AUCTORES
Globalize your Research
case report
*Corresponding Author: Ranasinghe L, Professor and Director of Emergency Medicine Clerkship, California Northstate University College of Medicine (CNUCOM), Elk Grove, California, USA.
Citation: Dang R, Eggleton J , Habibe M, Alhadi S, Kessler M. et all (2022) A Rare Case of Mastoiditis in an Adult Patient. J. Archives of Medical Case Reports and Case Study, 5(5); DOI:10.31579/2692-9392/119
Copyright: © 2022 Ranasinghe L, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 04 March 2022 | Accepted: 15 April 2022 | Published: 22 April 2022
Keywords: mastoiditis; pediatric
Mastoiditis is more commonly seen and easily recognized in children. However, adults are more likely to present with complications requiring emergency medical treatment. One of the challenges in the management of mastoiditis is recognizing symptoms and beginning treatment with antibiotics early to prevent progression of disease and potential surgical management. This case report details an unusual case of a 41-year-old woman whose indolent symptoms went unrecognized for three weeks before presenting to the emergency department with unilateral ear pain and hearing loss. Imaging revealed coalescing mastoiditis with erosion of the medial cortex into the jugular foramen and enhancement suggestive of meningitis. This report can assist practitioners in recognizing and managing mastoiditis and its associated complications in the emergency setting.
Background
Mastoiditis is an infection or inflammation of the mastoid air cells that most often results from the contiguous spread and progression of an acute or chronic otitis media (OM) infection [1]. Before diagnosis of mastoiditis, patients tend to have more than one visit to physicians with reports of unilateral otalgia, swelling, erythema over the mastoid bone, fever, and hearing loss. There is a risk of progression into intratemporal and intracranial complications that may be deadly such as prolonged latent mastoiditis, intracranial abscesses, meningitis, sigmoid sinus thrombosis, or otogenic hydrocephalus if not treated promptly [2,3]. Otitis media is a common childhood disorder with a peak incidence between 6 months and 2 years of age [4,5]; however the average age of patients presenting to the emergency room with complications of OM is 37 years of age. [6] While the incidence of mastoiditis overall has declined significantly with the routine use of antibiotics for OM, some studies have shown that the incidence of mastoiditis in adults has remained consistent [2,7]. This report is significant, as most of the literature on this topic is based on pediatric cases. This case report details an unusual case of a 41 year old woman on initial presentation to the emergency room with minimal symptoms which ultimately proved to be advanced mastoiditis complicated by osteomyelitis of the mastoid bone.
The patient was a forty-one year old female with a past medical history significant for asthma, gastriculcers, endometriosis, and more than ten packyears of smoking history, presenting to the emergency department complaining of left ear pain for three weeks. The pain was rated a constant 10/10 on the pain scale and described as “dull with aching” in quality. This pain was reported to be minimal to start, but progressed gradually over three weeks with similar discomfort radiating up the left jaw. The pain was initially responsive with use of over-the-counter pain medications, but she eventually presented to the emergency department when they no longer relieved or controlled the pain. Associated with the ear pain was hearing loss of the left ear that progressively increased in severity over three weeks. Other associated symptoms included yellow drainage from the left ear, which self-resolved one week prior to her initial presentation to the emergency department, left-sided neck swelling, and mild nasal congestion. The patient denied right ear pain, changes in right-sided hearing, fever, nausea, vomiting, headache, or dizziness. She did not seek medical attention prior to her visit to the emergency department. She had no further reported chronic medical conditions and she took no medications regularly at home. The rest of the review of systems was unremarkable.
The patient’s vital signs upon arrival to the department indicated that she was afebrile at 36.6° Celsius, normal tensive with a BP 132/88 mmHg, heart rate of 99 bpm, respiration rate of 16 breaths per minute, and saturating at an SPO2 of 100% on room air.
Upon physical exam, the patient was a well-appearing female in mild distress due to her left ear pain. There was tenderness, slight swelling, and erythema located behind the patient’s left ear. The tragus and auricleof the left ear were extremely tender.There was also significant tenderness at the left mastoid.
Using the otoscope, the ear canal was noted to have mild swelling with a normal-appearing ear drum, with minimalerythema of the external auditorymeatus. There were no abnormalities seen on the physical exam of the right ear or the throat. There was no significant neck swelling. Patient had a regular rate and rhythm with cardiac auscultation. Lungs were clear to auscultation without labored breathing. Patient had normalspeech with baseline movement of all four extremities.
During ENT consultation, the left tympanic membrane was dull with signs of middle ear effusion visualized. The left pinna was displaced forward with marked tenderness along the mastoid bone. There was moderateedema of the extra-auditory canal.Sound lateralized to the left ear with Weber testing.
As part of the emergency medicine workup, the following labs were ordered: CBC, CMP, lactate, b-HCG. The CBC revealed leukocytosis with 19,000 cells/mcL and a high neutrophil percentage of 78.1%. The remaining lab values were non pertinent to management or diagnosis. While in the ED, the patient received the following as part of management: Unasyn 3g x1, Vancomycin 1250mg x1, Norco 5mg/325mg x1, Morphine 6mg x 1, Zofran 4mg x 1, Ibuprofen 600mg x1. The case was discussed with the inpatient medicine team and the ENT surgical team. Patient was admitted to the inpatient team for intravenous antibiotics and surgical intervention. Admitting diagnoses included abscess, encephalitis, meningitis, and leftmastoiditis.
Blood cultures and ear cultures were collected. Patient’s wound indicated 1+ growth of streptococcus pneumoniae. No strict anaerobes were isolated.
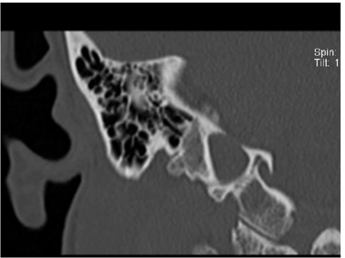
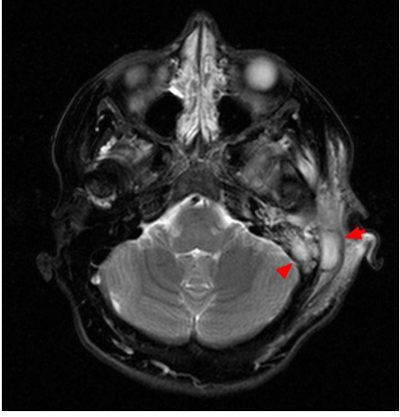
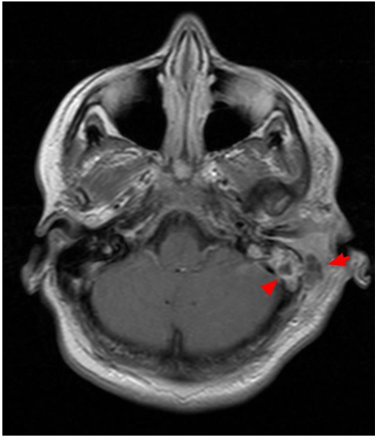
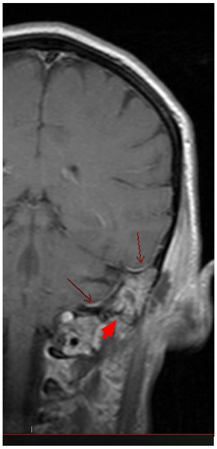
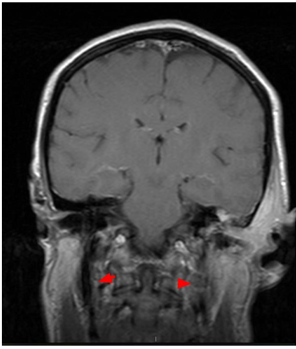
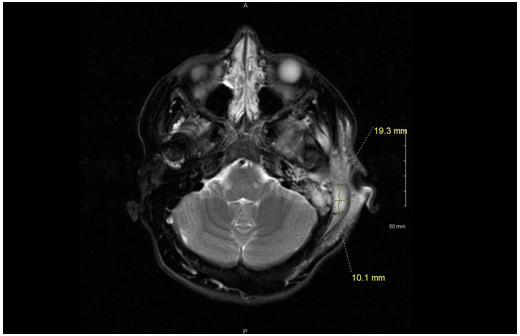
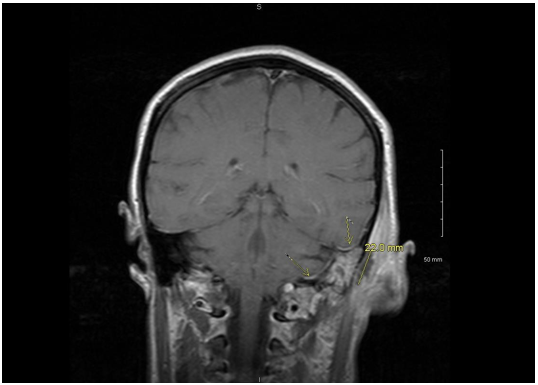
A noncontrast CT scan of the temporal bones and an MRI of the brain with and withoutcontrast were also orderedin the ED. The CT scan showed extensive periauricular soft tissue swelling and absorption of several septae of the mastoid air cells with erosive changes of the medial wall indicative of coalescent mastoiditis and concern for intracranial extension. Additionally, fluid could also be seen within the middle ear cavity; however, the ossicles remained intact. The contralateral ear and mastoid air cells were normal. On the MRI, a 1.9 x 1.0 x 2.2 cm fluid collection was seen in the periauricular tissues demonstrating restricted diffusion and peripheral enhancement, compatible with an abscess. Fluid signal and enhancement of the mastoid air cells, as well as septae absorption and medial cortical wall erosion, again confirmed the diagnosis of coalescent mastoiditis.
Intracranial extension of the infection was confirmed with thickening and enhancement of the meninges and possible diffusion restriction along the outer cortex of the adjacent cerebellar hemisphere. No definitive flow void was seen in the distal sigmoid sinus and jugular vein raising concern for venous compression with possible thrombus. Images with captions/descriptions included at the end of this publication.
During her first twelve hours of admission on antibiotics, the patient reported feeling considerably better. Dexamethasone sodium phosphate 4mg/mL 1mL q8h x 3, Piperacillin/Tazobactam 4.5g q6h IV, and Ondansetron 2mg/mL 2mL q6h prn nausea/vomiting were added to the patient’s medications. In preparation for surgical intervention with ENT in the morning, she was kept NPO. There were no further documented changes in condition throughout the night.
After evaluation of the patient and imaging, ENT deemed that the patient needed to undergo a tympanomastoidectomy. The CT and MRI imaging were indicative of coalescent mastoiditis with abscess formation overlying the mastoid bone, extending to the jugular bulb. Erosion of the tegmen overlying middle fossa, as well as evidence of meningitis with significant inflammation of the meningeal of the middle fossa, was reported. Additionally, there was soft tissue opacification of the middle ear cavity, as well as multiple entire left mastoid air cells. Patient was presented with all treatment options, with all the risks, benefits, and possible outcomes discussed. She understood and agreed to follow through with the operative route.
The operative procedures performed include: left tympanomastoidectomy with facial nerve monitoring using NIM nerve monitor and left myringotomy with tube placement. The operation was successfully performed with no complications and minimal blood loss (>20mL). During the procedure, evidence of a large abscess pocket overlying the mastoid bone extending over the temporalis fascia were noted. There was also evidence of cortical erosion of the mastoid, approximately 3 cm above the tip of the mastoid, and tegmen erosion that overlined the middle fossa of the sigmoid portion of the jugular bulb with total exposure. Additionally, some tissue granulation and mucopurulent fluid were noted throughout the mastoid air cell, as well as thickened granulated and polyploid tissue within the middle ear cavity with mucopurulent fluid, dehiscence and exposure of the meninges of the middle fossa. The surgical site was appropriately closed and a Penrose drain was placed for drainage purposes. The middle ear cavity was infused with ofloxacin through the myringotomy tube and an Otowick was then placed overlying the Gelfoam and was expanded with ofloxacin drops. The patient was then awakened, extubated safely, and transferred to the postanesthesia care unit in stable condition, breathing unassisted. The patient was sent to the post-anesthesia care unit after completion of previously noted procedures. Pain postoperatively was manageable. She was continued on broad spectrum IV antibiotics, including Vancomycin.
Outcome and Follow Up
After a five-day hospital course and an extensive work-up, the patient was found to be safe for discharge home on the fifth and final day. The patient’s last obtainable vital signs at the time of discharge indicated the following: afebrile with a body temperature of 37.0 degrees Celsius, pulse rate of 60, blood pressure at 104/76, and SPO2 at 100% on room air. She also reported a pain level that was improved from previous assessments at 5/10 on the pain scale. During the patient’s final physical examination, the Penrose drain was removed. This physical exam was notable for decreased hearing in the left ear. Otherwise, there were no focal strength deficits or sensory deficits found, Kernig’s sign was negative, and the patient's neck had a completely normal range of motion.
The patient was prescribed a fourteen-day course of clindamycin, 400 mg to be taken orally every 8 hours in addition to Oxycodone-Acetaminophen, 5 mg/325 mg, to be taken every 6 hours or as needed for pain management. This patient was instructed to follow up with her ENT surgeon in approximately one week for reassessment and reevaluation.
This patient did not however return for follow-up with her ENT surgeon a week after her discharge from the hospital admission, though she did return to the emergency department several months later with a chief complaint of right sided otalgia. At that time, the patient was seen and assessed by an advanced provider, whose physical exam found that the patient was overall not ill appearing. Her neck had full normal range of motion and no signs suggestive of meningismus. Further examination of the patient’s right ear indicated that her right tympanic membrane appeared macerated and was possibly bulbous with mild tenderness to palpation to the right preauricular area, right tragus, and right pinna. There was no
apparent swelling or discharge noted. The physical exam of this patient’s left ear, including the tympanic membrane, external auditory canal, tragus, and pinna was unremarkable. The patient denied further complaints or symptoms in relation to the left ear, including left sided otalgia, hearing changes or persisting decreased hearing, pinna displacement, swelling, or discharge. No lab work is available from this visit, though records indicate that she was eventually found to be appropriate for discharge from the emergency department with a diagnosis of right otitis media. The patient was given two prescriptions for treatment of the infection and management of her discomfort - a course of Augmentin, 125 mg to be taken every 8 hours, and Hydrocodone-Acetaminophen 5 mg/325 mg every 6 hours or p.r.n. for pain.
Demographics
Due to the rarity of mastoiditis in adults overall, there are fewer case studies and overall research on the demographic, pathogenesis, and treatment of adult mastoiditis. Acute otitis media (OM) is classically seen as a childhood disorder with most incidents occurring in children between 6 months and 18 months of age [8]. One retrospective analysis using the NEDS data from 2009-2011 is consistent with this trend, noting that most patients who presented to the emergency department for OM were pediatric cases with an average age of approximately 10 years old. although OM is largely considered a childhood disorder, a significant portion of these emergency department visits (20.1%) was composed of adults with an average age of 37 years [6]. Furthermore, adults make up the larger proportion (75.9%) of complicated OM cases such as acute mastoiditis, labyrinthitis, and facial paresis (top three in that order). Though the causation of this trend in adults is likely multifactorial in nature, one suspicion is the presence of underlying adult comorbidities— such as diabetes mellitus, cholesteatoma, or chronic otitis media— which can increase the likelihood of developing complications secondary to OM [9]. Among adults, the incidence of complications from OM, including intratemporal or intracranial processes, is relatively rare, occurring in less than 0.5% of cases [10][11]. Given the rarity of this worsening progression in adults, data is particularly limited in regards to further data as most of the literature surrounding OM discusses the pediatric age group. While some studies have claimed the overall incidence of acute OM has decreased in various parts of the world [12][13][14], there is some debate as to the actual cause. A common posited possibility that increased vaccination to pathogens such as S. pneumo and H. influenzae may play a role, while others believe the stricter diagnostic criteria for acute otitis media has decreased incidence [15].
Presentation
The majority of cases of mastoiditis are preceded by an episode of acute OM with or without cholesteatoma or with chronic recurrent OM [16][17]. Many patients are seen on an initial visit, either by a primary care provider or in the emergency setting typically with complaints that include a preceding upper respiratory tract infection, unilateral otalgia, and/or reduced or muffled hearing. Pain, while often severe in children, may vary from mild to severe in adults. Initial clinical suspicions of OM should be confirmed with an otologic exam revealing a bulging tympanic membrane and reduced mobility of the membrane with pneumatic pressure. If caught at this initial stage and treated appropriately, the risk of complications is reduced drastically [3]. However, as seen in this case, patients may not present initially with OM to a provider making prior visit history unavailable. This allows time for further progression of the infection which can lead to progressive destruction and coalescence of air cells and eventual medial sinus wall erosion. Mastoiditis rarely presents in this latent form seen in our patient with no prior acute episodes or recurrent history of OM [7]. Additionally, unique to this patient is the lack of risk factors and comorbidities that may increase a physician’s suspicion of mastoiditis. The patient’s history of tobacco use and childhood asthma increase the likelihood of OM, but she did not have documented comorbidities that existing literature identifies as increasing likelihood of severe complications secondary to OM, such as diabetes mellitus, chronic otitis media, cholesteatoma, craniofacial deformities, or immunosuppression [8][18].
Not only did our patient present with clinically advanced disease on initial presentation, but she also had minimal complaints compared to what would be expected for her clinical severity. Mastoiditis typically presents with otalgia, fever, dizziness/vertigo, otorrhea, posterior ear pain, retroauricular rubor, edema of the pinna, and a posteriorly displaced auricle [1][19]. Patients may also demonstrate leukocytosis and elevated CRP, though these findings are unreliable as current research shows contradictory evidence that suggests this may be related to the causative pathogens [2][4]. In latent mastoiditis, as with this patient, we may also see symptoms of rapid clinical deterioration and progression of the infection into complications with their own clinical findings such as meningitis, facial palsy, septic thrombosis of the sinus tract, subdural empyema or brain abscesses with focal neurological findings [4][7][20]. By contrast, this patient had a fairly benign clinical presentation. She was non-toxic, afebrile, without headache, neck stiffness, or erythema. She presented with unilateral, progressive otalgia and hearing reduction, with leukocytosis seen on labs. Physical examination was significant only for mild erythema with displacement of the auricle.
What can be reasonably inferred given the available literature, however, is the significance of this
patient’s case given her remarkable presentation and progression. Firstly, there is the surprising severity of her complications given her relatively benign complaints and physical examination upon her initial
assessment in the emergency department. More noteworthy still is that this 41-year-old patient’s progression from acute otitis media was complicated not only with coalescing mastoiditis. In addition, in her case further convoluted from this point leading to getting a MRI which indicated not only mastoiditis, but the presence deep ear abscess and additional incidental findings that were consistent with meningitis. Unlike most cases with complications relating to OM, this patient required not only broad spectrum intravenous antibiotics, but required admission to medicine and surgical intervention via a left sided myringotomy with Penrose drain placement, as well as a complete tympanomastoidectomy on the affected side.
Imaging
The patient’s minimal clinical symptoms brings up concerns about how to determine when imaging is indicated. What type of imaging to order and whether imaging is clinically indicated for acute otitis media/mastoiditis is a point of much debate within the current literature. It is widely accepted that a computed tomography (CT) with contrast of the head imaging performed when mastoiditis is suspected based on clinical symptoms [19][21][22]; however, some sources say imaging should be reserved for prolonged or complicated cases [23][24]. Both of these circumstances describe our patient as she had unilateral otalgia and hearing loss characteristic of OM or mastoiditis, and her symptoms were prolonged for more than three weeks despite not having any prior medical visits to reflect this. While a CT is the best initial image of choice due to speed and availability, typical findings such as fluid in the mastoids are nonspecific and thus should be correlated with clinical and microbiology findings [16]. There is conflicting data about when Magnetic Resonance Imaging (MRI) should be utilized. While many sources recommend that MRI should always be obtained, others state recommend MRI if there is suspicion of intracranial processes (ex. intracranial abscesses or sinus thrombosis). MRI will give a better view of the soft tissue components and intracranial changes that may not be visualized by CT [2][16][22][25]. MRI findings should be utilized in combination with clinical presentation as up to 82% of patients with mastoiditis on radiology reports (increased fluid signal intensity in the mastoid air cells on MRI) did not have clinical otologic disease [26]. Due to this conflicting data, this area seems to be one where further research is needed. Overall based on the current information available, it is recommended that early imaging be performed with CT at a minimum, and MRI when available. Imaging must be evaluated in correlation with clinical presentation and microbiology findings. Imaging can be crucial as intracranial complications may be clinically silent or have insidious onsets that may otherwise be missed without imaging. This idea was supported by our case in which the patient had a clinically mild case without fever or neurologic changes, but imaging revealed serious complications including coalescing mastoiditis with erosion into the jugular foraminal space, meningeal enhancement, and an intracranial abscess.
Risk Factors
Risk factors for pediatric acute or recurrent otitis media include allergy/atopy, upper respiratory infections, and snoring. Risk factors for pediatric chronic or recurrent otitis media include second hand smoke and low social status [27]. Other noted risk factors are immunosuppression and craniofacial abnormalities [28]. While most studies of risk factors have focused on pediatric populations, many pediatric risk factors are similar and have been extrapolated to the adult population [29]. Further research to confirm these risk factors can help better guide clinical management and risk of recurrence. A majority of mastoiditis cases are secondary to acute otitis media [30]. In the pre-antibiotic era, 20% of acute otitis media cases progressed to acute mastoiditis. After the implementation of antibiotics, mastoidectomies, and vaccinations against causative organisms such as the PCV-7 vaccine, the progression rate has dropped drastically with only 0.002% of children progressing to mastoiditis. Data for adult progression is limited due to the rarity of the presentation.
Of note, our patient had a past history of smoking and asthma. Both smoking and secondhand smoke have been associated with acute otitis media and therefore mastoiditis. One possible cause for increased acute otitis media in smokers and smoke exposure is that there is an association between smoking and an increased risk of pneumococcal colonization, a primary cause of acute otitis media. [31] Attempts to establish similar findings for H influenzae risk and smoking have not been as conclusive. In the past, there were reported cases of damage to the middle ear structures and impairment of valsalva due to smoking, but attempts to confirm such a theory have been inconclusive. [32][33][34] This association requires further evaluation as smoking may present the need for more aggressive screening for acute otitis media and mastoiditis such as imaging or surgical evaluation. While the connection between allergies and acute otitis media has been well-established, connections of asthma have not been as clearly highlighted. Pediatric studies have shown correlation between asthma predicting acute otitis media later in life and vise versa but it is unclear if these trends extend past adolescence. [35]
Management
As previously mentioned, mastoiditis presents often as a complication of acute otitis media. It often occurs in the setting of untreated acute otitis media or in cases of antibiotic resistance. Patients who do progress to mastoiditis often do so after having been treated with antibiotics initially for acute otitis media. Antibiotic choice should cover the most common causes of acute otitis media including S. pneumoniae, H. influenzae, and M. catarhallis. AAFP recommends first line treatment dosage for acute otitis media as amoxicillin 80 - 90 mg/kg per day in two divided doses. Amoxicillin-clavulanate 90mg/kg per day of amoxicillin with 6.4 mg/kg per day of clavulanate in two divided doses may be considered if the patient has received amoxicillin in the last thirty days or have otitis/conjunctivitis syndrome [36].
Patients can often be treated on antibiotics for five to seven days if infection is mild/moderate. In the cases of severe infection, a ten day course of antibiotics is recommended. Supplementary workup including middle ear fluid cultures, blood cultures, and IV antibiotics may be indicated for severe presentations. Failure to respond to first line antibiotics may benefit from a change to a second line antibiotic choice such as a cephalosporin(ex. ceftriaxone) or fluoroquinolone(ex. levofloxacin or moxifloxacin). Evaluating antibiotic sensitivity of previous middle ear or blood cultures may help to guide therapeutic decisions but is often not necessary unless the patient is unresponsive or severely ill.
Most cases of acute otitis media may have subclinical mastoiditis. If initial acute otitis media is left untreated or antibiotic treatment is unsuccessful, progression to complications such as mastoiditis can occur. In such a scenario, evaluating the sensitivity of cultures is important to determine if the patient is receiving an appropriate antibiotic choice for the identified pathogen. As discussed above, indications for imaging including CT/MRI with or without contrast vary depending on clinical severity of the patients presentation. Surgery is indicated for patients with abscess formation or infected tissue evidenced on imaging in the middle ear or mastoid. Surgery may also be beneficial in maintaining the anatomical contour for acoustics or restoration of tympanic/mastoid aeration [37][38]. The most common surgical options include myringotomy, tympanoplasty, or mastoidectomy. Mastoidectomy is the most invasive of the procedures mentioned and focuses on removing infected tissue while preserving the middle ear and skull anatomy. There are multiple surgical approaches to mastoidectomy including intact canal wall and canal wall down approaches but no controlled prospective studies are currently available to compare complications or success rates. Along with surgical debridement, tools such as Penrose drains and Otowicks can assist with postsurgical management to improve drainage and topical antibiotic application respectively.
Postsurgical management often includes inpatient expectant management for complications of surgery. The patient should have the Penrose drain removed on postoperative day number two. Mastoid dressings should be changed daily until discharge and the patient is to be instructed to remove dressing two to three days after discharge for a total of five days of compression. While inpatient, patient should received continued appropriate antibiotics and be sent home with a prescription of oral levofloxacin, amoxicillin with clavulanate, or clindamycin for a fourteen day course Care should be placed in keeping the surgical site dry for a few days following discharge. It may be recommended that the patient have a second tympanoplasty with ossiculoplasty to evaluate the middle ear anatomy and any need for possible revision [39].


Mastoiditis is most often a complication of acute otitis media. If left untreated, the incidence of mastoiditis secondary to acute otitis media is 50%, however, the incidence has been estimated by some studies to have decreased to 0.4% with the introduction of antibiotics [40]. Without treatment, complications resulting from mastoiditis encompass findings such as abscess formation, labyrinthitis, meningitis, thrombosis, facial nerve dysfunction, hearing loss, and sinus occlusion [41]. Abscess formation tends to be a typical complication of coalescent mastoiditis. Bezold’s abscess is a highly uncommon deep neck/infratemporal abscess that can originate from organisms such as Streptococcus. This organism was also cultured from the intracranial abscess that required surgical intervention in our patient. While it is rather uncommon for the formation of Bezold’s abscess to occur, given the efficiency of modern-day antibiotics, reports of the abscess were more prevalent among adults with a 55.6% of documented cases, and males, 61% of documented cases [42]. Thrombosis of the sigmoid sinus, lateral sinus, and internal jugular, and facial nerve paralysis/dysfunction are both exceedingly rare complications, with almost no case reports found in adults since the initiation of antibiotics. [43] One of the more severe complications of mastoiditis is meningitis as seen in our patient’s case. We could find no other cases within the literature of meningitis developing secondary to mastoiditis, with the same demographics or presentation of our patient. Of the 4 cases referenced, 2 of the individuals were significantly older (73 y/o F and 70 y/o M), one of which had been suffering from chronic mastoiditis [44/45], and the other 2 cases describe individuals who were significantly younger than our patient (11 y/o M and 25 y/o M). All of the cases described had either chronic mastoiditis or presented with severe toxic or neurologic complications such as presenting with altered levels of consciousness. Our patient was afebrile, nontoxic, and with no neurologic findings despite having coalescent mastoiditis with an abscess and meningeal inflammation seen on imaging, making this case unique within the current literature.
Bacterial Pathogens
Bacterial cultures obtained during surgical management of the patient in our study grew S. pneumoniae with pan-sensitivity. With the development of antibiotic regimens and preventative measures such as S. pneumniae and H. influenza vaccines, the general incidence of acute otitis media declined in the last few decades. Other studies, however, have claimed that overall incidence has not changed but rather the epidemiology seems to have shifted. Proportions of causative pathogens continue to shift and include more resistant or non-typable strains of these bacteria. [46/47/48] Pediatric cases of acute otitis media were more often due to S. pneumoniae, H. influenzae, and M. catarrhalis. Pathogens involved in acute otitis media in adult cases had more variety. Some studies showed high prevalence of S. pneumoniae and H influenzae similar to pediatric populations. [49] The limited adult studies have seen H. influenzae, S. aureus (including resistant strains), and S. pyogenes as the predominant bacteria isolated. [2/50/51] Pathogens identified in adult cases of acute otitis media compared to adult acute/latent mastoiditis were similar. [2] The anaerobic bacteria Fusobacterium necrophorum has also recently been implicated in an increased proportion of pediatric acute mastoiditis although data is limited and implications for adult cases have not been pursued. [52] Pediatric studies have also seen a correlation between P. aeruginosa and recurrent acute mastoiditis. [53] These studies highlight the changing epidemiology of these disorders and continued need for research into changes in microbiological causes of acute otitis media and mastoiditis in order to guide management.
While otitis media and mastoiditis is less common in adults, cases that present often do require more aggressive treatment or surgical intervention. Because these cases are less common, patients may not know the possible risks of not treating otitis media appropriately. Key focuses for this case as well as other adult cases of mastoiditis should address presentation of symptoms, at-risk demographics, diagnostic workup/imaging, appropriate antibiotic coverage, and possible need for surgical intervention. Complications, while rare, should be considered and discussed with patients. Further studies identifying changes in common pathogens causing otitis media or mastoiditis may be beneficial.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
