AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Rehan Haider, Riggs Pharmaceuticals Karachi, Department of Pharmacy, University of Karachi-Pakistan.
Citation: Rehan Haider, (2023), Bone and Rheumatic Disorders in Diabetes, J Clinical Orthopaedics and Trauma Care, 5(3); DOI: 10.31579/2694-0248/066
Copyright: © 2023, Rehan Haider. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 13 July 2023 | Accepted: 21 July 2023 | Published: 01 August 2023
Keywords: rheumatic disorders, bone mineral density (BMD), fractures, osteoclasts; insulin signaling pathway; osteoclast function
Diabetes mellitus, a chronic metabolic ailment characterized by hyperglycemia, affects millions of people worldwide and poses a considerable burden on public health. While the number-one headache of diabetes frequently involves the cardiovascular, renal, and neurological systems, increasing evidence indicates a link between diabetes and bone and rheumatic issues. This abstract explores the complex interplay between diabetes and musculoskeletal conditions, to offer an overview of their pathophysiological mechanisms and medical implications.
Bone problems in diabetes are typically characterized by decreased bone mineral density (BMD) and an increased risk of fractures. The imbalance between bone formation and resorption, driven by hyperglycemia-precipitated oxidative stress, advanced glycation stop products (ages), and persistent inflammation, results in decreased osteoblasts interest and more desirable osteoclast features. Furthermore, alterations in the insulin signaling pathway and impaired osteocyte characteristics contribute to compromised bone formation in diabetes. These adjustments together contribute to an extended fracture chance and not on-time fracture recuperation in patients with diabetes.
Rheumatic issues in diabetes embody a wide variety of conditions including osteoarthritis, rheumatoid arthritis, and frozen shoulder syndrome. Persistent irritation due to dysregulated immune responses in diabetes can boost joint degeneration, worsen pain, and cause useful impairments. Furthermore, weight problems, regularly linked to type 2 diabetes, place additional mechanical pressure on the weight-bearing joints, exacerbating the progression of osteoarthritis. Rheumatoid arthritis, an autoimmune disease, may have complex interactions with diabetes because of its shared inflammatory pathways.
The clinical implications of these interactions are significant. First, healthcare providers should be vigilant in screening and diagnosing bone issues in patients with diabetes, particularly in the elderly population who are at a higher risk of fractures. Second, promoting lifestyle changes, including weight management, normal physical activity, and glycemic manipulation, can mitigate bone and joint-associated complications in diabetes. Additionally, progressive treatment plans focused on the common pathways of inflammation and oxidative stress may hold promise for the treatment of diabetes and its musculoskeletal comorbidities.
Bone and rheumatic disorders are increasingly identified as vital comorbidities in diabetes. The tricky pathophysiological mechanisms involved call for similar research to expand patient-centered therapeutic techniques that efficiently manage these musculoskeletal headaches and enhance the overall quality of life of individuals living with diabetes. A complete understanding of these relationships will enable healthcare specialists to enforce timely interventions and customize treatment plans to deal with the specific demanding situations posed by the aid of bone and rheumatic disorders in patients with diabetes.
1. Musculoskeletal disease in diabetes
Various musculoskeletal disorders have been associated with diabetes. These disorders may cause pain and functional impairment, and influence the ability of patients to adhere to other aspects of diabetes treatment, particularly exercise and weight management. Therapies commonly used in the treatment of rheumatic diseases, particularly corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), may be particularly problematic in patients with diabetes. The important bone and joint disorders associated with diabetes discussed in this chapter are outlined in Table 1.
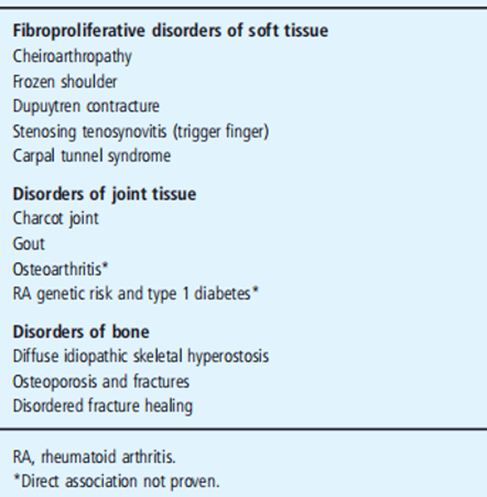
Table 1: Bone and joint disorders in patients with diabetes.
2. Fibro proliferative disorders of soft tissue
Limited joint mobility (cheiroarthopathy) Limited joint mobility refers to joint contracture syndrome resulting in decreased passive mobility of the joints in patients with diabetes [1]. Flexion contractures of the proximal interphalangeal (PIP) joints and metacarpophalangeal (MCP) joints of the hands are characteristic, with the fifth PIP joint being affected first (Figure 1).
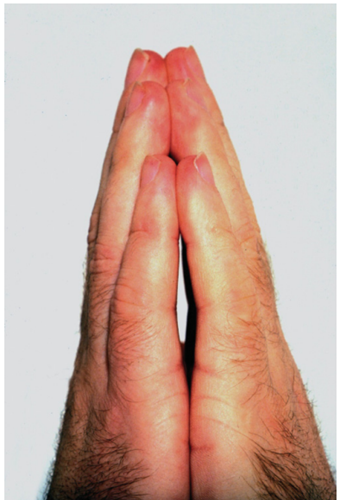
Figure 1: Limited joint mobility with flexion contractures affecting the finger proximal interphalangeal joints. Courtesy of Dr. Tim Cundy.
The skin on the dorsum of the hands typically appears tight and waxy [2]. Large joints such as the wrists, elbows, the ankle and cervical spine can also be affected, and reduced lung volumes have been reported in severe cases [3, 4]. Pain is usually mild or absent early in the disease, and features of synovitis such as Joint swelling, effusion, warmth, and tenderness were typically absent. The disorder can be readily differentiated from systemic sclerosis by lack of Raynaud phenomenon and other systemic features, normal nail fold capillary examination results, and negative autoantibodies [5, 6].
The presence of limited joint mobility of the hands is detected clinically by assessing the Prayer sign or tabletop sign. The Prayer sign is positive if patients are unable to oppose the palmar surfaces at any interphalangeal or MCP joints when the hands are placed in the Prayer position. To assess the tabletop sign, the patient placed both hands on a tabletop with the palms down and fingers fanned out. The fingers were then viewed at the table level. In Stage 0, the entire Palmer surface of the fingers makes contact with the table. In stage 1, one finger is affected (usually the fifth PIP joint in one or both hands). In stage 2, two or more fingers of both hands are affected (usually the fourth, and fifth PIP joints, respectively). In stage 3, there is involvement of all fingers and restricted movement in a larger joint, usually the wrist or elbow [7]. Passive joint movement should also be assessed to confirm the limitations of joint mobility [8]. Prevalence estimates for limited joint mobility in type 1 diabetes mellitus (T1DM) range from 9% to 58%, and 25% to 75% in type 2 diabetes mellitus (T2DM) [1, 9–11]. There is some evidence that prevalence rates have declined in patients with T1DM in the last 20 years because of improvements in glycemic manipulation [12]. Constrained joint mobility is essential in most cases because of the medical institution. It is one of the earliest headaches in diabetes and is strongly related to the presence of microvascular complications, including retinopathy and nephropathy in T1DM [1, 12–15], and macro vascular complications in T2DM [10]. It is also associated with other fibro proliferative disorders that affect the higher limbs, including frozen shoulder, upper trunk contractures, and carpal tunnel syndrome [15–18]. Limited joint mobility does not critically impact hand function; however, mixtures of these higher-limb disorders may additionally motivate higher-limb incapacity [19 – 21]. In addition to microvascular complications, chance elements for the improvement of confined joint mobility Patients with diabetes include older age, puberty (T1DM), disordered periods, and cigarette smoking [10, 22–24]. Advanced imaging strategies have confirmed thickening of the skin, tendons, and tendon sheaths in patients with restricted joint mobility [25, 26]. Histologic examination of the pores and skin suggests altered mucopolysaccharides distribution, elastin, and collagen, and decreased vascular lumen [27]. Non-enzymatic glycosylation and accumulation of collagen have been implicated in pathogenesis [28]. Disordered glycosaminoglycan (GAG) metabolism is likewise a characteristic; pores and skin biopsies from patients with extremely limited joint mobility show stated hyaluronan expression inside the dermis and diminished expression inside the epidermis and basement membrane as compared with skin from controls without diabetes and controls without diabetes but without restrained joint mobility [29]. in addition, elevated urinary GAG excretion has been pronounced in sufferers with restrained joint mobility [30]. reduced circulating insulin-like growth aspect I (IGF - I) is related to restricted joint mobility, implicating the growth hormone IGF - I axis in the pathogenesis of the hassle [31]. Microvascular abnormalities also contribute to disease, with reviews of disordered palmar microvascular flow in response to thermal tasks [32].
The mainstay of this remedy remains to reap wonderful glycemic management and decrease the occurrence of this disorder, as has been said with such interventions [12, 33]. Physiotherapy, particularly hands This treatment may be beneficial in enhancing joint contractures and characteristics. Corticosteroid injection of flexor tendon sheaths has been shown to cause finger contractures in nearly two-thirds of cases related to restricted joint mobility and needs to be considered [34].
2.1 Frozen shoulder
This ailment is characterized by shoulder aches, stiffness, and a critically restricted range of motion in all planes [35]. Three phases of the disorder are well recognized: first, the painful freezing stage with associated nocturnal pain (lasting 4–8 months), accompanied by the aid of the adhesive section with development in aches but with a severely restricted variety of motion (lasting 8–24 months), and finally, the resolution section [36]. The suggested time to make a decision is 30 months [36]. Plain radiographs of the shoulders were normal. Even though the circumstances are typically self-proscribing, some patients have chronic shoulder aches and a restricted variety of movements a few years after assessment [37, 38]. Imaging and histologic studies have proven that the pathologic functions of a frozen shoulder include thickening of the capsule and synovium with reduced joint extent. The affected tissue is characterized by dense type I and III collagen deposition with proliferating fibroblasts and a chronic inflammatory infiltrate comprising T cells, macrophages, and mast cells [39, 40].
Disordered collagen synthesis and vascular endothelial growth factor 1 (VEGF-1)-mediated angiogenesis have also been implicated [41, 42]. The remedy is tailored to the degree of the ailment [35]. in the painful freezing stage, analgesics, inclusive of NSAIDs if tolerated, are indicated. Early use of intra - articular corticosteroids is related to progressed results, and physiotherapy with exercise inside the limits of ache is of greater benefit than more intensive physiotherapy, which includes stretching and mobilization [43, 44]. although oral corticosteroids provide short-term comfort inside the painful freezing level, they are no longer mechanically advocated because of the lack of long-term benefits and the danger of destructive events [45] More extensive physiotherapy was indicated for the adhesive segment. For those who fail to respond to physiotherapy and have continual shoulder restriction, interventions consisting of radio-image-dehydroxylation-oxidation, manipulation under anesthesia, or arthroscopic release should be considered [46, 47].
Diabetes primer risk factor for a frozen shoulder. The prevalence of frozen shoulder is 11–19% in patients with diabetes compared with 2–3% in age-matched controls [16, 19, 48, 49].
Patients with diabetes are more likely to have bilateral ailments. Key hazard factors for frozen shoulders in patients with diabetes are older age, period of diabetes, previous myocardial infarction, retinopathy, and peripheral neuropathy [50]. The presence of other fibro proliferative musculoskeletal problems, which include confined joint mobility and Dupuytren contractures, is strongly associated with the frozen shoulder in sufferers with diabetes [50]. moreover, frozen shoulder in patients with diabetes is more difficult to manage due to continual ailment and worse outcomes following surgical interventions [47, 51, 52].
2.2 Dupuytren contractures
Dupuytren contracture is a fibro proliferative ailment of the palmar fascia that leads to the formation of palmar nodules, improvement of a palmar aponeurosis wire with tethering of the overlying pores and skin, and flexion contractures, mainly affecting the ring and little fingers [53]. Elderly people of Northern European ancestry are most frequently affected. Disordered fibroblasts and my fibroblast feature has been described, with the deposition of type III collagen, potentially mediated via boom factors inclusive of remodeling increase thing β (TGF-) and primary fibroblast growth thing [54–56].
Surgical treatment is the mainstay of therapy, although non-surgical options, especially near collagenase injections, are promising [57]. Splinting and intralesional corticosteroids might also be considered but are ineffective [58]. A surgical referral must be taken into consideration in the presence of contractures. diverse surgical approaches are available, which include fasciotomy (division of the affected palmar fascia) or fasciotomy (excision of the affected palmar fascia). Percutaneous needle fasciotomy is a minimally invasive approach with accurate short-term results, although recurrence is a frequent problem [59, 60].
Danger elements for Dupuytren contractures include older age, male intercourse, cigarette smoking, guide labor, and alcohol consumption. Diabetes is also a critical danger factor for Dupuytren contracture, which is present in up to 26% of patients with diabetes [19,20,61]. Age and disease length are major risk factors for the improvement of Dupuytren contracture in patients with diabetes [62]. Dupuytren contractures are also related to microvascular clear headaches in T1DM and macro albuminuria in T2DM [63,64]. Rapid modern contractures are less frequently observed in patients with diabetes [62]. The co-proliferator-activated the e disease is frequent in patients with diabetes-associated Dupuytren contractors, with better rates of confined joint mobility [64].
Stenosing tenosynovitis (trigger finger)
Finger is “a condition in which the flexor tendon is prohibited from gliding through the tendon sheath because of thickening of the synovial sheath over the tendon” [65]. This disorder most often affects the ring finger; however, it can also affect the other fingers and thumbs. The affected person might also record a clicking sensation while transferring the finger, discomfort over the palm, or overt triggering when the finger is locked in flexion [66]. Nodular or diffuse flexor tendon sheath swelling is palpable. The syndrome takes place as a result of a discrepancy between the flexor tendon and its sheath within the A1 pulley at the level of the metacarpal head [66]. The pulley thickens with extracellular matrix and fibrous cartilage metaplasia [67].
These pathological changes can be precipitated by repeated trauma. Corticosteroid injection into the tendon sheath is a powerful therapy for most patients, particularly in the presence of nodular ailments. For patients with nodular sickness lasting less than six months, the local injection has a reported fulfillment rate of 90% [68]. Splinting and hand therapy are beneficial adjuncts to local injection. If a conservative remedy fails, the use of a percutaneous needle technique or open surgery is indicated [69]. sufferers with diabetes are at greater risk of trigger finger, with a lifetime chance of 10% compared to 2.6% of the overall population [66]. The affected person's age, diabetes duration, and presence of microvascular complications are associated with multiple hazards of trigger finger in diabetes [62, 70]. Effects are commonly worse while the cause of fi finger is related to diabetes, with decreased responses to corticosteroid injection and a greater need for surgical operation [71–73]. furthermore, T1DM is associated with a better incidence of sickness, more affected digits, a greater need for surgery, and a higher risk of recurrence [62, 71, 73].
2.3 Carpal tunnel syndrome
Carpal tunnel syndrome is a not unusual compressive neuropathy affecting the median nerve as it traverses with the flexor tendons through the carpal tunnel, an anatomical space made out of the carpal bones and transverse carpal ligament [74]. The most common histological appearance is non-inflammatory tensional fibrosis, with elevated fibroblast range and type III collagen deposition, most likely mediated by TGF- [75]. Compression within the carpal tunnel leads to a disordered microvascular supply of the nerve, causing demyelination and axonal degeneration. The standard presentation is hand paresthesia, particularly affecting the thumb, index finger, and central finger. Paresthesia is frequently greater frequent at night and can wake the affected individuals from sleep. Wrist and hand pain may also occur and sufferers often report hand clumsiness.
The clinical of l examination may be normal; however, in the presence of intense and prolonged ailments, there may be features of median nerve denervation, which include then factor the point of thumb abduction, and sensory loss over the median nerve distribution. Provocative assessments such as the Phalen and Tinel exams can be positive, and if present, have rather excessive specific metropolises for carpal tunnel syndrome. The Phalen test is effective if paresthesia inside the median nerve distribution is reported following flexion of the wrist at 90 ° for 60 s. Tinel check is effective if paresthesia is reported after tapping the volar wrist over the carpal tunnel.
The diagnosis is confirmed by nerve conduction testing, with traditional findings of prolonged latencies and delayed conduction velocities affecting the median nerve throughout the wrist [76]. Treatment includes preserving the wrist in a neutral position and using a detachable wrist splint. Splinting is particularly beneficial for nocturnal signs and symptoms and can be sufficient to treat mild diseases [77]. Even though oral corticosteroids have short-term efficacy, the results are usually unacceptable [78]. A nearby corticosteroid injection provided short-term relief [79]. Surgical launch under neighborhood anesthesia is a well-tolerated and effective treatment that must be considered in patients who have failed conservative treatment or have extreme signs and symptoms of nerve compression [80]. Open-release and endoscopic approaches have comparable scientific results [81].
Carpal tunnel syndrome may be due to various factors, including non-specific c flexor tenosynovitis affecting the wrist, rheumatoid arthritis and different inflammatory synovial arthropods, weight problems, pregnancy, and disordered wrist anatomy [74].
Diabetes is one of the most common metabolic issues associated with carpal tunnel and is found in 16% of affected sufferers [82]. Studies have shown the extended danger of carpal tunnel syndrome in patients with T1DM and T2DM [62, 83, 84]. The latest survey on the use of scientific and neurophysiologic assessment showed a 2% occurrence of carpal tunnel syndrome in a reference population without diabetes, 14% in patients with diabetes but no diabetic polyneuropathy, and 30% in patients with diabetic polyneuropathy [85]. Carpal tunnel syndrome is related to periods of diabetes and is frequently present in patients with microvascular complications, such as retinopathy, nephropathy, and polyneuropathy [62,86].
Carpal tunnel syndrome is also more common in patients with limited joint mobility, and it has been postulated that this disorder occurs at higher frequency in diabetes because of accelerated thickening and fibrosis of the flexor tendon sheaths within the Carpal tunnel [18]. Glycosylation of collagen may also reduce the compliance of connective tissues within the carpal tunnel [84]. In addition, the presence of the existing microvascular disease may further increase the risk of endoneurial ischemia, as the median nerve travels through the carpal tunnel. Carpal tunnel syndrome may be more difficult to assess in patients with coexistent diabetic neuropathy owing to atypical presentation and neuro physiological assessment [85,87]. The treatment options for patients with diabetes and carpal tunnel syndrome are similar to those for patients without diabetes, and responses to surgery are usually good [88,89]. One study reported positive results in symptom scores and neurophysiologic testing using local insulin injections in women with T2DM and carpal tunnel syndrome in combination with corticosteroid injection [90].
Disorders of joints
2.4 Charcot joint
Charcot's weakest joint is a destructive arthropathy that most commonly affects patients with diabetes in the presence of severe peripheral neuropathy. This disorder affects 0.1 – 0.4% of patients with Diabetes may lead to severe foot deformities, disabilities, ulcerations, and limb amputations [91].
Several stages of the disease have been described [92,93]. The developmental stage presents as acute inflammation with swelling, warmth, and erythema of the feet. Pain may be a feature, despite presence of peripheral sensory neuropathy. Peripheral pulses are usually palpable. Gradually worsening deformity occurs with bone resorption, fracture, and dislocation, leading to instability of the foot and classic rocker-bottom dislocation of the mid foot. Plain radiographs may appear normal early in the acute phase of the disease (Stage 0), but magnetic resonance imaging (MRI) scans show fl or bone marrow edema, subchondral cysts, micro fractures, and bone scientist showing increased uptake in the bony phase [93]. As deformity develops, radiographs show severe osteolysis, bone fragmentation, and disordered architecture (stage 1). In the coalescence phase (Stage 2), hyperemia resolves, swelling is reduced, and the skin temperature normalizes. Bone debris is resorbed and bone sclerosis may occur. The reconstructive stage (stage 3) is characterized by bone remodeling, ankylosis, bone proliferation, and the formation of a stable foot. The acute phase (stages 0 and 1) typically lasts 2 – 6 months, while the reparative phase (stages 2 and 3) lasts up to 24 months. During both the acute and the reparative phases of the disease, the bony deformity may lead to abnormal load-bearing, ulceration of the overlying skin, and secondary osteomyelitis.
Five separate patterns of foot involvement are identified in patients with diabetes [94]: I, affecting the forefoot with osteolysis of the MTP and IP joints of the feet, leading to the “sucked candy” appearance on plain radiography; II, affecting the tarsometatarsal (Lisfranc) joint leading to instability, subluxation, and fracture (Figure 2); III, dislocation and fracture affecting the mid tarsal and naviculocuneiform joints; IV, affecting the ankle and subtalar joints, often with severe osteolysis; and V, affecting the calcaneus. The most common patterns are II and III, and combinations of these patterns may be present. Bilateral disease was present in one-quarter of the patients. Rarely, other joints, such as the knees, elbows, and shoulders, are affected.

Figure 2: Plain radiograph of Charcot foot. Note the osteolysis, bone fragments, subluxation and fracture affecting the tarsometatarsal joints of the foot. Courtesy of Dr. Tim Cundy.
The etiology of this disease remains controversial [95]. Minor trauma frequently precipitates the onset of disease and may lead to sub clinical recently benefited recently weak bone injury that triggers an aberrant inflammatory response [96]. Disordered weight-bearing in joints affected by peripheral neuropathy likely leads to repetitive injury and instability (neuro traumatic hypothesis). Additionally, autonomic dysfunction causing vasodilation, arteriovenous shunting, and hyperemic bone resorption has been implicated (the neuro vascular hypothesis). The development of osteopenia and site lysis increases the risk of fractures in the presence of abnormal load bearing with a cycle of joint instability and fracture development, causing further abnormal load bearing [97]. Recent studies have focused on the role of local inflammation in the pathogenesis of disease. Advanced imaging and histologic analysis have demonstrated that inflammation of the synovium and bone is evident in Charcot's joint and is characterized by increased expression of the pro-inflammatory cytokines tumor necrosis factor α (TNF) and interleukin 1 [98–101]. Large numbers of osteoclasts are present within the affected bone, and patients with Charcot's joint have an increased ability to form peripheral blood-derived osteoclasts in vitro compared to diabetic and non-diabetic controls [101,102]. Markers of bone resorption are increased in patients with acute Charcot joint [103]. Interestingly, acute phase markers were not significantly elevated, indicating an apparent dissociation between local and systemic inflammatory diseases [104]. These statistics implicate receptor activator of nuclear aspect κ B ligand (RANKL) mediated osteoclastogenesis is pushed locally through pro-inflammatory cytokines and offers a rationale for the use of sellers that target osteoclasts in the treatment of sickness. The control of Charcot's joint depends on the stage of the disorder. Treatment for the duration of the acute phase consists of immobilization, which reduces infection, prevents extraordinary load-bearing, and stabilizes the foot in a position of minimal deformity. The same old immobilization approach used throughout the acute phase is a non-weight-bearing general touch cast. This treatment calls for close tracking and normal adjustment should be maintained until swelling and temperature normalize, and radiographs show no further bone destruction [105]. Some recent out-of-control reviews have indicated that the use of a weight-bearing overall touch solid can be an appropriate opportunity for a non-weight-bearing option; however, managed trials are not yet available [106,107].
The recognition that the extreme segment of the Charcot's joint is associated with immoderate osteoclast activity has brought about the trying out of dealers targeting bone turnover for the treatment of this situation. randomized managed trials of bisphosphonates had been said, and each displayed efficacy. An unmarried intravenous infusion of 90 mg pamidronate in an examination of 39 sufferers with acute Charcot joint caused giant upgrades in symptoms and bone turnover markers [108]. In a study of 20 patients with acute Charcot joint, weekly oral management of 70 mg alendronate for 6 months changed related to sizable upgrades in pain rankings, bone turnover markers, and foot bone density [109].
A randomized trial of intra nasal calcitonin confirmed its efficacy regarding bone turnover markers; however, no variations in clinical variables have been reported [110]. The efficacy of TNF inhibitors and different antiresorptive retailers, such as the RANKL inhibitor denosumab, have not yet been studied in the Charcot's t joint, even though the potential use of these dealers has been recognized [96].
Surgical procedures are usually no longer considered first-line remedies, even though one observer has suggested correct surgical consequences following debridement, open reduction, and internal fixation with autologous bone grafting in the acute phase of the disorder [111]. In popular opinion, surgical management is currently recommended for patients in the reparative (rather than the acute) segment of the disorder, specifically for patients with deformities related to continual foot ulcers and joint instability. Numerous surgical techniques for arthrodesis may be used, consisting of open discounts with internal and external fixation, relying on the presence of nearby infection and different anatomic variables [112]. Different surgical treatments consist of osteotomy, intramedullary rodding, and amputation. contamination, non-union, and triggering of acute Charcot responses are crucial for postoperative headaches and cautious postoperative control is important. The effects on patients with Charcot's foot are frequently disastrous. A current evaluation of hundred and fifteen sufferers stated that non-operative management is associated with a 2.7% annual rate of amputation, a 23% risk of requiring bracing for greater than 18 months, and a 49% risk of recurrent ulceration. The presence of open ulcers at initial presentation or chronically recurrent ulcers is associated with an increased risk of amputation.
2.5 Gout
Gout is an inflammatory arthritis caused by intraarticular deposition of Monosodium urate (MSU) crystals. This disorder is the most common form of inflammatory arthritis, affecting men and affects 1–2% of the Caucasian adult population. In the early stages of the disease, gout presents as recurrent episodes of self-limiting acute inflammatory attacks (“flares”) of arthritis. These Attacks most often affect the first MTP joint, mid foot, and ankle. In the presence of prolonged hypercalcemia, some patients develop recurrent poly articular attacks and chronic tophaceous disease, and erosive arthritis (Figure 3).

Figure 3: Chronic tophaceous gout of the hands in a patient with type 2 diabetes.
The key risk factors for gout are hyperuricemia, male sex, chronic renal impairment, hypertension, obesity, diuretic use, coronary heart disease, and seafood, meat, and alcohol intake.
The relationship between gout and metabolic syndrome is well established. Serum urate concentrations and gout are strongly associated with abdominal adiposity and have been predicted T2DM. Patients with gout have higher rates of metabolic syndrome and T2DM than those without gout. The promotion of renal Tubular reabsorption of uric acid by insulin is thought to mediate this relationship. The recent identification of the glucose and fructose transporter SLC2A9 as a key regulator of serum urate concentrations suggests a further etiologic link between hyperuricemia and hyperglycemia. A recent study reported a 22% prevalence of gout in patients with T2DM treated in secondary care. The key risk factors for gout in this population are male sex, renal impairment, and diuretic use. Fewer than half of the patients with gout and diabetes in this study were prescribed urate-lowering therapy, and only 8% had a serum urate level < 0>
Options for the treatment of acute gout flares include NSAIDs, corticosteroids, and/or colchicine. Long-term urate-lowering therapy is indicated for patients with gout who have recurrent flares, gouty arthropathy, tophi, or radiographic damage. Serum urate level lowering to a concentration of < 0>
Initiation of urate-lowering therapy is frequently associated with exacerbation of gout flares; this side effect can be avoided by the commencement of urate-lowering therapy once the acute flare has resolved, gradual introduction of the urate-lowering drug, and co-prescription of low-dose colchicine.
The presence of coexisting gout has several implications for individuals with T2DM. Poorly controlled gout may hinder exercise attempts and weight loss. In addition to the dietary restrictions required for glycemic control, these patients also need to avoid consuming alcohol- and purine-rich foods. Diuretic therapy may exacerbate hyperuricemia and should be avoided in patients with gout unless required. Drugs such as losartan and fen of vibrate have weak urate-lowering effects and may be of particular benefits in patients with diabetes and gout if antihypertensive or lipid-lowering therapy is required.
Prolonged cartilage loading is an important factor in the development of osteoarthritis, and joint stiffness is an important part of the burden and joint problems. Although some studies have reported the measurement of T2DM and osteoarthritis, the use of the waist mass index (BMI) is not well-controlled. T2DM was not a risk factor for the development of osteoarthritis in most (but not all) BMI-adjusted studies. According to the model, today's analysis shows that the increase in BMI is replacing T2DM as a good time for osteoarthritis development. The association between rheumatoid arthritis and T1DM involves many genetic mechanisms, including PTPN22, HLA-DR9, loci on chromosome 4q27, and proximity to IDDM5 and IDDM8. There is also evidence that these problems affect one's family. 2. Eight percent of immediate family members of patients with rheumatoid arthritis have type 1 diabetes, compared to 0.35% of the general population. However, based on these observations alone, there may be little evidence of long-term arthritis in patients with type 1 diabetes. Bone pain in diabetes mellitus: diffuse idiopathic skeletal hypertrophy. Ossification of the anterior longitudinal ligament is common in the thoracic spine (Figs. 40–84). Extraspinal ossification is also observed. There are higher ones. We recommend a rate of 15% for women and 25% for men. to > 50). Although it is controversial whether DISH is associated with pain and stiffness, affected individuals may also experience pain and stiffness.
3 Osteoarthritis
Increased load-bearing of articular cartilage is an important risk factor for the development of osteoarthritis, and a strong positive relationship has been reported between obesity and the risk of the development of osteoarthritis. Although some studies have reported an association between T2DM and osteoarthritis, most studies have not adequately controlled for body mass index (BMI). In
In most (but not all) studies that have adjusted for BMI, T2DM was not an independent risk factor for the development of osteoarthritis. Overall, the current data indicate that increased BMI, rather than T2DM, is a risk factor for the development of osteoarthritis.
3.1 Rheumatoid arthritis
Rheumatoid arthritis and T1DM share several genetic associations, such as PTPN22, HLA - DR9, chromosome 4q27 region, IDDM5 region, and IDDM8 region. Furthermore, there is evidence of familial clustering of these disorders; 2.8% of first-degree relatives of probands with rheumatoid arthritis have T1DM, compared to 0.35% of the general population. Despite these observations, there is little evidence that the prevalence of rheumatoid arthritis is increasing in patients with T1DM.
Diffuse idiopathic skeletal hypertrophy (DISH) results from bone formation, particularly in tissues (connective and tendon insertion into the bone). Ossification of the anterior longitudinal ligament of the spine typically occurs in the thoracic spine. can also be used to identify fossils. A prevalence of up to 15% in women aged 50 years and 25% in men has been reported. This article is about harassment back pain, which is frequently detected as an incidental finding on chest radiographs. Rare complications such as dysphagia, vocal cord paralysis, compression of the inferior vena cava, and neurologic compression syndromes have been in patients with fl-rid hyperostosis. Spinal fractures may occur after a relatively minor injury and cause significant neurologic compromise. The diagnosis is made radio graphically, according to the Re Snick criteria, which are as follows:
Most case series have identified both obesity and T2DM as risk factors for DISH. The presence of additional metabolic disorders such as dyslipidemia or hyperuricemia further increases the risk of DISH is associated with diabetes. Patients with DISH have higher rates of hyperglycemia and circulating insulin levels, particularly after a glucose load. Obesity is likely to have direct biomechanical effects because of the increased load on the entheses. Additionally, systemic factors may contribute to the development of DISH, as patients with this disorder have evidence of increased bone mineral density (BMD) elsewhere in the skeleton. Insulin, growth hormone and IGF - I have been implicated in the pathogenesis of DISH, and high circulating concentrations of these hormones may contribute to the development of hyperostosis. High expression of nuclear factor κ B (NF κ B), platelet-derived growth factor-BB, and TGF - β 1 have also been reported in the affected tissue in patients with DISH, implicating these factors in osteoblasts Activation and new bone formation.
4 Osteoporosis and fractures
4.1 Background
Fragility fractures are a major cause of morbidity and public health expenditures. The most devastating fracture, that of the proximal femur, is associated with a 20% risk of dying within 6 months and a substantial risk of loss of independence. Individual fractures are associated with considerable periods of disability and loss of productivity. The number of fractures occurring annually is rising steadily, as a result of both the aging of the world population and an age-specific increase in some countries. Important risk factors for fragility fractures include low BMD, older age, female sex, light body weight, previous fracture, cigarette smoking, and glucocorticoid use. Dual-energy X-ray absorptiometry (DEXA) is currently the preferred modality for BMD measurements. Recently, absolute fracture risk algo rhythms have been developed using these risk factors, to provide 5- – 10-year estimates of the risk of any osteoporotic fracture, or hip fracture. Insight into the mechanism(s) by which bone loss occurs can be gained by measurement of biochemical markers of bone turnover, which reflect either osteoblasts function/bone formation or Osteoclast function and bone resorption. At present, bone markers are important tools for evaluating the pathogenesis and treatment of osteoporosis in clinical studies, but their utility in the management of individual patients is limited by assay variability, low predictive value for skeletal events, and high costs. In recent years, evidence has shown that the risk of fragility fractures is increased in both types of diabetes, albeit through different mechanisms. In addition, attention has recently been focused on the skeletal effects of T2DM treatments, particularly thiazolidinediones.
Fracture epidemiology in diabetes
5 Type 1 diabetes
Two recent meta-analyses of observational studies examined the relationship between T1DM and the risk of fracture. Hip fracture is the only fracture type evaluable in these analyses, owing to the paucity of studies on other fracture types. Both meta-analyses demonstrated a substantially increased (six- to nine-fold) relative risk of hip fracture in T1DM. Studies of other fracture types in T1DM are few and may include only a small number of events, but they generally support the notion that non-vertebral fracture risk is increased, with relative risk estimates of 1.3 – 3 for any fracture and 2.4 for foot fractures. The only study to date to assess vertebral fracture risk in T1DM found no increase.
6 Type 2 diabetes
Until quite recently, little information was available as to the skeletal consequences of T2DM; however, recent epidemiologic studies have suggested that fracture risk is increased in that disease. Meta-analyses of these observational studies report an increased risk of all fractures, and also those of the hip, forearm, and foot. Relative risk estimates for hip fracture are lower in T2DM (1.4–1.7) than in T1DM, and the estimates of fracture risk at other sites in T2DM range from 1.2–1.4. Since the meta-analyses were published, the Women s Health Initiative (WHI) An observational study, which included > 5000 postmenopausal women with T2DM, reported increased risks of fractures at several specific sites, including the hip, spine, foot, and upper arm. Risk estimates ranged from 1.2 – 1.5 across skeletal sites. The WHI study was one of the few to evaluate vertebral fractures. Although there was an increased risk of spinal fractures in the WHI study, it remains uncertain whether the risk of this fracture type is higher in T2DM, as other studies have not found an association.
7 Mechanisms of Skeletal Fragility in Diabetes
Although fracture risk appears to be increased in both T1DM and T2DM, there are likely important differences in the mechanisms by which skeletal fragility is increased in the two (Table 2). At least two mechanisms underlie increased skeletal fragility in patients with T1DM. The majority of cross-sectional studies on T1DM have reported decreased BMD throughout the skeleton, although there is no consistent association between the age of participants, duration of disease, and magnitude of BMD, deficit. Interestingly, studies performed in children and young adults demonstrated lower than-normal BMD of the hip and spine at the time of diagnosis. Taken together with the observations from longitudinal studies that BMD does not progressively decline in T1DM, and cross-sectional studies of middle-aged subjects with T1DM that report normal levels of markers of bone turnover, these data suggest that the observed defects in BMD in T1DM occur early in the course of the disease and perhaps before its clinical presentation. It is likely that the deficiency of insulin and other pancreatic β-cell hormones, such as amylin and preptin, each of which has been implicated in skeletal homeostasis, contributes to the decreased BMD observed in T1DM. Recent data also implicate low levels of IGF - I in the pathogenesis of cortical bone loss in T1DM. Insulin deficiency alone is probably not sufficient to explain the lower BMD because insulin therapy does not affect BMD. Lower body weight may also be a factor, there was a strong positive relationship between weight and BMD.
The magnitude of the reduction in BMD (3 – 8%) is probably insufficient to explain the higher fracture rates in T1DM. A second mechanism by which skeletal fragility is likely to increase is an increased propensity to fall because of disease complications. Neuropathy, visual impairment, cerebrovascular disease, and hypoglycemia are likely to increase the risk of falls. In the only study to date that has evaluated this possibility, substantially higher risks of hip fracture were observed in T1DM patients with a range of disease complications than in those without complications. Neuropathy may also impact adversely on BMD in the distal limbs, as patients with T1DM and neuropathy are associated with a lower cortical bone mass in the distal limbs than in those without neuropathy. Animal studies suggest that interruption of nerve supply to bone decreases regional bone mass, independent of changes in mechanical loading. The presence of regional osteopenia likely contributes to the increased risk of distal limb and foot fractures in patients with T1DM.
The mechanism(s) by which skeletal fragility increases in T2DM are uncertain (Table 2).
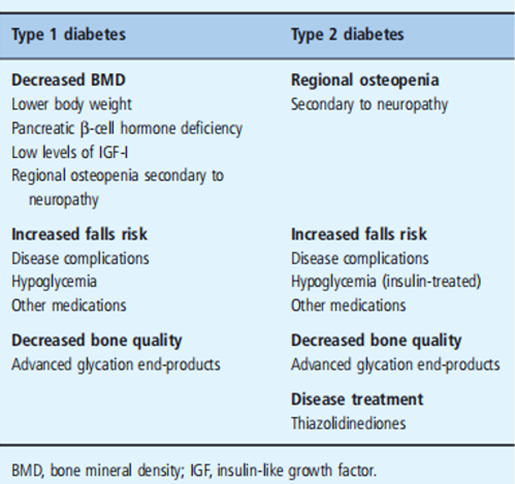
Table 2: Mechanisms of increased skeletal fragility in diabetes.
The observation that fractures risk is increased is in some ways surprising because the higher the body weight that commonly accompanies T2DM might be expected to preserve bone mass and protect patients from adverse skeletal outcomes. BMD in the axial skeleton is higher in subjects with T2DM than in subjects without diabetes; however, BMD remains an important risk factor for fracture in T2DM, because incident fractures occur more frequently in subjects with T2DM and decreased BMD compared to those with normal BMD. The limited available evidence suggests that T2DM patients with neuropathy and nephropathy had a lower BMD than those free of these complications.
As in T1DM, it is likely that complications of T2DM, such as neuropathy, vascular disease, and impaired vision, increase the risk of falling, and thereby of fracture. In the Study of Osteoporotic Fractures, a Prospective study of fracture Epidemiology in older American women, participants with T2DM had a 22% higher risk of non-spine fractures than participants without diabetes.
Participants with T2DM who were treated with insulin had both a higher prevalence of disease complications and a higher risk of fracture than those with T2DM who were not treated with insulin.
In the Health ABC study, a prospective study of older (> 70 years)
American men and women, there was a strikingly higher prevalence of neuropathy, cerebrovascular disease, and falls in participants with T2DM who developed a fracture than in those with T2DM who did not fracture. Many risk factors for falls, including the use of medications associated with increased fall risk, are more commonly present in those with T2DM than in the population without diabetes. Low-impact falls are more frequent in insulin-treated patients with diabetes than in healthy controls. Curiously, adjusting for diabetes complications and/or fall risk did not attenuate the increased fracture risks observed in T2DM.
Aspects of bone strength and/or quality that are not captured by DEXA assessment may be abnormal in patients with either type of diabetes and contribute to increased bone fragility. At present, there is no validated methodology for assessing these aspects of bone quality. Potentially relevant to this hypothesis is a growing body of evidence that advanced glycation end-products (AGE), products of non-enzymatic glycation, are present in greater amounts in the skeletons of diabetic animals than those of non-diabetic animals. The glycation of the matrix proteins in bone may alter biomechanical properties in such a way as to decrease bone strength. In vitro, studies suggest that AGEs inhibit the differentiation of osteoblasts and increase the differentiation of osteoclasts [204], thereby potentially altering bone remodeling and/or strength in a detrimental fashion. There may be AGE-specific effects on bone remodeling, as pentosidine decreases osteoclast development in vitro; however, mice deficient in the receptor for AGE exhibit increased bone mass and decreased osteoclast function, suggesting that the overall effect of increased AGE signaling in bone is likely to be detrimental.
Finally, in T2DM, there is clear evidence that treatment with either of the currently available thiazolidinediones (TZDs), rosiglitazone and pioglitazone, increases fracture risk, at least in women. Data collected as adverse events during the conduct of randomized controlled trials of each TZD in middle-aged populations of those with T2DM demonstrated a twofold increase in the risk of distal limb fractures in women, although not in men. Observational data from an older cohort of patients with T2DM suggests that fracture risk is also increased in men exposed to TZDs and that the incidence of “classic” osteoporotic fractures (hip, forearm, humerus) is also higher in TZD users.
The mechanisms underlying the adverse skeletal effects of TZDs are complex and likely to involve both direct and indirect pathways (Figure 7). Of primary importance is the effect of the TZDs to inhibit bone formation directly, by diverting men's chemical stem cell precursors from the osteoblasts to the adipocyte lineage. A substantial body of preclinical studies in rodents, and data accruing from studies in humans, demonstrates that TZDs decrease bone formation and BMD in vivo. In addition, TZDs increase or maintain bone resorption at appropriate lately elevated levels, via direct actions on osteoclast development. Indirect actions of TZDs that potentially contribute to their detrimental skeletal effects include decreasing systemic and skeletal production of IGF - I, modulating production of skeletally active adipokines, and decreasing levels of pancreatic β - cell hormones with known skeletal activity. The skeletal toxicity of TZDs has prompted interest in the effects of other oral hypoglycemic agents on bone health. At present, the available data suggest that metformin and sulfonylureas are neutral regarding the skeleton.
Investigation and management of osteoporosis in d diabetes Diabetes of either type should be regarded as a risk factor for fragility fracture, and included in clinical fracture risk assessment, along with recognized risk factors such as age, gender, body weight, previous fracture, cigarette smoking, glucocorticoid use, and BMD. Recently developed fracture risk algorithms may help determine an individual patient’s short to medium-term absolute fracture risk. Although BMD is on average increased in T2DM, measurement of BMD in patients with T2DM is still helpful in defining that person’s fracture risk. Prescription of TZDs to patients with T2DM who are found to be at high risk of fracture should be avoided unless there are compelling reasons to do so. Minimizing fall risk is an important component of skeletal management in diabetes – this can be achieved by targeting both macro vascular and microvascular disease complications, minimizing the risk of hypoglycemia, optimizing visual acuity, and minimizing the use of other medications known to be associated with falls. Although there are no data from interventional studies on the effects of pharmacologic treatments of osteoporosis in diabetes, it is reasonable to assume that agents are known to prevent fractures in non-diabetic osteoporotic populations, such as bisphosphonates, will also be effective in those with diabetes.
Fracture healing in diabetes
A growing body of evidence suggests that fracture healing is abnormal in those with diabetes. In rat models of T1DM, the mechanical and structural properties of the healing bone are inferior in diabetic rats when compared with control animals, findings that are accompanied by evidence of both decreased callus size and collagen content. Interventional studies demonstrate that therapy with insulin to achieve normoglycemia is associated with fracture healing that is indistinguishable from that observed in non-diabetic animals. Subsequently, administration of insulin at the site of skeletal injury was also shown to promote fracture healing, without altering serum glucose, implying a role for insulin in directly mediating bone repair. Few data are available from human studies, but increased rates of fracture non-union in both T1DM and T2DM have been reported, as having higher-than-expected rates of serious complications in patients with diabetes and open ankle fractures. Further investigation of the influence of diabetes and its treatment on fracture repair in humans is needed.
The research method employed in this study on Bone and Rheumatic Disorders in Diabetes involved a combination of literature review, data analysis, and clinical investigations. Relevant scientific articles, medical databases, and research papers were reviewed to gather existing knowledge on the topic. Patient data from hospitals and clinics were also collected and analyzed to identify patterns and associations between diabetes and bone/rheumatic disorders. Additionally, clinical examinations and tests were conducted on diabetic patients to evaluate their bone health and the prevalence of rheumatic disorders.
The results of the study revealed a significant association between diabetes and an increased risk of bone and rheumatic disorders. Diabetic individuals exhibited a higher prevalence of osteoporosis, osteoarthritis, and other rheumatic conditions compared to non-diabetic individuals. The data analysis also indicated that the risk of bone fractures and joint-related complications was elevated in diabetic patients, especially those with poor glycemic control and longer disease duration.
The findings of this research align with previous studies that have investigated the link between diabetes and musculoskeletal disorders. The underlying mechanisms that contribute to bone and rheumatic issues in diabetes were discussed, such as chronic inflammation, oxidative stress, and impaired bone remodeling due to hyperglycemia. Furthermore, the impact of diabetes medications on bone health and potential interactions between diabetes and existing bone/rheumatic conditions were considered.
The research established a clear correlation between diabetes and bone/rheumatic disorders, emphasizing the importance of recognizing and managing musculoskeletal complications in diabetic patients. It highlighted the need for healthcare providers to incorporate bone health assessments and preventive measures into the standard diabetes care regimen. Additionally, the study suggested that early intervention and proper glycemic control could potentially mitigate the risk of bone-related complications and improve the overall quality of life for individuals with diabetes.
Overall, the findings of this research contribute to the growing body of evidence on the association between diabetes and musculoskeletal disorders. The conclusions drawn from this study may help healthcare professionals develop targeted interventions and treatment strategies to reduce the burden of bone and rheumatic disorders in diabetic patients, leading to better patient outcomes and improved long-term health. Further investigations are warranted to explore specific mechanisms and to evaluate the effectiveness of various interventions in preventing and managing these complications in diabetic individuals.
The crowning glory of this research challenge could no longer be feasible without the contributions and guidance of many individuals and agencies. we’re deeply grateful to all those who performed a position in the achievement of this mission We would also like to thank My Mentor Dr. Naweed Imam Syed Prof. Department of Cell Biology at the College of Calgary and Dr. Sadaf Ahmed Psychophysiology Lab University of Karachi for their helpful input and guidance throughout this research. Their insights and understanding had been instrumental in shaping the direction of this challenge.
I, at this second, declare that: I haven’t any pecuniary or another private hobby, direct or oblique, in any dependence that raises or can also boost a war with my duties as a supervisor of my workplace control.
The authors declare that they have no conflicts of interest.
No Funding was received to assist with the preparation of this manuscript.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
