminatum is the cause of viral contamination and malignant transformation, it is worth considering histopathological examination and molecular biological techniques in order to protect both the patient and the sexual partner.
Juan et al. [30] stated that Giant condyloma acuminatum (GCA) is a rare, sexually transmitted disease with a high rate of local recurrence and malignant transformation. Nevertheless, the optimal treatment for patients in whom GCA coexists with penile cancer had not been well defined. Juan et al. [30] reported a case that was treated successfully with preservation of the penis. Wide tumour excision was undertaken and the patient received adjuvant intra-arterial chemotherapy with methotrexate. Juan et al. [30] evaluated the efficacy and functional outcome of penile preservation management for GCA with penile cancer transformation. In their reported case, no recurrence of penile tumour or of condyloma was found during follow-up for more than 12 months after treatment. The patient was very satisfied with the cosmetic and functional results following preservation of his penis.
Pineda-Murillo, et al. [31] stated the following:
The Buschke–Löwenstein tumour is an epithelial tumour that was initially described in 1925.
It tends to manifest within the fifth decade of life with a male-to-female ratio of 2.7:1.
Data had shown that approximately 3 million to 4 million cases of genital warts in men occur each year with a peak rate of 500 per 100,000 in the 25–29-year-old age group. [32]
There is an etiological relationship with the human papillomavirus (HPV).
More than 30 genotypes of HPV could infect the genital epithelium.
Genital warts that are due to HPV are mainly associated with genotypes 6 and 11 (low risk), while anogenital squamous cell carcinoma is associated with genotypes 16, 18, 31 and 33 (high risk).
Multiple investigations had been undertaken to differentiate verrucous carcinoma (VC) from giant condyloma of Buschke–Löwenstein (GCBL) and its relation to HPV2. [33]
Risk factors do include lack of personal hygiene, promiscuity, smoking, chronic irritation, presence of foreskin and immunodeficiency (congenital and acquired). [30]
The tumour comes from the confluence of multiple condyloma acuminata and is clinically manifested by warty, exophytic, ulcerated lesions, with aggressive behaviour, rapid growth, invasion and destruction of adjacent structures.
In men, it is usually located within the penis (81–94%), anorectal region (10–17%) and urethra (5%), but it could be found in the scrotum and urinary bladder.[34]
Within the penis, lesions typically occur around the coronal sulcus, frenulum and glans.
Despite benign histology, the malignant transformation of Buschke–Löwenstein tumour had been reported in 30% to56% of cases. [35] [36] [37]
Pineda-Murillo, et al. [31] reported a 57-year-old man who had type II diabetes mellitus, high blood pressure and a history of high-risk sexual behaviour with multiple partners, who was evaluated in the urology department for multiple penile lesions of verrucous appearance and fetid odour of 10 months of evolution, which had prevented the foreskin retraction. His clinical examination demonstrated several confluent penile lesions of exophytic morphology including the prepuce, glans and coronal sulcus (Figure. 5). The results of his serology tests were negative for various sexually transmitted infections, including human immunodeficiency virus (HIV) infection. Along with his clinical examination, he had a computed tomography CT) scan of his abdomen and pelvis which demonstrated the location and extension of the lesion as well as the involvement of inguinal lymph nodes, which were not affected. Biopsy of the lesion was undertaken and pathology examination of the specimen revealed a giant condyloma acuminatum that was associated with HPV. Conservative treatment with imiquimod cream (5%) was administered 5 days a week for a period of 1 month without any effective response, for which a partial penectomy was undertaken (Figures. 6, and 7). Management of the neourethra was crucial, being dissected from the corpus spongiosum distally for a distance of approximately 1 cm and transected. It was spatulated on its dorsal surface in order to facilitate reconstruction and prevent the development of stenosis. The spatulated urethra was approximated to the penile skin to create an oblique meatus with its open side at the 12 o’clock position. The length of the shaft of penis that shaft remained after the surgical procedure was about 3 cm, which was considered to be an acceptable length to maximize functional outcomes. At his follow-up assessment, it was noted that the patient had preserved the ability to void in the standing position with effective capacity to direct the urinary stream. His sexual function was maintained due to a penis length that was greater than 2 cm, which is considered the minimum length to allow intercourse. The patient had remained with satisfactory evolution in close surveillance due to the high risk of recurrence, with consultations within the outpatient clinic every 3 months during the first year in which physical examination of the penis, urethral meatus and inguinal region is undertaken in search of new lesions, stenosis and adenopathies.
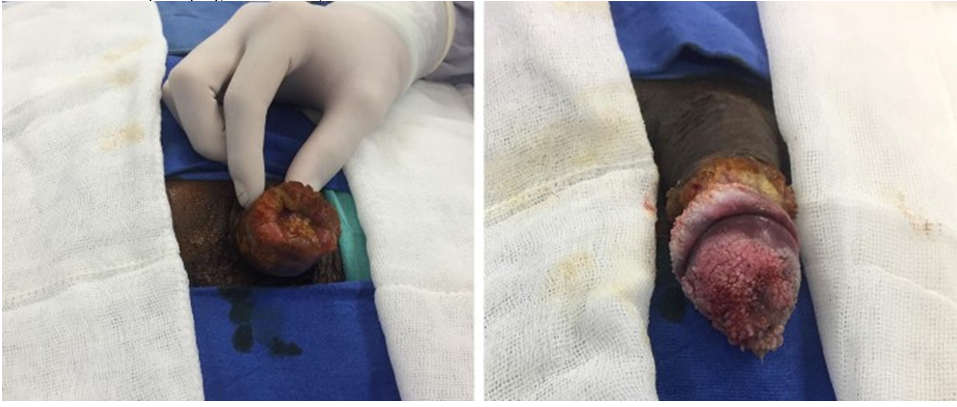
Figure. 5
Penile lesion of verrucous morphology including the prepuce, glans and coronal sulcus; Reproduced Under Copyright: Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
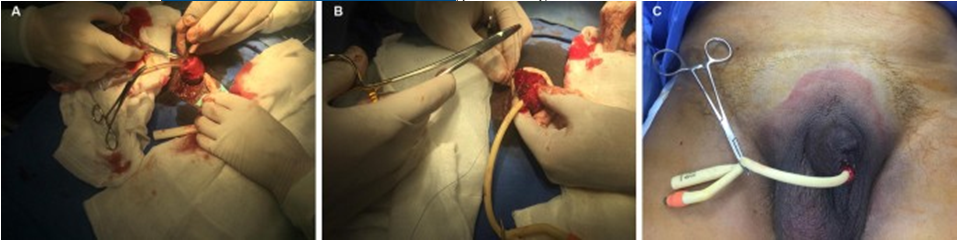
Figure. 6
Partial penectomy. a Urethral repair. b Closure of cavernous bodies. c Remaining penile tissue. Reproduced under Copyright: Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
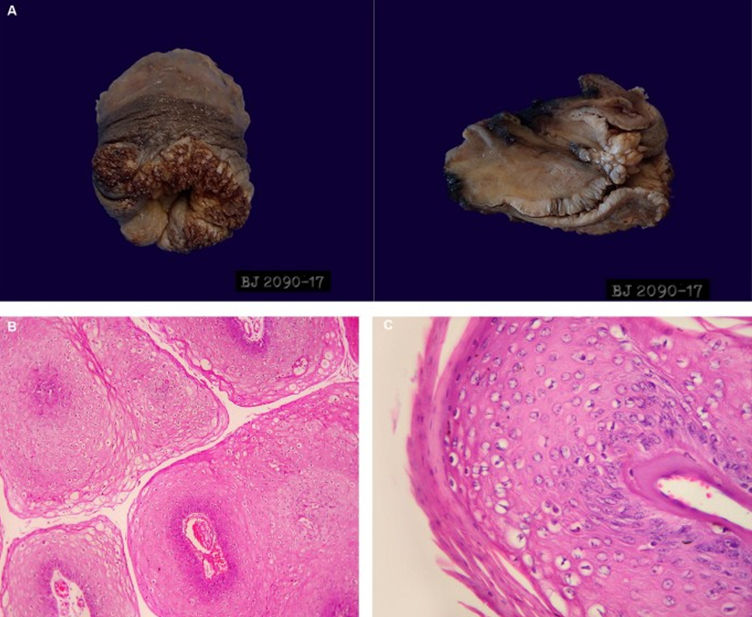
Figure. 7
a Macroscopic product of partial phallectomy. b Papillary projections coated by stratified squamous epithelium with acanthosis. c Cytopathic changes associated with human papillomavirus (HPV). Reproduced under copyright: Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Pineda-Murillo, et al. [31] made the ensuing summating discussions:
GCBL had been treated by several modalities of treatment, which can be classified into three types: topical therapy (e.g., podophyllin, fluorouracil or radiotherapy), tumour removal (e.g., cryotherapy, CO2 laser therapy or surgical excision) and immunotherapy (e.g., imiquimod).
Nevertheless, the variety of treatment regimens that currently being applied at the time of publication of their article did not allow the formulation of definitive therapeutic guidelines.
The application of imiquimod (5%), podophyllin (25–30%), trichloroacetic acid, 5-fluorouracil and bleomycin alone or combined with cisplatin or methotrexate has had variable results.
Treatment with interferons 2α and 2β combined with laser therapy (Nd:YAG) had been described, as well as cryosurgery with some cases of success.
Radical surgical excision with wide surgical margins has remained the first line of treatment, with a higher success rate (63–91%) and a lower rate of relapse. [38]
However, penile skin loss and repair of the urethra could be a challenge for urologists.
Surgical options include one-stage or two-stage procedures, utilizing either single or multiple tissue transfer [39] [40].
Preputial and various penile skin flaps, such as a longitudinal flap, the hockey stick flap, the penile island flap and the circumferential/circumpenile flap, had been utilized for penile urethral reconstruction as good options when needed. [41] [42].
A large representative biopsy specimen is important to judge the structure of the lesion in order to establish the diagnosis and to exclude VC. [43]
In microscopy examination, invasion of the subepithelial tissue is seen by expansion rather than by infiltration, leaving the basement membrane intact.
A well-stratified epithelium was shown with minimal cellular dysplasia or atypical cells, rare mitotic figures, acanthosis and hyperkeratosis and no evidence of neural or vascular invasion. [44]
The risk for the development of recurrence after excision is 60% to 66%, with an overall mortality of 20–30%. [45]
Close follow-up of these patients is crucial given the complexity and tumour recurrence.
Pineda-Murillo, et al. [31] made the following conclusions:
The Buschke–Löwenstein tumour is a rare disease which is typified by giant slow growing condyloma acuminatum that is locally aggressive and destructive.
Even though there had been reports of successful treatment with conservative modalities, the only consistently effective therapy is wide surgical excision of the tumour with clear margins with or without adjuvant chemotherapy.
Meliti et al. [46] stated the following:
Condyloma acuminatum is an anogenital lesion caused by the human papillomavirus infection.
It is a common, sexually transmitted disease.
It usually affects the external genitalia, while urethral and bladder involvement has tended to be uncommon.
Human papillomavirus types are classified into three categories depending on their oncogenic potential: low risk (type 6, 11, 42, 43, 44, 59, 66, 68, and 70), intermediate-risk (type 30, 31, 33, 34, 35, 39, 40, 49, 51, 52, 53, 57, 58, 63, and 64) and high risk (type 16, 18, 45, and 56). High-risk and intermediate-risk human papillomavirus DNA types, together with other co-factors still to be defined, account for over 90% of anogenital pre-malignant and malignant tumours.
They were reporting a unique case of condyloma acuminatum positive for human papillomavirus -6 involving the penile urethra, presents as the primary and only site of the disease in a diabetic type-2 patient. [46]
Meliti et al. [46] reported a 47-year-old male patient, who was a known case of diabetes mellitus and hypertension, well-controlled on medications. He was known to have bilateral renal stones for which he underwent percutaneous nephrolithotomy (PCNL) and bilateral ureterorenoscopy (URS) with laser lithotripsy. The patient manifested to their hospital with visible haematuria, he underwent cystoscopy examination which demonstrated a papillary-like lesion that was suspicious for malignancy within his mid penile urethra extending distally. However, his urethral meatus, prostatic urethra, and urinary bladder neck were normal endoscopically. Apart from bilateral kidney stones, the patient did not have any previous history of genitourinary pathology. Clinical examination of his external genitalia was unremarkable for gross abnormality. The urethral lesion was removed through urethrocystoscopy biopsy and submitted for histopathologic examination. Gross examination of the specimen showed a minute papillary-like tan tissue fragment. Microscopic examination of the specimen showed a fragment of papillary proliferation that was composed of hyperplastic non-keratinizing stratified squamous epithelium. In areas HPV-related changes were evident, including koilocytotic atypia (nuclear wrinkling with perinuclear halos), and binucleation (Figure 8(a) and (b). Nevertheless, no convincing histopathological evidence of papillary urothelial carcinoma was found. P16 immunohistochemistry staining was positive (Figure 8(c). In-situ hybridization (ISH) was positive for HPV-6 (Figure 8(d) and negative for HPV-16. Altogether, the histology features and molecular studies were adjudged to be diagnostic of condyloma acuminate of the penile urethra. The postoperative stay of the patient was reported to be uneventful with a short hospital stay. The patient had been put on follow-up regularly at the outpatient urology clinic. He was healthy with excellent functional performance status at 5 months.
Meliti et al. [46] made the ensuing summating discussions:
Condyloma acuminatum does uncommonly affect the male genital system, particularly the urethra.
The involvement of the male urethra usually occurs in an association with external genitalia condylomata.
A literature review had revealed few reported cases of isolated male urethra condyloma acuminata.
Olsen and colleagues had presented one example of condyloma acuminatum of the prostatic urethra without associated lesions on the external genitalia, but these condylomas were extensively involving the urethral meatus. [47]
Fralick and colleagues studied 114 biopsy-proven HPV infection of the external genitalia, of which 14 were intraurethral lesions. Only 8 patients had presented with a single urethral lesion, and the remaining 6 with multiple lesions; all were confined to anterior urethra. [48]
Their reported case represented an isolated penile urethral papillary growth without previous or concurrent evidence of external genitalia involvement. The initial clinical impression had raised the suspicion of a malignant urothelial neoplasm, particularly papillary urothelial carcinoma. Nevertheless, the histopathology examination revealed classic features of condyloma acuminatum. Confirmatory ancillary studies were positive P16 and HPV-ISH, which further supported the histology impression.
Few studies had suggested that chronic diseases with long-standing immunosuppression such as diabetes mellitus could be the initiative causative factor for urinary bladder malignancy.
Pathophysiology of long-standing insulin resistance, along with the metabolism of body fat, is more likely to generate an environment of cellular destruction. Ultimately leading to random genetic mutations and cell proliferation that can contribute to metaplasia and dysplasia-carcinoma sequence. [49]
The morphological differential diagnosis of their reported case includes papillary urothelial carcinoma, squamous cell carcinoma (SCC), and verrucous carcinoma. High-grade papillary urothelial carcinoma predominantly exhibits significant disordered proliferation with loss of polarity, high N/C ratio, prominent nuclei, and atypical mitosis. SCC shows unequivocal malignant features either of keratinizing or non-keratinizing subtype with anaplastic cytonuclear changes. On the other hand; verrucous carcinoma could arise upon the external genitalia, exhibits an exophytic, non-infiltrative growth pattern with bushing borders.
The role of HPV testing might not be necessary for condyloma acuminate diagnosis as the cytomorphologic features are usually sufficient for determination. Nevertheless, it is essential not to misdiagnose condyloma acuminatum as a malignant lesion to avoid overtreatment.
Meliti et al. [46] made the following conclusions:
They had reported a unique case of isolated penile urethral condyloma acuminatum
. Condyloma acuminatum does involve not only the external genitalia but also on rare occasions it could involve the prostatic urethra, urinary bladder, and ureter.
Urologists and practicing pathologists should be aware of this uncommon event as a diagnostic pitfall and should always consider condyloma acuminatum in the differential diagnosis for malignant urothelial neoplasms to further enhance the clinical management plans safely.
Olsen et al. [47] stated that Condylomata in the urethra usually tend to occur as a complication ensuing genital warts upon the external genitals and they are most often situated within the distal part of the urethra. Olsen et al. [47] reported of a male patient who had recurring papillomatous transitional cell tumours, stage pTa and pT1, grade 2 and 3 in his urinary bladder and his right ureter, who had presented with extensive condylomatosis within his urethra from the meatus to the verumontanum, without simultaneous presence of condylomata at the external genitals. Olsen et al. [47] also reported that Condylomatous fragments were also found present in the TUR specimen from his urinary bladder, but may have been displaced from the urethra during cystoscopy. Using PCR technique and in situ hybridisation, HPV types 6/11 were detected in the condylomata, but no virus was present within his transitional cell tumours. The lesson that clinicians need to learn from this case summation is the fact that condyloma of the urethra which has been regarded as a benign lesion most of the time could be found associated with transitional cell carcinoma of the urinary bladder and the ureter.
Fralick et al. [48] stated that in order to develop guidelines as to which asymptomatic male patients who have genital human papillomavirus (HPV) infection need to undergo further evaluation of the urethra, they studied two screening methods: urethroscopy and voided urethral cytology. With regards to the methods of their study, Fralick et al. [48] reported that over a four-year period, 135 asymptomatic men had undergone complete screening for HPV infection, who were evaluated because of HPV-related genital disease in their female sex partners or visible genital lesions, or both. Fralick et al. [48] summarized the results as follows:
Out of the 135 patients, 21 patients that amounted to 16% of the patients had no clinical, subclinical, cytological, or urethroscopic evidence of disease, and 114 of the patients that amounted to 84% of the patients had biopsy-proven HPV infection.
Out of these 114 patients, only 14 patients that amounted to 12.3% of the patients had intraurethral condyloma.
All of these 14 patients had current or historical evidence of meatal or peri-meatal "sentinel" lesions. They constituted 29.8 percent of 47 such patients with sentinel lesions.
In 5 patients that amounted to 4% of the patients, the results of their voided urine cytology were positive for condyloma cells, but only 1 of these had visible intraurethral disease.
Out of the 14 patients who had urethral disease, only 1 patient that amounted to 7% of the 14 patients had positive results of urine cytology.
Fralick et al. [48] concluded that these observations had indicated that any asymptomatic male patient undergoing screening for condyloma acuminatum who has a history of or demonstrable subclinical or grossly visible peri-meatal or meatal HPV infection should undergo the undertaking of urethroscopy as well as that voided urine cytology is not a reliable or cost-effective test for the detection of visible intraurethral disease.
Timm et al. [50] made the following summatory introductory iterations:
Isolated urethral condylomata acuminata (CA) is an unusual subgroup of genital warts which had been encountered in 0.5–5% of cases. [51]
It has been stated that HPV is sexually transmitted and the low-risk groups, DNA types 6 and 11, most commonly cause genital, perineal and anal lesions, which lend themselves to topical treatment. [52]
Urethral lesions do tend to present a challenge in application particularly if the proximal urethra has been involved.
First described by Dretler & Klein in 1975, [53] 198.administration of 5-fluourouracil (5FU) to the urethra had been utilized for the treatment of urethral CA with promising outcomes, even though exact administration details had been stated to be vague. [54]
Surgical treatment of intraurethral warts by laser had been successful, even though it carries with it the risk of fibrosis and in the younger age population they believed the risk of stricture formation is too high. [55]
They had described their technique for distribution of topical 5FU treatment to the entire urethra for the treatment of extensive pan-urethral CA and its outcomes in a patient where maximum flow rate (Qmax), post void residual (PVR) and cystoscopy evaluation were used as measures of response.
Timm et al. [50] reported a 28-year-old immunocompetent male who had manifested with increasing difficulty voiding over 6 months upon a background of previous cystoscopy investigation which had denoted no cause for obstruction. He was noted to be sexually active without concurrent sexually transmitted infection and no history or examination findings of genital warts. He underwent repeat cystoscopy following result of a Qmax of 7ml/s and PVR of 311ml upon his urine flow study. He underwent cystoscopy which demonstrated circumferential, pan-urethral polyps from the navicular fossa to his urinary bladder neck, (Figure. 8). The lesions were biopsied and pathology examination of the specimens demonstrated acanthopapillomatosis, surface hyperkeratosis and developed koilocytes, which pathologists had agreed was consistent with condylomatous histology (Figure. 9). Immunohistochemical staining studies of the specimen with p16 was found to be positive which is highly suggestive of human papilloma virus (HPV) infection.
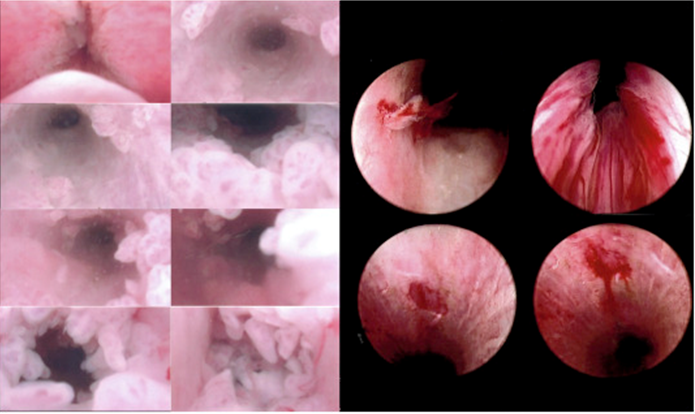
Figure 8: Cystoscopy findings pre-treatment and post treatment with urethral 5FU and focal surgical treatment. Reproduced from: [50] under Copyright. © 2020 The Authors. Published by Elsevier Inc.
Elsevier has partnered with Copyright Clearance Center's RightsLink service to offer a variety of options for reusing this content. Note: This article is available under the Creative Commons CC-BY-NC-ND license and permits non-commercial use of the work as published, without adaptation or alteration provided the work is fully attributed. For commercial reuse, permission must be requested below.
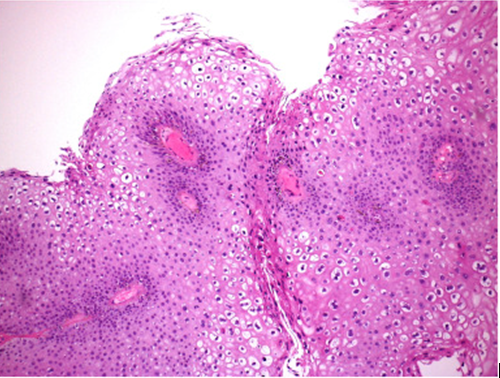
Figure. 9: H&E 100x magnification, features suggestive of condylomata acuminata -papillomatosis, surface hyperkeratosis and koilocytic change. Reproduced from: [50] under Copyright. © 2020 The Authors. Published by Elsevier Inc.Welcome to RightsLink
Elsevier has partnered with Copyright Clearance Center's RightsLink service to offer a variety of options for reusing this content. Note: This article is available under the Creative Commons CC-BY-NC-ND license and permits non-commercial use of the work as published, without adaptation or alteration provided the work is fully attributed. For commercial reuse, permission must be requested below.
Timm et al. [50] made the ensuing summating discussions:
Condylomata acuminata are a frequent manifestation of the most common sexually transmitted disease, HPV.
It has been stated that CA is associated with low-risk HPV (strains 6 and 11) in up to 90% of cases. [55]
Whilst CA is associated with low-risk HPV, it does not exclude the possibility of malignancy and hence histopathology assessment is advised.
A treatment protocol had been developed in coordination with the Melbourne Sexual Health Centre. Weekly rather than daily instillation of 5FU was elected for treatment as more significant side effect profiles have been encountered with daily application. [51] [52] [54]
The previous report by Wein et al. which had utilized self-instillation described as a “squeeze” of 5FU via urethral applicator after every void caused significant meatal ulcers, erosions and burning following treatment. [51]
Their induction treatment of 10g of 5FU weekly for 8 weeks avoided complications and was associated with only mild irritative symptoms.
Combination therapy of surgical and topical treatment had demonstrated improved outcomes compared with single modality treatment alone in recurrent urethral CA. [55]
Extensive surgical treatment may lead to stricture formation and therefore we advocate for debulking medical treatment prior to surgical intervention in extensive pan-urethral disease.
Equipment that was required for their 5FU instillation method: 2% lignocaine gel 10ml, 5FU 10g, Sterile gloves, normal saline, penile clamp, dressing pack (gauze and plastic pots/forceps). NB – all surfaces must be non-metal to preserve function of 5FU.
The procedure: Tube of 5FU is weighed to ensure correct dosage (If > 10g tubes available, able to be split and stored for multiple applications - in consultation with pharmacy). Sterile drape is placed upon scales including a sterile pot from catheter tray and contents of tube of 5FU are squeezed into pot and weighed to ensure correct dosage. A 10 ml Lignocaine gel 2% is then added to pot with 5FU and mixed with plastic forceps. Utilizing lignocaine syringe, mixture is drawn up and applicator tip is replaced (Figure. 10). The glans penis is then cleansed with normal saline and Lignocaine syringe is inserted gently into the urethral meatus where the mixture is slowly instilled. The meatus is manually occluded while the remaining volume of mixture is re-collected and administration is completed. A penile clamp or patient compression at distal glans penis is applied for 30minutes. Following release, the glans is cleansed with normal saline soaked gauze and the patient returns home to void and shower in an effort to avoid irritant side effects.
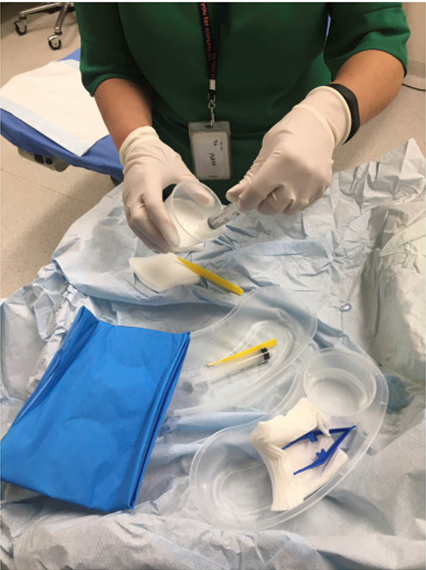
Figure 10: Equipment set up and administration preparation by our practise nurse. NB – Importance of all plastic utensils to avoid metal ion binding and making the 5FU less effective. Reproduced from: [50] under the Creative Commons Attribution License.
Pursuant to the 8-week induction course, an improvement in Qmax and PVR was demonstrated, most notably prior to the third instillation. Measures of Qmax and PVR following instillation at 1st, 2nd and 8th instillation were 7ml/s, 15ml/s, 19ml/s and 311ml, 230ml and 160ml respectively.
Subjective and objective improvement in flow was notable following a single instillation.
Increased sloughy debris was found following fifth treatment, even though testing for infection was negative.
Surveillance cystoscopy at 9 weeks had demonstrated significant volume reduction of the lesions; nevertheless, a small volume of residual CA at the neck of the urinary bladder and navicular fossa remained (Figure 8). These were removed by cold cup biopsy forceps without cautery or laser. The application of 5FU over 8 weeks was repeated a further time in an effort to reduce the risk of recurrence. At check cystoscopy there remained a single papilloma at the navicular fossa which was removed again by cold cup biopsy forceps.
Both Wallin et al. and Wein et al. had encountered similar difficulties with clearance of CA within the navicular fossa using 5FU. [51] [54]
Pursuant to the findings of recurrence of CA in the navicular fossa after 2 courses of 5FU, they had adopted the patient occluding the most distal portion of the glans in an effort to improve instillation time of 5FU and reduce risk of glans irritation.
Timm et al. [50] made the following conclusions:
In the absence of readily available premixed 5FU compounds for intraurethral application, sterile combination of 5_U with lignocaine 2% gel allows for a technically feasible and tolerable treatment regimen to minimise disease burden.
This decrease in disease volume diminishes the need for extensive surgical intervention which may lead to the development of urethral strictures in the younger populations.
Notably since the introduction of Quadrivalent HPV vaccination in 2007 there had been a declining incidence of genital warts, and, in time, urethral warts are likely to be relegated to the annals of historical curiosities.
Vageli et al. [56]] stated the following:
Penile warts in infants are rare and cases of condylomata acuminata at the urethral meatus are rarer.
Their reported case was the first report of a 2.5 years infant with a condyloma acuminatum at the urethral meatus of penis which was found positive for HPV 6, by PCR analysis.
The Infant’s mother presented warts on her hands, which had suggested a possible transmission of virus from mother to infant via extragenital contact, without excluding a vertical transmission.
It has been documented that Genital warts in children are not frequent while penile warts are even rarer [57] [58] [59] [60] [61]
The youngest documented case of this type of lesion was a 7-month-old circumcised Caucasian boy who had manifested with a rapidly progressing giant penile condyloma acuminatum which had been surgically removed followed by a fatal course of Neisseria meningitis. This case has served as a warning, concerning the course of condyloma acuminatum in infants, since the infant had died from meningococcemia five days after undergoing surgery. [61]
Condyloma acuminatum of the urethral meatus is very rare while there was only a single report of a 5-year-old child who had presented such a lesion without HPV infection history. [61]
They were reporting a HPV infected penile condyloma acuminatum at the urethral meatus, of a 2.5 year old infant, with a possible virus transmission from mother to infant.
Vageli et al. [56] reported a 2.5-years-old infant, who had manifested with a penile condyloma acuminatum at hic external urethral meatus, who attended the Paediatric Surgery Clinic of General Hospital of Larissa (Figure 11). His mother had mentioned that she had presented warts on her hands. The condyloma was surgically removed and two years after surgery the child was still healthy. The condyloma mass was subdivided to a part that was taken for the standard histopathology examination while the remaining tissue was immediately immersed into stabilization solution and frozen to -20°C. DNA was extracted from tissue using Puregene® Cell and Tissue extraction kit (Gentra Systems, Inc., USA) and an HPV detection molecular method was applied, as was previously was described. [62] [63] In brief a multiplex PCR (MPCR) was employed for the detection and discrimination of HPV types 6, 11, 16, 18 and 33 (specific E6 gene) utilizing a commercial kit (MPCR kit, Maxim Biotech) which included specific primers for each HPV type and corresponding positive control samples. The results of HPV-positive sample were reconfirmed by a PCR analysis utilizing specific primers for each HPV type only (Maxim Biotech). Vageli et al. [56] utilized non-template negative control samples, in each PCR reaction to exclude false positive results. The PCR products were electrophorized through 2% agarose gels, stained with 0.5 mg/ml ethidium bromide and visualized on a UV light transilluminator. The detection of specific sizes bands indicated the presence of target sequences, which corresponded to HPV type specific, in their specimen (Figure 2). Vageli et al. [56] undertook a melting curve analysis of PCR products to confirm HPV 6 genotype. Vageli et al. [56] undertook melting Curve analysis in Corbett RotorGene instrument as they had have described previously. [62] [64] utilizing SYBER Green (QuantiTect kit, Qiagen) and ramping 65-95°C (raising by 0.2°C each step). With regard to the results, Vageli et al. [56] stated that PCR analysis for HPV detection and typing had revealed that the DNA sample, derived from the penile condyloma acuminatum of the infant, was positively stained for HPV type 6 (Figure 12). Specifically, agarose gel electrophoresis of our specimen showed a 263-bp amplified PCR product, like HPV-6-positive control, corresponding to PCR amplified specific E6 gene of HPV type-6 (Figure 12). Confirmation of HPV6 genotype was undertaken performing a melting curve analysis of penile condyloma and HPV6 positive control PCR products. Both samples had shown melting peaks that corresponded to HPV6 genotype (Figure 13).

Figure 11: A condyloma acuminatu m at the urethral meatus of an infant’s penis.
Reproduced from: [56] Under Copyright: doi:10.4172/2157-7412.1000157 Copyright: © 2013 Vageli DP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
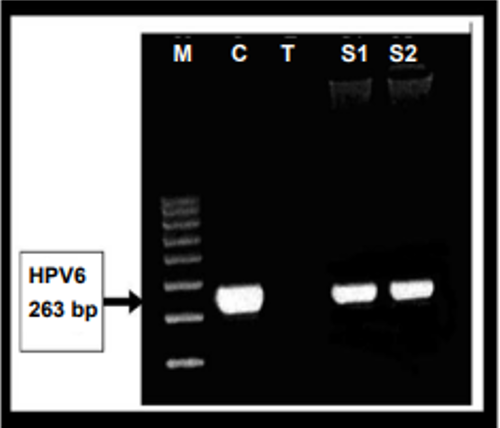
Figure 12: Detection of HPV 6 DNA, in a condyloma acumitatum derived from the urethral meatus penile of a 2.5 years infant, using HPV6-genotype specific primers. Lane M: DNA Molecular Weight Marker (100bp ladder); Lane C: HPV6 positive control; Lane T: Non-template negative control; Lanes S1 & S2: HPV6 positive amplified PCR products of DNA sample derived from the infant’s penile condyloma. Reproduced from: [56] Under Copyright: doi:10.4172/2157-7412.1000157 Copyright: © 2013 Vageli DP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
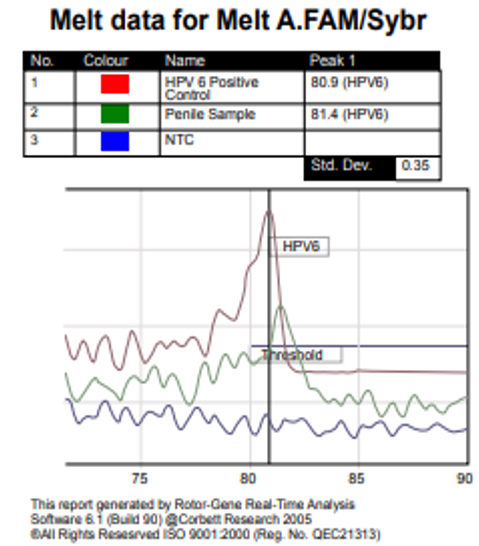
Figure 13: Melting curve analysis of a HPV 6 positive sample, derived from a 2.5 years infant’s penile condyloma acumitatum and a HPV6 positive control. Melting peaks at 81°C correspond to HPV6 genotype. Reproduced from: [56] Under Copyright: doi:10.4172/2157-7412.1000157 Copyright: © 2013 Vageli DP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Vageli et al. [56]] made the ensuing iterations:
They had reported a rare case of an infant who had a penile condyloma acuminatum at his urethral meatus that had been analysed by PCR method and which was found to be positive for HPV type 6.
In bibliography, it had been referred to a single case of a condyloma acuminatum of the urethral meatus in an infant, without a history of HPV infection. [61]
Genital HPV infection in children appeared to behave as a sexual transmitted via abuse [65] or vertically transmitted or extragenital contact transmitted. [66] [67]
None
© 2020 The Authors. Published by Elsevier Inc. Welcome to Rights Link
Elsevier has partnered with Copyright Clearance Center's Rights Link service to offer a variety of options for reusing this content.
Note: This article is available under the Creative Commons CC-BY-NC-ND license and permits non-commercial use of the work as published, without adaptation or alteration provided the work is fully attributed. For commercial reuse, permission must be requested below.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.
