AUCTORES
Globalize your Research
Research Article
*Corresponding Author: Ahmed Elbayomy, MD Department of Neurological Surgery, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA.
Citation: Ahmed Elbayomy, Jason Kim, Simon Ammanuel, Momin Mohis, Ian Koszewski, et al, (2024), Socioeconomic Disparities in the Utilization of Endoscopic Transsphenoidal Pituitary Surgery: A Retrospective Analysis of the National Inpatient Sample, J. Neuroscience and Neurological Surgery, 14(9); DOI:10.31579/2578-8868/318
Copyright: ©, 2024, Ahmed Elbayomy. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Received: 06 May 2024 | Accepted: 14 October 2024 | Published: 01 November 2024
Keywords: glioblastoma; adult diffuse glioma; heberferon
Introduction Pituitary neoplasms account for 15% of all intracranial neoplasms and affect 20% of the population.
Objective We aim to use the National Inpatient Sample (NIS) to ascertain disparities in utilization and outcomes among endoscopic endonasal pituitary surgery patients.
Methods NIS was used from 2010 to 2020. Pearson's v2, Fisher's Exact, and independent 2-tailed t-tests were used to assess patient characteristics and outcomes. A logistic regression model was used to compare in-hospital mortality and post-operative complications between Racial groups. Statistically significant postoperative complications were analyzed with a multivariable logistic regression to determine the independent impact of obesity on postoperative outcomes.
Results Hospitalization rates for this procedure declined significantly over the decade, from 10,279 in 2010 to 5,875 in 2020 (trend p value < 0.001). The majority of patients were between 25 and 64 years old (72.16%), with 60.73% having no comorbidities. While the gender distribution was nearly even, disparities emerged across racial and socioeconomic groups. Black and Hispanic patients were more likely to reside in lower income zip codes and depend on Medicaid compared to White patients. Black patients had higher odds of any postoperative complication (adjusted OR: 1.14, p=0.003) and specific complications like diabetes insipidus, fluid/electrolyte disorders, and renal/urinary issues compared to White patients. Both Black and Hispanic patients faced higher mortality risks post-surgery compared to White patients (adjusted OR: 2.62 and 2.44, respectively, p<0.05). Medicaid coverage was associated with higher odds of any complication (adjusted OR: 1.18, p=0.016), while private insurance was linked to lower odds (adjusted OR: 0.88, p=0.015).Patients in the lowest income quartile had higher odds of complications compared to those in higher quartiles. Obesity independently predicted increased odds of pulmonary, renal, and hemorrhagic complications.
Conclusion Despite advancements in endoscopic endonasal pituitary surgery, disparities in access and outcomes persist across racial, socioeconomic, and insurance groups. These findings underscore the need for targeted interventions to address these inequalities and ensure equitable access to quality care.
Pituitary neoplasms account for 15% of all intracranial neoplasms and impact approximately 20% of the global population [1]. The mechanism underlying development and growth of pituitary neoplasms remains largely elusive, though current hypotheses propose hormonal changes as a key driver [1, 2]. Additionally, it's posited that these hormonal responses could be influenced by stress levels, leading to speculation that socioeconomic factors might play a role in the disease's pathophysiology [1, 3]. Historically, symptomatic tumors, which are capable of inducing neurological deficits, have been managed through microscopic surgical interventions [4].
Over the past two decades, the advent of endoscopic pituitary surgery has marked a significant evolution in treatment practices [5]. Comparative studies have consistently shown the endoscopic endonasal technique to be safer and more effective than its microscopic counterpart [4, 5]. This technique's advantages, including superior visualization and shorter hospital stays, have contributed to its increasing adoption for treating pituitary tumors [4]. However, the literature has not fully quantified the impact of preoperative factors such as high BMI, limited surgeon experience, and female gender on the risk of complications, notably cerebrospinal fluid (CSF) leaks [5]. Additionally, studies have exposed stark disparities in access to neuro-oncological care related to socioeconomic status and race/ethnicity, highlighting the critical issue of inequality within the healthcare system [5, 6].
Despite the recognized importance of socioeconomic factors, there appears to be a lack of comprehensive analyses on how socioeconomic status (SES) influences the complications and outcomes of endoscopic pituitary surgery. Our study seeks to address this gap by leveraging data from the National Inpatient Sample (NIS) to explore variations in surgical utilization and patient outcomes based on procedure type (endoscopic endonasal or tranfrontal), SES, race, payer type, and obesity. and. We also evaluated the mortality and morbidity associated with these procedures based on medical and endocrine complications and 30day readmission for CSF leak.
Study Design and Patient Eligibility
A retrospective cross-sectional investigation was conducted utilizing the NIS from 2010 to 2020, which is part of the Healthcare Cost and Utilization Project (HCUP) from the Agency for Healthcare Research and Quality. Furthermore, the NIS is a hospital discharge database that represents 20% of all inpatient admissions to non-federal hospitals in the U.S. [7]. Prior to 2012, the NIS represented 100% of discharges from a 20% sample of all hospitals in the HCUP strata. However, beginning in 2012, the sampling procedure was modified to reflect a 20% sample of hospital discharges from all HCUP hospitals. Consequently, the database name was modified in 2012 to reflect these changes. Each discharge in the NIS database represents one hospitalization. In this regard, the NIS does not have unique patient data; therefore, one patient may represent multiple discharges. We also examined the national Readmission Database (NRD) for the same period, focusing on 30-day readnission specifically for CSF leaks.
In the present study, a discharge is referred to as a patient. All patients undergoing endoscopic transsphenoidal and transfrontal pituitary surgeries were identified using the International Classification of Diseases, the 9th Revision (ICD-9 CM) codes (07.62, 07.65, and 07.61, 07.64), and the 10th Revision (ICD-10 CM) codes (0GB04ZX,0GB04ZZ, and 0GB00ZZ, 0GT00ZZ) for diagnosis and procedure coding for endoscopic transsphenoidal and transfrontal approaches, respectively.
Data Collection and Outcomes
Patient-level data includes the patient's age, sex, race (White, Black, Hispanic, Asian or Pacific Islander, Native American, and others), median household income in the patient's zip code (1st quartile, 2nd quartile, 3rd quartile, and 4th quartile), primary expected payer (Medicare, Medicaid, private insurance, and uninsured), discharge status (routine, transfer to short-term hospital, transfer to another facility [including skilled nursing facility (SNF), intermediate care facility (ICF), another type of facility], home health care, against medical advice [AMA], died in hospital, discharged alive, discharged to court/law enforcement, destination unknown), length of stay, hospital bed size (small, medium, and large), teaching status, hospital region (Northeast, Midwest, South, and West), along with location (urban and rural), principal diagnosis, as well as secondary diagnosis using the ICD-9 and ICD-10 revisions. The comorbidity burden was assessed using Deyo's modification of Charlson's comorbidity index (CCI). Finally, in-hospital mortality is directly coded in the NIS database, and complications were examined in all secondary diagnosis fields using ICD-9 CM and ICD-10 CM codes.
The analyzed complications included CNS infection, CSF leak, diabetes insipidus (DI), iatrogenic pituitary disorder, fluid and electrolyte disorders, neurological disorders, pulmonary disorders, cardiac disorders, renal disorders, hemorrhage, and hematoma. All statistical calculations for this analysis were performed using STATA version 17. Additionally, patient characteristics and outcome variables were tested using Pearson's chi-square test, Fisher's exact test, and independent two-tailed t-tests, as appropriate. Variable differences between the groups were deemed to be statistically significant if the P-value was less than 0.05. Moreover, a logistic regression model for comparison of in-hospital mortality and postoperative complications between racial groups included race, age, sex, and CCI as independent variables. Furthermore, statistically significant postoperative complications were analyzed with a multivariable logistic regression (which accounts for age, gender, race, and statistically significant demographic differences) to determine the independent impact of obesity on postoperative outcomes.
Over the span of a decade from 2010 to 2020, a total of 82,249 patients who underwent endoscopic transsphenoidal pituitary surgery were identified. The hospitalization rates for endoscopic transsphenoidal pituitary surgeries in the United States displayed a notable decline. The rates started at 10,279 hospitalizations in 2010, peaked slightly in 2011 with 10,798 cases, and then followed a downward trajectory to 5,875 by 2020. This trend of decreasing hospitalization rates was statistically significant, with a trend p-value of less than 0.001. (Table1, fig 1).
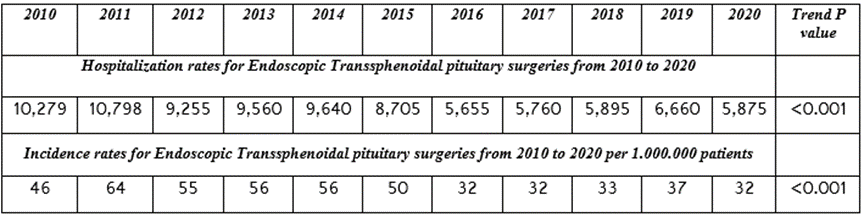
Table 1
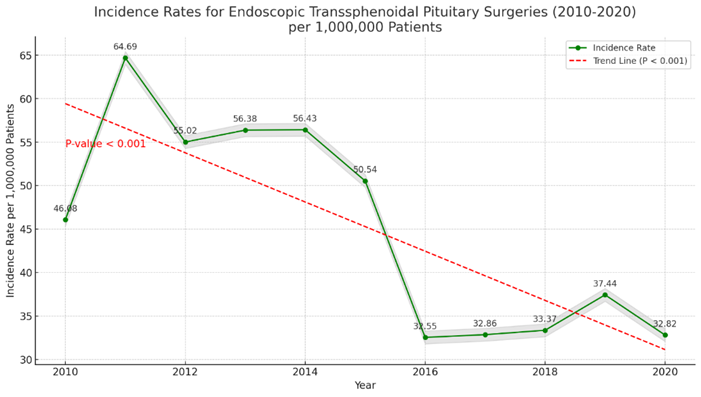
Figure 1: Incidence rates for endoscopic transsphenoidal pituitary surgeries from 2010 to 2020 per 1.000.000 patients. This figure was created with M.S. Excel version X.
The incidence rates of endoscopic transsphenoidal pituitary surgery in the U.S. were calculated using the annual estimates of the U.S. resident population on July 1st as the denominator. In parallel, the incidence rates of these surgeries per 1,000,000 patients also saw a decline over the same period. The incidence rate was at its highest in 2011, with 64 cases per million, before gradually decreasing to 32 cases per million by 2020, mirroring the trend observed in hospitalization rates. This reduction in both hospitalization and incidence rates underscores a significant shift in the management of pituitary disorders, potentially indicating improvements in non-surgical interventions, changes in clinical guidelines, or access to care, and is also statistically significant with a trend p-value of less than 0.001. (Table 1, Figure 2).
In this study, patient age distribution was as follows: 22,597 (27.47%) were between 25 to 44 years, 36,758 (44.69%) were aged 45 to 64 years, 22,072 (26.83%) were in the 65 to 84 years age group, and 823 (1.00%) were 80 years or older, with this age distribution being statistically significant (P<0>Among the study population, the vast majority (89.61%, n=73,687) were routinely discharged to their homes. A smaller proportion were
transferred to short-term hospitals (0.35%, n=290), skilled nursing or intermediate care facilities (3.75%, n=3091), or received home health care (5.74%, n=4725). A negligible number were discharged against medical advice (0.09%, n=75), while a few patients either died or had an unknown discharge status (0.04%, n=352), indicating significant differences in discharge outcomes (P<0 n=40,675) n=41,436) n=4845) n=11377) n=65675), n=74209), n=7697)>Geographically, hospital patient counts were as follows: Northeast (18.70%, n=15,387), Midwest (19.91%, n=16,380), South (36.61%, n=30,114), and West (24.76%, n=20,368), exhibiting a mean hospital stay of 4.43 days, which was statistically significant (P<0 n=44,443), n=22,971), n=8,053), n=2,895), n=3,292), n=434) n=21,446), n=20,564), n=19,566), n=18,844)>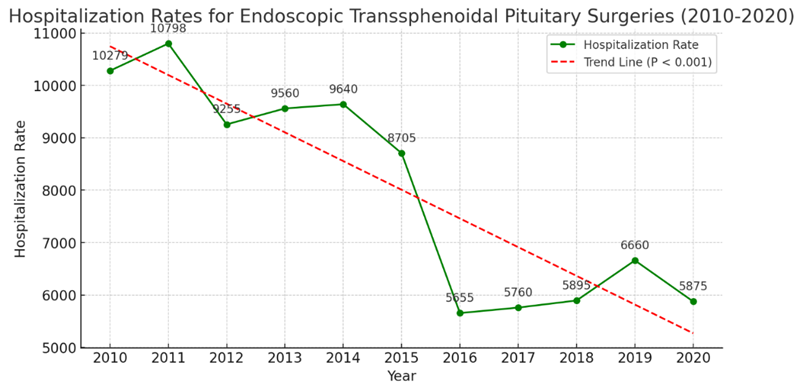
Figure 2: Hospitalization rates for endoscopic transsphenoidal pituitary surgeries from 2010 to 2020. This figure was created with M.S. Excel version X.
Racial Disparities
This study identified 74,547 patients—White (48,356), Black (15,133), and Hispanic (11,058)—undergoing endoscopic transsphenoidal pituitary surgery. The analysis revealed Hispanic patients as the youngest group with a mean age of 48.04 years, closely followed by Black (53.08 years) and White patients (53.13 years), showing significant age differences (P<0>Variable White (N= 48356), % Black (N= 15133), % Hispanic (N= 11058), % P-value Age (mean ± S.D.) 53.13 ± 19.60 53.08 ±29.35 48.04 ±35.91 <0> 25 to 44 25.40% 25.34% 35.84% 45 to 64 43.54% 48.20% 44.81% 65 to 84 29.85% 25.95% 18.71% 85 and older 1.21% 0.51% 0.64% CCI <0> Zero 63.72% 53.26% 62.93% One 21.50% 26.51% 24.37% Two 7.91% 9.91% 6.71% Three and higher 6.87% 10.32% 5.99% Sex <0> Male 49.83% 47.73% 45.88% Bed Size 0.818 Small 5.27% 5.92% 4.95% Medium 14.37% 14.44% 15.14% Large 80.36% 79.63% 79.91% Hospital Region <0> Northeast 20.29% 18.11% 12.93% Midwest 20.91% 16.41% 7.94% South 35.81% 54.82% 37.10% West 22.99% 10.65% 42.03% LOS 4.05 ± 6.96 5.38 ± 14.26 5.10 ± 17.79 Payer <0> Medicare 29.03% 28.32% 17.49% Medicaid 6.71% 14.98% 20.91% Private 58.71% 45.80% 46.58% Self-pay 2.05% 4.30% 8.00% No charge 0.19% 0.71% 1.79% Others 3.31% 5.89% 5.22% Disposition <0> Routine 90.95% 85.39% 91.29% Short term hosp 0.25% 0.50% 0.37% SNF, ICF, Another 3.49% 5.15% 2.50% HHC 5.03% 8.06% 5.31% Others 0.28% 0.90% 0.53% Teaching Status <0> Non-teaching 10.02% 8.00% 11.58% Teaching 89.98% 92.00% 88.42% Median Income <0> 1st quartile 19.33% 40.35% 32.07% 2nd quartile 24.18% 23.34% 22.92% 3rd quartile 27.06% 20.10% 26.69% 4th quartile 29.43% 16.22% 18.32%
Table 2: Patients' demographics and Hospital characteristics by Racial and Ethnic Group
Abbreviations: LOS, Length of stay; Short term hosp; Short-term hospital; SNF, Skilled Nursing Facility ; ICF, Intermediate Care Facility;Another, Another type of facility;HCC, Home Health Care.
Analysis of Complications by Race
Table 3 summarizes the in-hospital mortality and complication rates among racial groups, with Table 4 detailing the odds of complications for Black and Hispanic patients relative to White patients. Black patients had significantly higher odds of experiencing any postoperative complication (unadjusted OR [uOR]: 1.19 [1.09-1.30], P<0 P=0.003) P=0.03), P=0.004) P=0.02),>Complications White, % Black, % Hispanic, % P-value Died 0.22% 0.70% 0.49% <0> Any Complication 35.98% 40.11% 38.34% <0> CSF leak 7.53% 8.38% 9.39% 0.013 CNS Infection 0.88% 0.75% 0.97% 0.69 Diabetes Insipidus 14.89% 16.62% 16.88% 0.014% Iatrogenic Pituitary Disorder 1.07% 1.03% 0.85% 0.66% Fluid and Electrolyte Disorders 14.23% 17.55% 14.50% <0> Neurological Diseases 6.91% 7.07% 7.36% 0.77% Pulmonary Diseases 1.80% 2.16% 1.81% 0.42% Cardiac Diseases 0.66% 0.59% 0.41% 0.40% Renal Diseases 1.60% 4.08% 1.71% <0> Hemorrhage 0.89% 1.29% 1.14% 0.15%
Table 3: Complication and Mortality Rate by Racial and Ethnic Groups
| Complications | Black | Hispanic | ||||||
| uOR (95% CI) | P-value | aOR (95% CI) | P-value | OR (95% CI) | P-value | aOR (95% CI) | P-value | |
| Died | 3.20(1.69-6.03) | <0> | 2.62(1.36-5.06) | 0.004 | 2.24(1.06-4.71) | 0.032 | 2.44(1.11-5.33) | 0.025 |
| Any Complication | 1.19(1.09-1.30) | <0> | 1.14(1.04-1.24) | 0.003 | 1.10(1.00-1.22) | 0.045 | 1.07(0.97-1.18) | 0.14 |
| CSF leak | 1.12(0.96-1.31) | 0.13 | 1.08(0.91-1.27) | 0.34 | 1.27(1.05-1.53) | 0.010 | 1.24(1.01-1.51) | 0.034 |
| CNS Infection | 0.85(0.54-1.34) | 0.49 | 0.75(0.47-1.19) | 0.23 | 1.09(0.68-1.76) | 0.70 | 1.10(0.68-1.77) | 0.68 |
| Diabetes Insipidus | 1.13(1.02-1.27) | 0.02 | 1.15(1.02-1.28) | 0.016 | 1.16(1.01-1.32) | 0.02 | 1.00(0.88-1.15) | 0.91 |
| Iatrogenic Pituitary Disorder | 0.96(0.64-1.43) | 0.86 | 0.93(0.62-1.40) | 0.76 | 0.79(0.48-1.31) | 0.37 | 0.77(0.46-1.29) | 0.33 |
| Fluid and Electrolyte Disorders | 1.28(1.14-1.44) | <0> | 1.21(1.08-1.36) | <0> | 1.02(0.89-1.17) | 0.75 | 1.10(0.95-1.26) | 0.16 |
| Neurological Diseases | 1.02(0.87-1.20) | 0.76 | 0.99(0.84-1.17) | 0.97 | 1.07(0.87-1.30) | 0.50 | 1.05(0.86-1.28) | 0.61 |
| Pulmonary Diseases | 1.20(0.90-1.60) | 0.20 | 1.07(0.80-1.43) | 0.63 | 1.00(0.71-1.41) | 0.97 | 1.09(0.77-1.53) | 0.60 |
| Cardiac Diseases | 0.90(0.53-1.53) | 0.71 | 0.81(0.48-1.38) | 0.45 | 0.62(0.31-1.24) | 0.18 | 0.75(0.37-1.49) | 0.41 |
| Renal Diseases | 2.61(2.05-3.32) | <0> | 2.35(1.83-3.02) | <0> | 1.07(0.73-1.56) | 0.71 | 1.31(0.90-1.93) | 0.15 |
| Hemorrhage | 1.46(0.99-2.14) | 0.053 | 1.42(0.96-2.10) | 0.073 | 1.28(0.77-2.15) | 0.32 | 1.46(0.87-2.46) | 0.14 |
Table 4: In-hospital mortality and postoperative complications in Black and Hispanic patients compared to White patients.
Analysis of Complications by Insurance Status
Table 5 delineates the odds of postoperative complications across different insurance types relative to Medicare. Patients with Medicaid exhibited higher odds of any complication (uOR: 1.31 [1.17-1.46], P<0 P=0.016), P=0.008; P=0.015). P=0.007) P=0.03), P=0.008).>
Table 5: In-hospital mortality and postoperative complications by primary expected payer compared to Medicare.
Analysis of Complications by Median House Income by Zip Code
Patients residing in the 2nd and 3rd quartiles of median household income demonstrated significantly lower odds of any postoperative complications compared to those in the 1st quartile, with uOR of 0.87 and 0.86, and aOR of 0.90 and 0.89, respectively (P≤0.02 for all). Additionally, those in the 4th quartile were notably less likely to develop CNS infections (uOR: 0.52, P=0.011; aOR: 0.50, P=0.014). The odds of fluid/electrolyte disorders also decreased in the 2nd, 3rd, and 4th quartiles compared to the 1st, with respective uORs of 0.80, 0.78, and 0.80, and aORs reflecting a consistent reduction in risk (P≤0.033). Moreover, those in the 3rd and 4th quartiles faced significantly lower odds of renal complications, showcasing the protective effect of higher socioeconomic status (uOR: 0.53 and 0.54, P=0.001 for both; aOR: 0.54 and 0.64, P≤0.008) (Table 6).
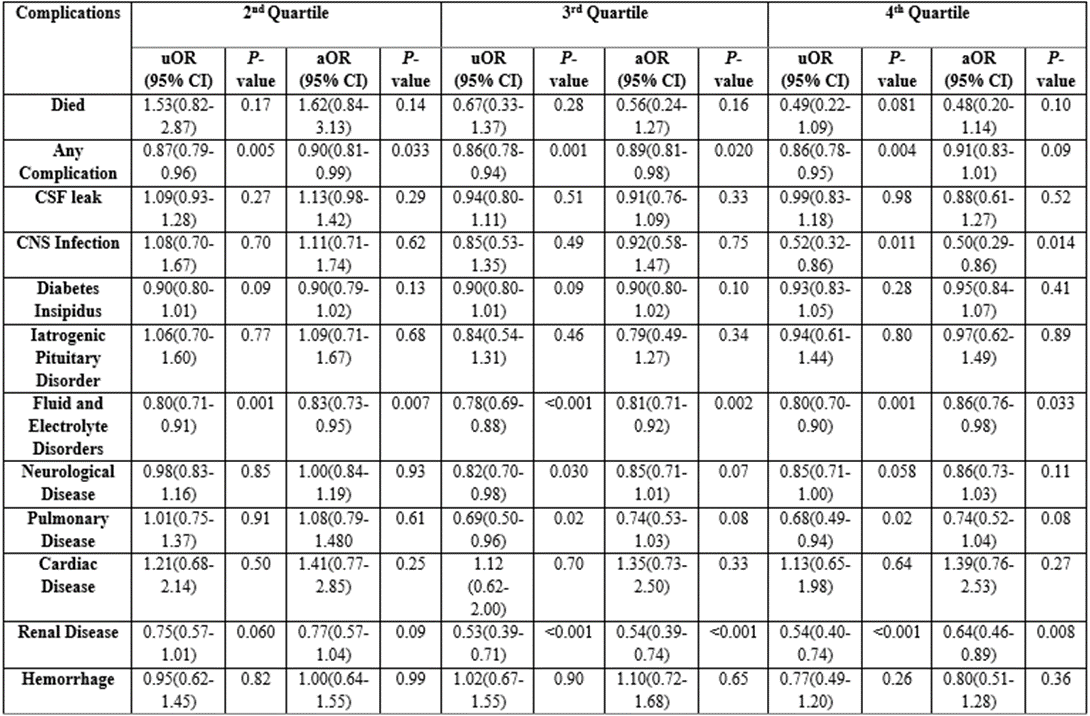
Table 6: In-hospital mortality and postoperative complications by hospital volume quartiles compared to the lowest quartile.
Analysis of CSF Leak After Endoscopic Transsphenoidal Pituitary Surgery and Transfrontal Pituitary surgery
Our data revealed a significant difference in the proportions of patients experiencing CSF leaks with endoscopic transsphenoidal and transfrontal pituitary surgeries. CSF leaks were reported in 8.0% of patients undergoing the endoscopic approach compared to 10.3% in the transfrontal group (p < 0>To further investigate the accuracy of CSF leak reporting, we examined the NRD for the same period, focusing on 30-day readmissions specifically for CSF leaks. This analysis revealed 529 readmission cases (10.11%) following endoscopic transsphenoidal surgery and 152 cases (10.79%) after transfrontal surgery. Readmission rates based on sex were similar across both surgical approaches, with no statistically significant
differences observed (p = 0.58 and 0.67 for endoscopic and transfrontal groups, respectively).
Interestingly, a linear trend analysis of CSF leak readmissions showed an increase over time for the endoscopic group, with a statistically significant odds ratio of 1.07 (p = 0.002). This trend was not observed in the transfrontal group, where the odds ratio was 1.05 with a non-significant p-value (1.65).
Analysis of Obesity on Mortality and Postoperative Complications for Endoscopic Transsphenoidal Pituitary Surgery
Univariate regression analysis revealed significantly lower odds of hemorrhagic complications (OR: 0.65, P=0.015), alongside higher odds for developing overall complications (OR: 1.17, P≤0.001), CNS infection (OR: 1.56, P=0.014), DI (OR: 1.48, P=0.017), and complications related to fluids and electrolytes (OR: 1.11, P=0.046), pulmonary (OR: 1.53, P<0 P=0.015). P=0.027), P=0.005) P=0.027)>Variables uOR (95% CI) P-value aOR (95% CI) P-value Died 0.82(0.43-1.55) 0.55 0.53(0.23-1.24) 0.15 Any Complication 1.17(1.08-1.26) <0> 1.08(0.99-1.18) 0.060 CSF leak 1.19(1.04-1.36) 0.010 1.00(0.86-1.15) 0.99 CNS Infection 1.56(1.09-2.25) 0.014 1.20(1.04-1.17) 0.37 Diabetes Insipidus 1.09(0.98-1.20) 0.082 0.99(0.88-1.10) 0.85 Iatrogenic Pituitary Disorder 1.48(1.07-2.05) 0.017 1.41(0.96-2.06) 0.073 Fluid and Electrolyte Disorders 1.11(1.00-1.24) 0.046 1.08(0.96-1.21) 0.17 Neurological Diseases 1.05(0.90-1.22) 0.46 1.05(0.90-1.24) 0.49 Pulmonary Diseases 1.53(1.20-1.95) <0> 1.50(1.13-2.01) 0.005 Cardiac Diseases 0.81(0.47-1.37) 0.43 0.82(0.47-1.42) 0.48 Renal Diseases 1.52(1.21-1.92) <0> 1.33(1.03-1.71) 0.027 Hemorrhage 0.65(0.63-0.89) 0.015 0.57(0.35-0.94) 0.027
Table 7: Effect of obesity on endoscopic transsphenoidal pituitary surgery
Analysis of Mortality and Postoperative Complications Between Endoscopic Transsphenoidal and Transfrontal Approaches for Pituitary Surgeries
Among the surgical cases reviewed, 88,081 underwent endoscopictranssphenoidal approach, while 21,836 received a transfrontal approach. The analysis revealed that the transfrontal approach was associated with a higher incidence of mortality (0.88% vs. 0.38%, P<0 P=0.013),>Variables Transsphenoidal (N=88081), % Transfrontal (N= 21836), % P-value Died 0.38% 0.88% <0> Any Complication 36.88% 45.11% <0> CSF leak 8.00% 10.3% <0> CNS Infection 0.86% 1.27% 0.013 Diabetes Insipidus 15.48% 22.69% <0> Iatrogenic Pituitary Disorder 1.03% 2.00% <0> Fluid and Electrolyte Disorders 14.70% 19.92% <0> Neurological Diseases 6.95% 5.54% <0> Pulmonary Diseases 1.85% 3.52% <0> Cardiac Diseases 0.58% 0.67% 0.45 Renal Diseases 2.01% 3.03% <0> Hemorrhage 0.99% 1.08% 0.60
Table 8: Comparison between Endoscopic transsphenoidal and transfrontal approach for mortality and postoperative complications
Over the decade spanning 2010 to 2020, patients undergoing endoscopic transsphenoidal pituitary surgery predominantly fell within the 25 to 44 age group, with a significant majority (61.47%) presenting no comorbidities (CCI = 0). Female patients slightly outnumbered male patients (51.18% vs. 48.82%). Private insurance was the primary coverage for most patients, followed by Medicare. While surgical interventions were broadly distributed across all income quartiles, the highest income group exhibited the greatest surgery rates. Predominantly, these procedures were executed in academic settings, with a staggering 90% taking place in large teaching hospitals. Regional analysis showed that Southern and Western centers accounted for a larger share of cases, surpassing those in the Midwest and Northeast. These findings suggest that socioeconomic factors significantly influence access to and outcomes of endoscopic transsphenoidal pituitary surgery. The distribution of surgeries across different income quartiles, with a skew towards higher income groups, indicates potential barriers to access for lower-income patients. This disparity emphasizes the need to address socioeconomic factors as key determinants of health care access and quality.
A previous study analyzing pituitary adenomas and carcinomas from 1997 to 2016 using the NIS database revealed a peak incidence among individuals aged 65 to 84 [1]. This trend suggests an enhanced detection of pituitary adenomas over the years, likely attributed to the proliferation of head imaging techniques that increase the rate of incidental findings [8]. Despite observing a higher incidence in women, statistical significance was not established in sex differences [1]. Interestingly, while urban centers reported a higher incidence rate, our analysis indicates a predominant surgical treatment of adenomas in academic centers [1]. This pattern implies a referral system funneling patients from rural or suburban diagnoses to academic surgical facilities, highlighting concerns about equitable access to care for those living far from such centers. Additionally, the most pronounced disparities were observed in the incidence and treatment utilization across different racial demographics. The notable emphasis on academic centers for surgical treatment raises concerns about access for patients in non-urban areas, potentially exacerbating existing socioeconomic and geographic disparities. This situation underscores the importance of developing strategies to ensure equitable access to specialized surgical care, irrespective of patients' geographical location or socioeconomic status.
Research reveals variable incidences of pituitary tumors across racial groups, with Black Americans experiencing nearly double the incidence rate of their White, Asian, and American Indian counterparts, particularly among older populations. Despite a similar peak incidence age between Black, White, and Asian Americans (75-79 years) as indicated in previous studies [8], our analysis uncovers a significant treatment gap, showing lower surgical intervention rates for Black Americans compared to White Americans. This disparity could be attributed to several factors, including higher stroke rates among Black Americans leading to more frequent imaging and incidental tumor findings not requiring surgery, systemic barriers limiting access to specialized neuro-oncological care and patient education, and insurance-based discrepancies. Predominantly, private insurance serves as the primary payer, whereas Black and Hispanic patients are more likely to depend on Medicare, Medicaid, or lack insurance, constraining their surgical treatment options. Furthermore, there appears to be a financial incentive for prioritizing well-insured patients, who are mostly White, for surgery over other monitoring approaches that might be equally viable. The disparities in surgical intervention rates among Black Americans compared to White Americans highlight significant racial inequalities in healthcare. These findings point to the need for targeted interventions to reduce barriers to care and improve surgical outcomes for racial and ethnic minorities. Understanding and addressing the root causes of these disparities, including systemic barriers and insurance-based discrepancies, are critical steps toward achieving equity in healthcare.
In our study, similar to patterns of utilization, we observed potential disparities in outcomes among different racial groups. Notably, both Black and Hispanic Americans exhibited higher odds of total postoperative complications compared to White Americans, with Black Americans experiencing not only higher mortality rates but also an increased incidence of specific complications such as diabetes insipidus, fluid/electrolyte disorders, and renal and urinary issues. This discrepancy might be linked to the higher prevalence of renal disease and hypertension observed in the Black population relative to White Americans. Furthermore, the connection between electrolyte/fluid disorders and income disparities could point to issues like inadequate nutrition or lower caloric intake, leading to electrolyte imbalances and compromised fluid status. These outcome disparities may stem from a range of underlying causes, including socioeconomic inequalities and diminished trust in the healthcare system, reflecting the complex interplay between health outcomes and social determinants of health.
Our study uncovered a notable discrepancy in postoperative complications based on the type of insurance, where patients covered by Medicaid experienced a higher rate of complications compared to those with private insurance, who demonstrated lower odds of such outcomes. Furthermore, we observed an inverse relationship between income levels and complication rates, with patients in the highest income quartile exhibiting lower odds of experiencing complications than those in the lowest quartile. These findings are consistent with prior research indicating an association between Medicare or Medicaid coverage and adverse outcomes, particularly in studies examining frailty [11]. Additionally, our results suggest a potential interaction effect between low-income status and increased frailty among patients undergoing pituitary surgery. This interaction could mean that the longer hospital stays, and higher medical expenses typically associated with frailty might exert a more significant burden on patients with lower income levels, highlighting the compounded impact of socioeconomic factors on health outcomes.
Our study revealed a notable difference in the proportion of patients experiencing CSF leak with the endoscopic and transfrontal approaches. The overall rates of CSF leak were lower than those typically reported in the literature, with 8.00% with the endoscopic approach and 10.3% with the transfrontal approach and were statistically significant (P<0>
In our analysis, after adjusting for age, sex, race, and CCI, we discovered that a BMI over 25 independently predicted an increased likelihood of pulmonary, renal, and hemorrhagic complications. This aligns with existing research indicating that obese individuals are at a heightened risk for various postoperative complications and hospital readmissions when compared to their non-obese counterparts [12, 13]. The elevated complication rates in obese patients have been attributed to both surgical and medical challenges [14, 15]. Specifically, studies have reported CSF leak rates exceeding 10% in obese patients [14, 15], a stark contrast to the 1.3% to 1.7% range observed in non-obese individuals [16, 17]. Moreover, medical issues like pneumonia contribute to the overall higher complication rates seen in the obese population [13], underscoring the complex interplay between obesity and postoperative health outcomes.
Our study is subject to several limitations that merit consideration. Firstly, the transition from ICD-9 to ICD-10 coding systems introduced significant changes. Additionally, the inconsistency in recording obesity before 2016 posed challenges in accurately assessing its impact on surgical outcomes. Despite these challenges, our results align with existing literature, underscoring their relevance. However, it's important to highlight that the database does not provide information on radiographic tumor characteristics, which means that patients predisposed to higher complication risks, possibly due to larger tumor sizes, cannot be distinctly identified through this analysis.
Despite advancements in endoscopic endonasal pituitary surgery, its access and utilization remain uneven across different populations, highlighting persistent disparities in healthcare access and outcomes influenced by socioeconomic factors, race, and ethnicity. Racial and ethnic minorities, in particular, experience higher rates of complications from such surgeries. The root causes behind these disparities are complex and multifaceted, with socioeconomic determinants of health playing a crucial role in these variations, thereby presenting numerous opportunities for in-depth research. It raises the question of whether these disparities stem from differing perceptions and acceptance of pituitary surgery among various racial groups, potentially with some groups more hesitant to undergo surgery, or if they are attributable to variations in access to healthcare financing and specialized care facilities capable of performing such surgeries. Additionally, the observed higher incidence of stroke and other comorbid conditions within the Black population might contribute to more incidental findings of pituitary issues and subsequently poorer postoperative outcomes, further complicating the landscape of healthcare equity in the context of pituitary surgery.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.
