AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Ujjwal Kumar Chowdhury, M.Ch., Diplomate NB Professor Department of Cardiothoracic and Vascular Surgery AIIMS, New Delhi-110029, INDIA.
Citation: Ujjwal K. Chowdhury., Diplomate NB., Singh S., George N., Hasija S., et al., (2020) Adjustable Vertical Vein Ligation in Supracardiac Totally Anomalous Pulmonary Venous Connection: A Clinical Report of 99 Patients.. J, Clinical Cardiology and Cardiovascular Interventions, 3(8); Doi:10.31579/2641-0419/075
Copyright: © 2020 Ujjwal Kumar Chowdhury, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cardiothoracic Sciences Centre All India Institute of Medical Sciences, New Delhi, India.
*Corresponding author: Ujjwal Kumar Chowdhury, M.Ch., Diplomate NB Professor Department of Cardiothoracic and Vascular Surgery AIIMS, New Delhi-110029, INDIA.
Received: 04 August 2020 | Accepted: 04 September 2020 | Published: 11 September 2020
Keywords: adjustable vertical vein ligature; atrial septal defect; left atrium;
Background: Unligated vertical vein in repaired obstructive totally anomalous pulmonary venous connection (TAPVC) with pulmonary hypertension reduces perioperative pulmonary artery pressure, pulmonary hypertensive crises and improves survival. Our aim was to assess the long-term results of delayed ligation of the vertical vein using an adjustable ligature on survival and reoperations.
Method: A series of 99 consecutive patients (62 males), aged 24.8±55.3 months (range 1 day-25 years; median 4 months) underwent rechanneling of isolated, obstructive and non-obstructive TAPVC with left atrial augmentation, atrial septal fenestration and an unligated vertical vein. An adjustable vertical vein ligature was employed in all patients for later interruption.
Results: Hospital mortality was 5.0% (n=5) with 2 (2%) late deaths. At a mean follow-up of 218.8 (sE± 209.9) months, the actuarial survival was 93.7% (SE± 0.02%; 95% CI: 86.5, 97.1). Postoperatively, all ligatures were tightened gradually over a period of 24-144 hours. Computed-tomographic angiograms during follow-up revealed absence of flow through the vertical vein and ruled out distortion of the left superior pulmonary vein and left brachiocephalic vein.
Conclusions: A patent vertical vein, augmented left atrium and atrial septal fenestration in repaired obstructive and non-obstructive TAPVC with pulmonary hypertension decreased postoperative pulmonary hypertensive crises and improved survival by providing superior hemodynamics. Percutaneously adjustable vertical vein ligature is an expedient, safe and effective technique in these patients in a setting where transcatheter solutions are not available. Use of a percutaneously adjustable ligature around the vertical vein allows gradual tightening of the ligature under optimal physiological conditions, without multiple reoperations (Figure 1).
ASD : Atrial septal defect
CCF : Congestive cardiac failure
CPB : Cardio pulmonary bypass
CPVC : Common pulmonary venous chamber
CVP : Central venous pressure
CT : Computed-tomography
ECMO : Extra corporeal membrane oxygenation
LA : Left atrium
LAP : Left atrial pressure
LCOS : Low cardiac output syndrome
LV : Left ventricle
PA : Pulmonary artery
PAH : Pulmonary arterial hypertension
PAP : Pulmonary artery pressure
RAP : Right atrial pressure
SE : Standard error
SVC : Superior vena cava
TAPVC : Totally anomalous pulmonary venous connection

Figure 1: Graphic display of the study group (n=99) showing the unligated and ligated vertical vein with an unrestrictive common pulmonary chamber-left atrial anastomosis.
Despite fine tuning of surgical techniques and pulmonary vasodilators, recurrent episodes of pulmonary hypertensive crises and low cardiac output remains a significant problem in repaired obstructive TAPVC leading to hemodynamic instability and mortality after surgery [1-4].
Studies have demonstrated that the left atrium lacks both normal compliance and reservoir function and the left ventricle (LV) is non-compliant and dysfunctional in a subset of patients with obstructive TAPVC [5-11]. It is postulated that a patent vertical vein may function as a temporary reservoir for pulmonary venous blood after repair of TAPVC, permit unloading of the volume in the small, non-compliant left-sided cardiac chambers until they are able to grow and adapt to increased flow demands [5, 6, 12, 13]. Not all investigators have accepted these findings or utilized these techniques. Clinical studies on an unligated vertical vein in the setting of obstructive TAPVC are limited and insufficient to generate evidence-based guidelines.
In our previous investigation on ligation versus non ligation, we demonstrated that unligated vertical vein in repaired obstructive TAPVC reduces perioperative pulmonary artery pressure, pulmonary hypertensive crises and improves survival [14]. Subsequently, in 2007, we demonstrated that a percutaneously adjustable vertical vein ligature allows gradual tightening of the ligature under optimal physiologic conditions without reopening the sternum15. In the current study, we did not repeat the above analysis.
The primary objective of this study was to i) determine the short-and long-term impact of delayed vertical vein ligation using an adjustable vertical vein ligature on survival of patients with supracardiac TAPVC having moderate or severe pulmonary artery hypertension. The secondary objectives of the study were to: ii) examine whether the unligated vertical vein is serving as a temporary “pop-off” valve in the event of pulmonary hypertensive crises; iii) ascertain the timing to occlude the vertical vein; iv) evaluate the presence of iatrogenic kinking of left superior pulmonary vein and left brachiocephalic vein, if any and v) study the requirement of cardiac reoperations for residual shunts at the level of vertical vein or recurrent pulmonary venous obstruction.
This retrospective study conforms to the principles outlined in the declaration of Helsinki and was approved by the Institutional Ethics Committee. Patients were enrolled in the study protocol after obtaining informed written consent from patients/parents/guardians.
Patient selection criteria
This study evaluated short- and long-term outcomes after delayed ligation of the vertical vein in a consecutive series of patients undergoing repair of isolated supracardiac TAPVC.
off cardiopulmonary bypass and systolic PAP (SPAP) and mean LAP (MLAP) were measured. If SPAP ≥31 mmHg, MLAP ≥18mmHg, and peak systolic right-to-left ventricular pressure ratio >1.0, adjustable vertical vein ligation was performed. Otherwise vertical vein was directly ligated and those patients were excluded from the study.
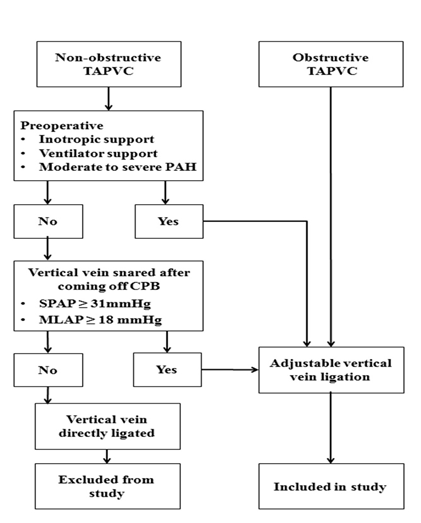
Figure 2: Schematic diagram showing the inclusion and exclusion criteria for selection of patients undergoing rechanneling of supracardiac totally anomalous venous connection (TAPVC) with or without vertical vein ligation and adjustable vertical vein ligation. PAH= pulmonary artery hypertension, SPAP=s systolic pulmonary artery pressure, MLAP= mean left atrial pressure
A 19-year (January 2000 to December 2019) retrospective review of medical records of 99 consecutive patients (62 males) undergoing rechanneling of supracardiac TAPVC with adjustable vertical vein ligation at AIIMS, New Delhi operated by a single surgeon (corresponding author) were studied. Inpatient and outpatient records were analysed to obtain demographic, operative, and perioperative features, follow-up echocardiographic computed tomographic (CT) angiographic studies, cardiac catheterization and clinical data.
Operative mortality was defined as patient death either prior to hospital discharge or within thirty days of the date of surgery according to the Congenital Heart Surgery Outcome measures endorsed by the Society of Thoracic Surgeons16.
Definitions
Criterions for pulmonary venous obstruction and indications of cardiac catheterization
Echocardiography was our principal diagnostic modality, and 60 of the 99 patients proceeded to operation with only echocardiographic data. The indications of preoperative cardiac catheterization were (1) anatomy that was unresolved by echocardiography, (2) characterization of the pulmonary venous obstruction, or (3) exclusion of major associated cardiac anomalies that required delineation or intervention.
Preoperative pulmonary venous drainage was considered obstructive if there was echocardiographic or angiographic data that indicated: (1) a significant gradient between the pulmonary veins and their point of drainage (flow acceleration >2 m/s by echocardiography or pressure gradient >4 mm Hg), (2) monophasic and continuous Doppler flow pattern in the individual pulmonary veins, the pulmonary venous confluence or the vertical vein, or (3) angiographically evident localized reduction in a single pulmonary vein diameter of 50% or more.
Pulmonary hypertension was defined as a right-to-left ventricular systolic pressure ratio of 0.6. According to SPAP, as measured by cardiac catheterization or on echocardiography on the basis of the velocity of tricuspid regurgitation, pulmonary hypertension was graded as follows: none (SPAP <18 mm Hg), mild (SPAP 19-30 mm Hg), moderate (SPAP 31-50 mm Hg), or severe (SPAP >50 mm Hg.) Isolated or simple TAPVC was diagnosed if the patient had TAPVC in association with a secundum atrial septal defect (ASD), a patent ductus arteriosus, or both. An operation was classified as an emergency if the patient was taken to the operating room within the first 24 hours after arrival at the hospital for hemodynamic or ventilatory compromise.
Low cardiac output syndrome in repaired TAPVC was diagnosed if the patient required inotropic support (dopamine at 4-10 µg/[kg/min]), dobutamine at 5-10 µg/[kg/min], epinephrine at 0.01-0.1 µg/[kg/min], milrinone at 50 µg/kg intravenous bolus followed by 0.375-0.75 µg/[kg/min]), either isolated or in combination in the operating room or in the intensive care unit, to maintain stable hemodynamics in the absence of residual structural lesions and mechanical external compression after correction of all electrolytes or blood gas abnormalities and after adjustment of the preload to its optimal value. Low-output syndrome was also diagnosed if there was an increasing requirement of the previously mentioned inotropes along with afterload reduction with sodium nitroprusside. Patients who received less than 4 µg/(kg/min) dopamine to increase renal perfusion were not considered to have low output syndrome.
Invasive monitoring to measure cardiac output directly (thermodilution catheter, PA pressure line, and thermistors) is cumbersome and hazardous in children and generally avoided in our setup, except in complex cases. We generally limit intracardiac monitoring to right atrial, LA, and PA pressure lines. Accordingly, under the definition of low output syndrome after repaired TAPVC, an integration of relevant clinical, laboratory, and bedside echocardiographic criteria was used. The criteria for diagnosis were as follows: cold extremities, absent pedal pulses, decreased toe temperature, reduced systolic pressure, impaired renal function and oliguria (<1.0 mL/[kg/hr]), metabolic acidosis, increased serum lactate levels (>2 mmol/L for >2 hours), low mixed venous oxygen saturation (<50%), and blunted sensorium in the absence of residual anastomotic or pulmonary venous obstruction.
Postoperative studies
All survivors (n=93) were examined and studied between January 2019 and December 2019, which was the closing interval of the study. Postoperative evaluation consisted of three monthly clinical examination, electrocardiogram, chest radiograph, echocardiography and computed-tomographic angiography. The functional class at follow-up was noted. A minimum of 12 months follow-up was mandatory for echocardiographic and angiocardiographic evaluation. For life table analysis, complete follow-up from the day of operation till the last follow-up was taken into consideration. Computed-tomographic angiography was performed on a third generation, 384 (2 x 192) slice, dual source CT scanner and multiplanar reformatted images and volume rendered images (SOMATOM FORCE, Siemens, Germany) were reconstructed and analysed.
Techniques of Computerised-tomographic Angiography
All scans were performed on a third generation, 384 (2 x 192) slice, dual source CT scanner (SOMATOM FORCE, Siemens, Germany). It has a rotation time of up to 0.25 seconds with a temporal resolution of up to 66 milliseconds and spatial resolution of 0.24 mm.
No form of heart rate control was required. Retrospective ECG-gated CT angiography examination was performed after injection of non-ionic iodinated contrast (1.0 to 1.5 mL/Kg body weight) was administered via peripheral intravenous line at flow rates varying from 1.0 – 4.5 mL/s followed by a saline chaser injected at the same flow rate. A prospectively gated flash mode acquisition at a pitch of 3.2 (table feed 737 mm s−1), and using a tube voltage of 80 kVp with automated tube current modulation was also performed. A “manual” bolus tracking method was used with acquisition manually triggered when optimal contrast opacification within the pulmonary vessels was perceived on the monitoring sequence. Automated tube voltage selection and automated tube current modulation based on body habitus (CARE kV and CARE Dose4D, Siemens Healthcare) were enabled.
Slices were reconstructed of 0.6-mm section thickness and increment of 0.4 mm, using a medium sharp kernel (Bv40), with a model based iterative reconstruction strength level 3 (ADMIRE; Siemens Healthcare). Multiplanar reformatted images and volume rendered images were reconstructed and analysed.
Operative and Postoperative Management
The surgical techniques, intra- and postoperative management protocols were uniform throughout the study period. No patients underwent deep hypothermic circulatory arrest in the study group. Forty-nine (49.4%) patients required emergency operation for hemodynamic or respiratory compromise.
All patients underwent rechanneling of TAPVC with left atrial augmentation, atrial septal fenestration, and adjustable vertical vein ligation under moderately hypothermic CPB and St. Thomas (II) based (4:1) cold blood cardioplegia. Both continuous and modified ultrafiltration was used in all patients to reduce total body water and to remove inflammatory mediators from the circulation. The technical details of the surgical steps including adjustable vertical vein ligation have been enumerated in our previous two publications as well as in the video presentation (Figures 3A-3D, Video presentation) [14-15] We proceeded to keep the vertical vein unligated if the PA pressure remained elevated (systemic or suprasystemic) with a peak systolic right-to-left ventricular pressure ratio ≥ 1.0 after coming off CPB and administration of protamine on snaring the vertical vein. Left atrial and PA pressures were monitored continuously during the operation. After the operation patients were sedated and paralyzed during the first 24 to 48 hours. Pulmonary arterial hypertension was treated with hyperventilation, sedation, phenoxybenzamine, sildenafil citrate and inhaled nitric oxide (10-15 ppm) in varying combination.
After weaning from bypass, upon snaring the vertical vein, the MLAP increased between 18 and 21 mmHg accompanied by an acute increase in systolic PAP to greater than 50 mmHg in 82 (82.8%) patients. Loosening of the vertical vein resulted in a decrease of pressure to a ratio of 0.6 and decrease of the MLAP to 11 mmHg with a range between 10-11mmHg in all patients. This was associated with a significant increase in mean arterial blood pressure and stable hemodynamics. The PA pressure in the remaining 17 patients was between 31-50 mmHg. The vertical vein was left open on an adjustable vertical vein ligature in all patients.
The sternum was left open in 11 (11.1%) patients. Delayed sternal closure was done 24 to 48 hours after hemodynamic stability was achieved.
Median duration of inotrope requirement was 8 days (range 6-19 days). Median duration of ventilation was 4 days (range 1-20 days). Thirty-nine (39.3%) patients received total parenteral nutrition commencing after 48 hours of ventilation. After the operation, patients were weaned from digoxin, diuretics, phenoxybenzamine and angiotensin-converting enzyme-inhibitors at varying intervals.
The mean CPB time was 56.5±11.9 minutes (range 35-120 minutes), and the mean aortic cross-clamp time was 26.2±8.3 minutes (range 17-70 minutes). Left ventricular assist devices and extracorporeal membrane oxygenation (ECMO) were not used for any patient in this study group.
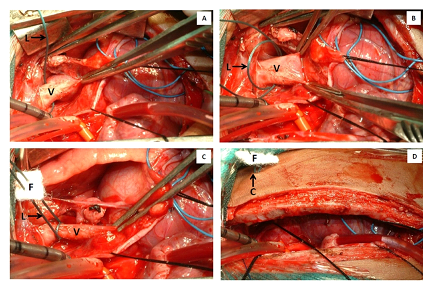
Figures 3A-3D: Surgical photograph of an adjustable vertical vein ligature (L) showing the sick suture doubly looped around the vertical vein (V) and passed through a polytetrafluoroethylene felt (F). Subsequently, the sutures are passed through the second left intercostal, skin and another polytetrafluoroethylene felt (F) in a straight lie. Two clips (C) are applied individually over each silk suture at the exit point under the subcutaneous tissue. An additional clip is applied over the polytetrafluoroethylene felt which act as a marker. C= Ligaclips, F= polytetrafluoroethylene felt, L= vertical vein ligature, V= vertical vein
Statistical Analysis
Statistical analysis was performed using STATA 14.0 Software (College Station, Texas, USA). Interval related data were expressed as mean ± standard deviation (SD) or median (minimum-maximum) and categorical variables were expressed as percentages. The survival probability with 95% confidence intervals was reported at various time intervals with the Kaplan-Meier technique (Figure 4). The p value of <0.05 was considered as statistically significant.
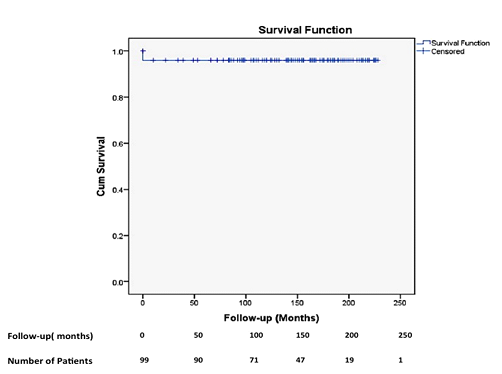
Figure 4: Actuarial survival curve of patients (n=99) undergoing adjustable vertical vein ligation and left atrial augmentation for obstructive supracardiac totally anomalous pulmonary venous connection.
Original cohort
Patients’ age at operation ranged from 1 day to 25 years (mean 24.8±55.3 months, median 4 months). Thirty-five (35.2%) patients were younger than 1 month, 10 (10.1%) were between 6 and 12 months, and 24 (24.2%) were between 12 months and 25 years. Body weight ranged from 1.8 kg to 47 kg (mean 6.3±6.2 kg, median 4 kg). Most patients in this study group were small for age and 60% weighed less than 50th percentile of predicted weight for Indian neonates and infants.
Two-dimensional colour Doppler echocardiography revealed obstructive TAPVC in 49 (49.4%) patients. The level of obstruction was at the insertion site of the vertical vein into the brachiocephalic vein in 25 patients, at the level of left bronchus and left pulmonary artery in 15 patients, and due to restrictive atrial septal defect (ASD) in 9 patients. (Definitions- Electronic)
Ten (10.1%) patients underwent preoperative balloon dilatation of the vertical vein and 9 (9.1%) patients underwent balloon atrial septostomy. The ductus arteriosus was patent in 64 (64.6%) patients. Nineteen (19.2%) patients required preoperative mechanical ventilation, and 32 (32.3%) patients required inotropic support for hemodynamic instability. Their demographic and clinical profiles are depicted in tables 1 and 2.
Cardiac catheterization and angiocardiography were performed in the initial 19 (19.2%) patients in whom an accurate anatomical pattern was unresolved by echocardiography and in 20 (20.2%) patients to evaluate the degree of pulmonary hypertension. Since 2009, computed-tomographic (CT) angiography is used as a routine to delineate the anatomic details in doubtful cases to establish the diagnosis and has almost replaced angiocardiography.
Short-term outcomes
There were 5 (5.0%) operative deaths due to persistent PAH and low cardiac output syndrome (LCOS) (n=2), refractory ventricular arrhythmias (n=1), massive pulmonary haemorrhage (n=1), and sepsis (n=1) during the early period of our study (2002- 2010). All survivors exhibited an entirely satisfactory primary repair (echocardiographically, showing a large unrestricted anastomosis, as large as or larger than mitral valve orifice area, with no gradient between the pulmonary venous confluence and LA and non-turbulent biphasic pulmonary venous flow at <1.2 m/sec. Ten (10.1%) patients demonstrated subtle echocardiographic changes with a large, unrestrictive anastomosis with no gradient between the common pulmonary venous chamber and LA and biphasic or mainly biphasic pulmonary venous flow with a velocity of 1.2 to 1.6 m/sec.
Despite having an unligated vertical vein, 13 (13.1%) patients with obstructive TAPVC with PAH undergoing emergency surgical intervention for hemodynamic or respiratory compromise exhibited suprasystemic PAP and unstable postoperative hemodynamics. Among them, the sternum had to be left open in 11 patients. Delayed sternal closure was done in 24- 48 hours after achieving stable hemodynamics. These patients were mechanically ventilated with an inspired oxygen fraction of 0.8 and 20 ppm nitric oxide and were administered pulmonary vasodilators (sodium nitroprusside 0.5µg/Kg/min, phenoxybenzamine 0.5 µg/kg at 8-hour intervals) for 15-20 days. Intraoperative transesophageal echocardiography at the time of sternal closure continued to demonstrate shunting from the common pulmonary venous chamber (CPVC) to the brachiocephalic vein and attempted snaring of the vertical vein resulted in rise of PAP to systemic and suprasystemic levels in all of them. Despite all attempts, 2(2%) patients died of pulmonary hypertensive episodes.
Serial echocardiography during these episodes demonstrated shunting from the CPVC to the brachiocephalic and right-to-left shunting across the fenestrated atrial septal patch, clearly documenting their roles as a temporary vent (Figures 5A, 5B, 6A-6D).
Postoperatively, all patients underwent daily echocardiographic assessment of biventricular function and flow through the vertical vein. Serial postoperative echocardiograms showed unobstructed pulmonary venous return into LA with a distended vertical vein (Figures 5A, 5B).
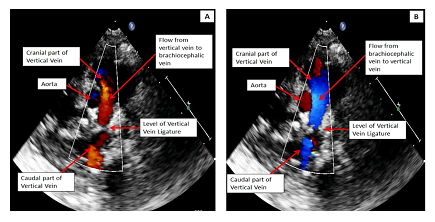
Figures 5A, 5B: Postoperative transthoracic two-dimensional echocardiogram: 2A: Day 1 postoperative with color flow patterns of venous flow in the unligated vertical vein showing shunting from the left atrium to the brachiocephalic vein via the patent vertical vein; 2B: Demonstration of change of the shunting patterns on the 10th postoperative day on the same patient from the brachiocephalic vein to the left atrium via the vertical vein.
Although all survivors were extubated within 24 to 96 hours with stable hemodynamics, 35 (35.35%) patients continued to have tachypnoea and biventricular failure during the first two weeks. Postoperatively, serial echocardiography demonstrated reversal of flow from the brachiocephalic vein to LA in all patients. The vertical vein was interrupted in all patients using the adjustable vertical vein ligature when there was phasic reversal of flow from the brachiocephalic vein to the LA on color Doppler (Figures 5A, 5B, 6A-6D).

Figures 6A-6D: Postoperative transthoracic two-dimensional echocardiogram showing the newly constructed interatrial septal patch with left atrial augmentation and atrial septal fenestration (arrow). Doppler flow shows there is complete interruption of blood flow through the vertical vein after adjustable vertical vein ligation. (AoV= Aortic valve, CC= Common pulmonary venous chamber, LA Aug= Augmented left atrium, PA= Pulmonary artery, RA= Right atrium, VV= Vertical vein).
At this point, we decided to tighten the adjustable ligature in increments. Tightening was achieved by placing additional clips outside between the polytetrafluoroethylene pledget and the previous clip, while monitoring the LA and PA pressure and arterial blood gases. Echocardiographic assessment was performed to assess the ventricular function and the degree of tightening was assessed by reduction of left-to-right shunt through the vertical vein. All ligatures were tightened gradually over a period of 24 to 96 hours, maintaining stable hemodynamics with PA pressure at subsystemic levels and normal blood gases.
Long-term outcomes
There were 2 (2.0%) late deaths 80 and 94 months after surgery due to ventricular arrhythmia (n=1) and pulmonary sepsis (n=1) respectively. Follow-up was 100% complete (1-228 months) and yielded 1695.7 patient-years of data. At a mean follow-up of 218.8 (sE± 209.9) months, the actuarial survival was 93.7 (SE±0.02%; 95% CI: 86.5, 97.1; Figure 4). All survivors were in New York Heart Association I or II at their last follow-up. There were no reoperations during this period.
At a mean follow-up of 218.8 (±SE, 209.9) months, serial 2-dimensional echocardiography did not reveal any evidence of pulmonary venous obstruction, or residual flow through the ligated vertical vein (Figures 5A, 5B, 6A-6D).
Angiographically, none of the survivors demonstrated any flow through the vertical vein and none had evidence of restenosis of the common pulmonary venous chamber-LA anastomosis. There was marked increase in the volume of the left atrium and there was no distortion of the left superior pulmonary vein and left brachiocephalic vein on any patient (Figures 7A-7D, 8A-8D, 9A-9C, 10A-10D)
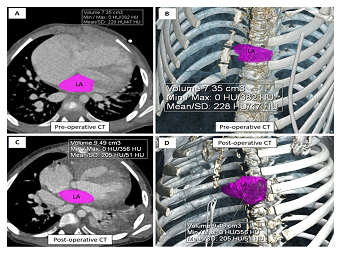
Figures 7A-7D: Axial images and three-dimensional volume rendered computed tomographic image in the oblique coronal projections (A and B; preoperative) and (C and D; postoperative) showing marked increase in the volume of the left atrium from 7.3 ml (preoperative) to 9.3 ml (postoperative) due to left atrial augmentation and changes in the loading condition of the left heart following common pulmonary venous chamber to left atrial anastomosis. (LA=left atrium)

Figures 8A-8D: Postoperative preligation, three-dimensional volume rendered coronal computerized tomographic image- A) anterior, B) posterior view showing unligated vertical vein and the wide unrestricted anastomosis between the common pulmonary venous chamber and left atrial appendage, C) anterolateral, & D) posterior projection showing the cranial part of the ligated vertical vein and all pulmonary veins draining into the common pulmonary venous chamber which has been anastomosed to the left atrial appendage (CC= Common pulmonary venous chamber, DTA= Descending thoracic aorta, LAA= Left atrial appendage, LSPV= Left superior pulmonary vein, RIPV= Right inferior pulmonary vein, RSVC= Right superior vena cava, RSPV= Right superior pulmonary vein, SVC= Superior vena cava).

Figures 9A-9C: Postoperative postligation, three-dimensional volume rendered computed tomographic images in the coronal (A), left anterior oblique projection (B) and the postero-anterior projection (C) showing the cranial part of the ligated vertical vein and the wide unrestricted anastomosis between the common pulmonary venous chamber and left atrial appendage. All pulmonary veins are draining into the common pulmonary venous chamber which has been anastomosed to the left atrial appendage (CC= Common pulmonary venous chamber, DTA= Descending thoracic aorta, LAA= Left atrial appendage, SVC= Superior vena cava).
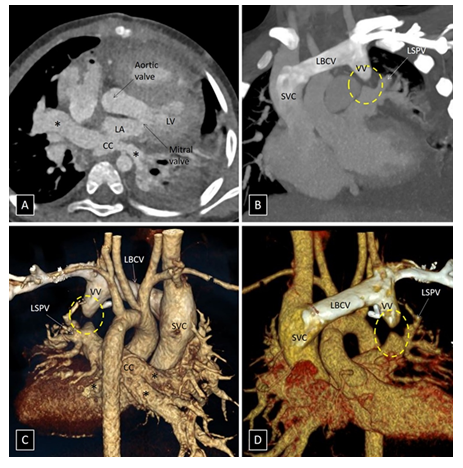
Figures 10A-10D: Postoperative postligation, axial image (A), coronal image, three-dimensional volume rendered computed tomographic image in the postero-anterior projection (C) and antero-posterior projection (D) showing the cranial part of the ligated vertical vein and the wide unrestricted anastomosis between the common pulmonary venous chamber and left atrial appendage. All pulmonary veins (*) are draining into the common pulmonary venous chamber which has been anastomosed to the left atrial appendage. (CC= Common pulmonary venous chamber, LA= Left atrium, LV=left ventricle, LBCV= Left brachiocephalic vein, LSPV= Left superior pulmonary vein, SVC= Superior vena cava; VV= Vertical vein).
The medical literature is rife with examples of therapies that seemed likely to be beneficial, but were in fact either pointless or harmful. As far as we could establish, there have been limited studies addressing the usefulness of vertical vein interruption at the time of TAPVC repair and the fate of unligated vertical vein following repair of TAPVC. There remain several unresolved queries in the medical and surgical management of TAPVC and there is no fool proof formula in the published literature to decide the optimal surgical management for a given patient.
Our 99-patient cohort is perhaps the largest so far to be evaluated for selective vertical vein patency, adjustable vertical vein ligature, LA augmentation and atrial septal fenestration on the postoperative outcomes of repaired TAPVC The age distribution was heterogenous with 35 (35.2%) patients being ≤1 month, and 24 (24.2%) were between 12 months and 25 years. The patient’s socioeconomic profiles and lack of healthcare access led to their referrals for surgery at older ages.
In our earlier publications, we demonstrated that late referral and late presentation lead to the development of severe PAH, malnutrition and ultimately cardiac cachexia. These factors predispose them to pulmonary infection, sepsis, postoperative pulmonary hemorrhage, and unfavourable reactions to bypass related stresses4. Despite aggressive perioperative management, we reported worse outcomes in whom conventional strategy of routine ligation of a discernible ascending or descending vertical vein was performed [14].
One important finding of our investigation was the occurrence of post bypass suprasystemic PA pressure due to late presentation, cardiac cachexia and cardiac pathology.
Our second finding is the occurrence of suprasystemic PA pressure and unstable hemodynamics upon snaring the vertical vein after weaning from bypass. Release of the snare resulted in improved postoperative haemodynamics, early weaning from ventilatory support, and survival. In the absence of anastomotic stricture, this undesirable effect can be explained by impaired unloading of the pulmonary venous chamber due to non-compliant left-sided cardiac chambers.
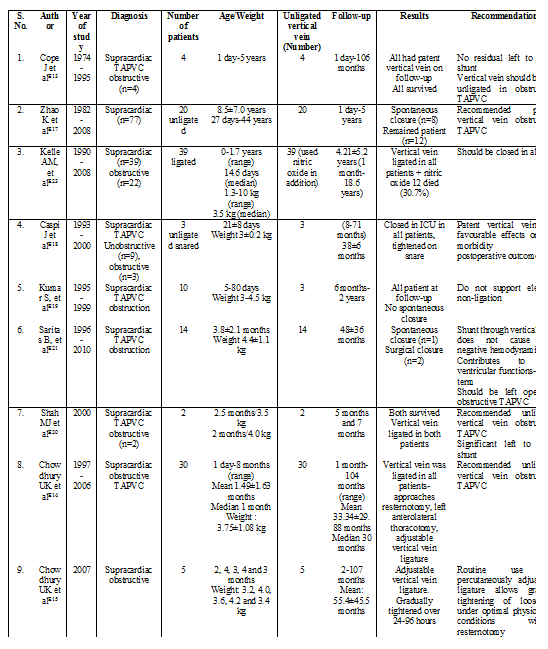
The benefits of an unligated vertical vein over the traditional concept of routine vertical vein ligation at the time of TAPVC repair remains debatable [16-23]. As yet, there are no universally accepted criterions for selection of patients in whom it is advantageous to maintain the patency of the vertical vein.
A number of studies with small cohort of patients have been published by various investigators with conflicting results (Table 3) [16-23]. Proponents of leaving the vertical vein unligated presume that it helps to tide over postoperative pulmonary hypertensive crisis [13,18,20,21]. Furthermore, some investigators have shown that the flow through vertical vein ceases as time passes and there is no requirement for further intervention13,17,21. However, there are few reports of persistent left-to-right shunt through the vertical vein leading to cardiac failure, which required reoperation for ligation of vertical vein [17,18,20]
Advocates of vertical vein ligation even in patients with moderate or severe pulmonary hypertension rely on advanced postoperative intensive care management utilizing nitric oxide therapy, ventilator management strategies and occasionally on ECMO [18,23,24].
Recurrent episodes of pulmonary hypertensive crises, rapid development of pulmonary arterial and venous medial hypertrophy, and a small noncompliant LA and LV have been variously implicated as the causative factors for the LCOS [1-4,14,25-32].
In 2007, we demonstrated that acute vertical vein ligation resulted in elevated LA pressure and impaired LV function suggesting that for a period of time the small, poorly compliant LV of the patient with obstructive TAPVC was unable to maintain adequate cardiac output [14].
The unligated vein group in our previous study demonstrated statistically significant decreased in-hospital mortality (p=0.04), decreased pulmonary hypertensive crises (p<0.001), shortened intensive care and hospital stay (p<0.001) and superior postoperative hemodynamics (p<0.001). Logistic regression analysis demonstrated 3.28 times (95% CI: 108-9.99) increased risk of death after vertical vein ligation [14].
Contrary to the reports by Cope and colleagues in which patent vertical vein atrophied, 11 of 23 survivors in our previous investigation had symptoms of a large left-to-right shunt through the unligated vertical vein requiring delayed interruption. The vertical vein was ligated through resternotomy in 4 patients, left anterolateral thoracotomy in 2 cases and adjustable vertical vein ligature in 5 patients [13,14]. Due to non-availability of Amplatzer vascular plug, these six patients underwent surgical ligation of the vertical vein. Although delayed closure of the vertical vein was successful in all cases it was attended by extremely high PAP in six patients and proved a difficult postoperative challenge. These findings were suggestive of a relatively small, non-compliant dysfunctional left-sided chambers or of disease-related or CPB-related pulmonary vasoreactivity [14].
There are varying reports on left heart volume characteristics in obstructive TAPVC from normal findings to the conclusion that left-sided chambers are smaller than normal and the LA lacks both normal compliance and reservoir function [5-11]. Such chamber abnormalities have been attributed to large left-to-right shunt causing reduced atrial filling and decreased LV relaxation secondary to elevated right ventricular diastolic pressure or volume [5-11]. Published literature does not address the percentage of patients with obstructive TAPVC who have structurally smaller left-sided chambers.
In order to allow the left heart to adapt and maintain adequate cardiac output, we have used an oversized Dacron patch for interatrial septation, deviating the same towards the enlarged right atrium and have incorporated part of the vertical vein to achieve structural alignment and augmentation of the LA cavity (Figures 7A-7D) [14]. The concept of enlarging the LA is almost similar to that described by Cooley and colleagues except that in our patients, we achieved it by excising the floor of the fossa ovalis and utilizing an oversized Dacron patch graft to close the ASD and enlarge the LA [33].
Corno and colleagues described the two-patch technique of LA enlargement34. Subsequently, several investigators have demonstrated increased incidence of supraventricular arrhythmias due to the use of a transverse right atrial incision and division of the supraventricular crest. We have not used this technique. There is no valid argument for or against the use of Dacron patch or pericardial patch. It may be argued that fenestration in the synthetic patch may be appropriately sized at the primary operation with minimal chances of over or undersizing. There were no residual shunts through the fenestration on any surviving patient on long-term follow-up.
The driving forces behind selection of patients whose vertical vein was kept patent after surgery were to reduce the PAP in the perioperative period, postoperative pulmonary hypertensive crises and mortality (Figure 2). We aimed to achieve this by leaving the vertical vein unligated so that it may function as a temporary venous reservoir for pulmonary venous blood, volume unloading the small non-compliant left-sided cardiac chambers until they are able to grow and adapt to the requisite flow demands. Secondly, the unligated vertical vein could serve as a temporary “pop-off” valve in the event of pulmonary hypertensive crises and thereafter the same may be subjected to a gradual process of occlusion15. Finally, despite late presentation and long standing pulmonary hypertension, we have been successful in occluding the patent vertical vein within 72 to 96 hours. (Figures 5A, 5B, 6A-6D).
The etiopathogenesis of postoperative pulmonary hypertensive crises in obstructive TAPVC may be multifactorial [25-32]. Although the pulmonary veins/capillaries do not have any valves, there are variable reactive pulmonary arteriolar changes due to the disease process and any rise in LAP will lead to pulmonary hypertensive crisis. The postoperative course targets management of these issues and occasionally ECMO is necessary while the pulmonary vascular bed recovers and LV compliance improves [14,15,24]. The time course of this adjustment is variable. It is conjectured that there is a feedback loop whereby acute elevation of LAP results in excessive pulmonary arteriolar constriction with disproportionate pulmonary hypertensive response that further exacerbates the low cardiac output state caused by a poorly compliant LV [14].
Atrial septal fenestration in patients undergoing rechanneling of TAPVC is controversial. In this study, we performed atrial septal fenestration to permit “spill over” in the setting of postoperative RV dysfunction in patients with both obstructive and non-obstructive supracardiac TAPVC with PAH. During episodes of pulmonary hypertensive crises with limited RV output, and an elevated central venous pressure (CVP), a fenestrated atrial septal patch permitted right-to-left shunting, increasing left ventricular preload and cardiac output, albeit at the expense of some degree of systemic desaturation (Figures 5A, 5B, 6A-6D). It is noteworthy that none of the survivors exhibited any shunting in the late postoperative period and none required any interventional closure of the fenestration. Thus, the unligated vertical vein, in conjunction with a calibrated atrial septal fenestration, resulted in equalization of LAP and CVP during episodes of pulmonary hypertensive crisis, and was the automatic choice to avert a dismal outcome in the perioperative period. Our protocol is to institute mechanical circulatory assistance, if the cardiac output cannot be sustained by the currently available medical and surgical treatment. We have not used ECMO on any of our patients in this study group.

Table 1: Demographic, operative and postoperative details and the study group (n=99)

Table 2: Demographic, operative and postoperative details of the study group (Obstructive vs. non-obstructive: n=99)
TAPVC=Totally anomalous pulmonary venous connection
Table 3: Summary of the published investigations documenting the fate of a patent vertical vein in the setting of obstructive supracardiac totally anomalous pulmonary venous connection (TAPVC)
Based on the literature and reasoning cited above, we decided to device a method to avail the benefits of an unligated vertical vein in patients with obstructive TAPVC with post-bypass systemic or suprasystemic PAH, at the same time avoid the nuances of residual left-to-right shunt in the late follow-up when the period of acute crisis is over. The technique and the initial observations following adjustable ligature of the vertical vein was published in 2007 [15].
Thus, the advantages of adjustable vertical vein ligature were:
The drawback of this technique may be the inability to loosen the ligature in the event of hemodynamic decompensation. All ligatures in this cohort were tightened gradually in increments over a period of 24-96 hours maintaining stable hemodynamics.
A persistent left-to-right shunt with bi-ventricular failure through an unligated vertical vein does not necessarily relegate a patient to a second-stage operation and does not warrant modification of our selection criteria for the unligated vertical vein. They may be candidates for adjustable vertical vein ligature or transcatheter vertical vein closure [15-35].
An initial concern about the technique was the possibility of iatrogenic distortion of the left superior pulmonary vein and left brachiocephalic vein. In order to address these concerns, we have threaded the loop ligature through a polytetrafluoroethylene felt and secured it to adventitia of the vertical vein, thus preventing its displacement, and brought the arms of the silk suture through the second left intercostal space, away from the sternotomy incision, perpendicular to the vertical vein, ensuring a vertical straight lie, and avoiding distortion or occlusion of the left upper pulmonary and brachiocephalic veins (Figures 3A-3D). Postoperatively, we performed computed-tomographic angiography on all survivors at follow-up and discovered no untoward findings (Figures 8A-8D, 9A-9C, 10A-10D).

Figure Legends of Video Presentation
A video presentation of the surgical techniques of adjustable vertical vein ligation and left atrial augmentation in obstructive supracardiac totally anomalous pulmonary venous connection (UKC’s modification).
Study limitations
This study has several limitations. In as much as this is a single-surgeon, single-center study, the results may not necessarily be applicable to all centers. Given its retrospective design, there may have been unmeasured confounding factors that influence the observed outcomes. The study institution likely has a referral bias for high-risk patients with complex congenital heart diseases, prematurity, late presentation, and referral from outside the geographical area.
We conclude that in obstructive and non-obstructive supracardiac TAPVC, postoperative pulmonary hypertension is common, and augmenting left atrial compliance by atrioplasty is perhaps useful. By leaving a pop-off, either an atrial septal fenestration, and/or the vertical vein in the immediate postoperative period, can be helpful to maintain cardiac output when there is an expected pulmonary hypertensive crisis. One or both of these pop-offs will at some point become redundant, with shunting only left-to-right, which slowly but surely, will lead to volume overload, and they will need to be addressed. In a setting where transcatheter solutions (plugging a vertical vein or ASD fenestration with a device) are not available or prohibitively expensive, percutaneous adjustable vertical vein ligature is a useful adjunct.
It allows gradual tightening of the ligature under optimal physiologic conditions without reoperation and without causing any distortion of the left superior pulmonary vein and left brachiocephalic vein. Knowledge of this approach should contribute to the armamentarium of cardiac surgeon faced with obstructive TAPVC with pulmonary arterial hypertension.
Statement of human rights/ethical approval
The authors assert that all procedures contributing to this study comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki declaration of 1975, as revised in 2008 and has been approved by the Institutional Research Committee.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of the article.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
