AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2641-0419/391
1Department of Cardiology, Mody Harvard Cardiac Institute & Research Centre- Krishna Super Specialty Hospital, Bathinda, Punjab, India. ORCID: 0000-0001-8977-5803.
2Department of Cardiology, Aster Hospital, Mankhool, Dubai, Al Quasis, UAE. ORCID: 0000-0003-1354-3808.
3Department of Medicine, Kasturba Medical College, Manipal, Karnataka, India. ORCID: 0000-0001-8944-9418.
4Department of Cardiology, Dr Asha Memorial Multispecialty Hospital, Fatehabad, Haryana, India. ORCID: 0009-0006-4702-5995.
5Department of Medicine, Government Medical College and Rajindra Hospital, Patiala, Punjab, India. ORCID: 0000-0009-2387-330X
6Department of Medicine, Extern, Internal Medicine, Medstar Franklin Square Medical Centre, Baltimore, USA. ORCID: 0009-0005-4510-2910.
7Department of Cardiology, Mody Harvard Cardiac Institute & Research Centre- Krishna Super Specialty Hospital, Bathinda, Punjab, India. ORCID: 0009-0006-4956-9013.
*Corresponding Author: Rohit Mody, Department of Cardiology, Mody Harvard Cardiac Institute & Research Centre- Krishna Super Specialty Hospital, Bathinda, Punjab, India. ORCID: 0000-0001-8977-5803.
Citation: Rohit Mody, Debabrata Dash, Bhavya Mody, Amit Munjal, Bankey Bihari, et al, (2024), Vulnerable Plaque: What the Future Holds?, J Clinical Cardiology and Cardiovascular Interventions, 7(8); DOI: 10.31579/2641-0419/391
Copyright: © 2024, Rohit Mody. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 02 July 2024 | Accepted: 19 July 2024 | Published: 26 July 2024
Keywords: fibroatheromatous plaques; optical coherence tomography; intravascular ultrasonography; near-infrared spectroscopy; pet imaging; ct angiography
Background: The concept of vulnerable plaque has gained prominence over the past four decades. Extensive research into the pathophysiology of these plaques has been quite beneficial in assessing an individual susceptibility to cardiovascular events. Understanding the occurrence of cardiovascular events is crucial.
Main Body: Vulnerable Plaque rupture along with plaque erosion contribute to acute coronary syndrome in over half of patients. The primary objective of this discussion is to demonstrate recent research findings on various diagnostic methods for the early detection, prevention, and treatment of patients at high risk of developing vulnerable plaques. Current studies and research are focused on various future imaging techniques that can detect this specific plaque pathophysiology. Identifying patients prone to vulnerability and implementing more intensive treatments for coronary atherosclerosis are key areas of ongoing investigation.
Short conclusion: Plaques which are more vulnerable to rupture causing MACE can be identified with the evolution of new non-imaging and imaging modalities to prevent risk of CAD.
1.ACS: Acute Coronary Syndrome
2.CAC: Coronary Artery Calcium
3.CAD: Coronary Artery Disease
4.CAG: Coronary Angiography
5.CCTA: Coronary Computed Tomography Angiography
6.CIMT: Carotid Intima-Media Thickness
7.CN: Calcified Nodule
8.CRP: Complement Reactive Protein
9.CT: Computed Tomography
10.CTCAC: Computed Tomography Coronary Artery Calcium
11.CTP: Cardiac Tomography Perfusion
12.CVD: Cardiovascular Disease
13.ECG: Electrocardiogram
14.ESS: Endothelial Shear Stress
15.FDG: fluorodeoxyglucose
16.FFR: Fractional Flow Reserve
17.IL-18: Interleukin-18
18.IVUS: Intravascular Ultrasound
19.IVUS: Intravascular Ultrasound
20.LAD: Left Anterior Descending artery
21.MACE: Major Adverse Cardiac Event
22.MI: Myocardial Infarction
23.MPIO: Microparticles of Iron Oxide
24.MRI: Magnetic Resonance Imaging
25.NIRAF: Near-Infrared Autofluorescence
26.NIRF: Near-Infrared Fluorescence
27.NIRS: Near-Infrared Spectroscopy
28.NSTEMI: Non-ST-Elevation Myocardial Infarction
29.OCT: Optical Coherence Tomography
30.PCS: Protein Convertase Subtilisin/Kexin
31.PET/CT: Positron Emission Tomography/Computed Tomography
32.PET: Positron Emission Tomography
33.pFAI: perivascular Fat Attenuation Index
34.PRS: Polygenic Risk Score
35.PVAT: Perivascular Adipose Tissue
36.SCD: Sudden Cardiac Death
37.S-CMR: Stress-Cardiac Magnetic Resonance
38.SOCT: Saline Optical Coherence Tomography
39.STEMI: ST-Elevation Myocardial Infarction
40.TCFA: Thin Cap Fibroatheroma
41.VCAM: Vascular Cell Adhesion Molecules
42.VH-IVUS: Virtual Histology-Intravascular Ultrasound
43.VI: Vulnerability Index
44.μOCT: Micro-Optical Coherence Tomography
Recent advancements have led to a significant decrease in deaths from coronary artery disease (CAD), the leading global cause of death, largely attributed to sedentary lifestyles. Historically, intravascular ultrasound (IVUS) was utilized to determine the morphology and characteristics of these lesions (plaques), and their potential impact on future cardiovascular events. However, studies on newer imaging techniques have raised concerns regarding the detection and progression of lesions that could lead to cardiovascular events [1]. Researchers now advocate for more accurate risk stratification and identification of high-risk patients. Another research direction involves developing more advanced in vivo imaging techniques to understand plaque pathogenesis and physiology. This article will discuss various invasive and non-invasive imaging methods to diagnose plaque burden and future imaging techniques for predicting future cardiovascular events.
The concept of plaque burden and increased thrombosis associated with plaque began in the early 1990s. This concept has now evolved to focus on vulnerable plaque and patients [1]. Even asymptomatic plaque can rupture, becoming vulnerable and leading to cardiovascular events or CAD. Major adverse cardiac events (MACE) are often the result of vulnerable plaque. Imaging studies have demonstrated that the morphological characteristics and features of atherosclerotic plaque change over time, particularly with the use of high-intensity statin therapy. In patients with stable conditions, most plaque erosions and ruptures remain clinically silent, and current imaging diagnostics methods provide limited evidence of plaque burden.
Main Text
Pathology
The formation of atherosclerotic plaque involves complex cellular interactions among various cells, including endothelial cells, smooth muscle cells, and immune system cells. Key processes in this formation are the retention of lipoproteins, recruitment of inflammatory cells, foam cells formation, apoptosis, necrosis, proliferation of smooth muscle cells, matrix synthesis, calcification, angiogenesis and arterial remodeling. As the plaque develops, it typically forms an atheroma characterized by a weak, soft, and highly thrombogenic structure, with a fibrous cap enclosing a core of extracellular lipids and debris. While most atherosclerotic plaques remain asymptomatic (subclinical disease), some become obstructive (causing stable angina), and others can precipitate acute thrombosis, leading to acute coronary syndrome (ACS) events [2]. Among young individuals, prevalence of ACS is rising, but clinical outcomes, causes and phenotypic characteristics have not been well demonstrated. Findings of study conducted among 8712 patients present with ACS demonstrated that atherosclerosis was the major prominent cause of ACS (86.5%), followed by coronary artery embolism (9%) and spontaneous coronary artery dissection (4.5%) [3]. Further, with the aim to demonstrate the association of distinct metabolic phenotypes with MACE and CAD, PROMISE (Prospective Multicenter Imaging study for Evaluation of Chest pain) was conducted in 4381 patients present with stable chest pain who underwent coronary computed coronary angiography. Findings of study proposed that metabolic phenotypes, including diabetes, hypertension, hyperlipidemia and obesity exhibit distinctly different CAD characteristics and risk for MACE [4].
Healed coronary plaques, signs of previous destabilization of coronary plaques can be identified by using Optical coherence tomography (OCT). In more than >50% of patients present with stable angina pectoris, healed plaques at the culprit lesions were seen. More complex angiographic features and multivessel disease features aree present in patients with healed culprit plaques, have huge degree of stenosis and greater vulnerability at the culprit lesion. Further, findings of study conducted on 163 patients in patients present with chronic stable angina, demonstrated that healed culprit plaque are more common in these patients and are associated with signs of advanced atherosclerosis and pan vascular vulnerability [5]. With the objective to demonstrate the morphological characteristics, clinical significance and prevalence of healed culprit plaques in patients present with ACS by using OCT, a study was conducted on 376 ACS patients present with STEMI and 124 patients with non-STEMI. Findings of study suggested that at culprit sites, healed plaques were present in more than one-quarter of ACS patients. More frequently, these patients were present with previous history of MI, were seen diabetic and hyperlipidaemic. Furthermore, more frequent OCT features of Vulnerability with evidence of systemic and local inflammation was observed in these healed plaques [6].
Local factors such as inflammation and matrix turnover contribute to changes in the plaque. The coagulation system also plays a role in plaque rupture, further aggravated by inflammatory mediators like vascular cell adhesion molecules (VCAM) and chemokine receptor-2 expression. Matrix turnover, a secondary growth factor, accelerates plaque rupture progression. The expression of tumor necrosis growth factor-β, which influences collagen synthesis, is amplified near atherosclerotic lesions. Plaque rupture is a leading cause of thrombosis which occurs where the fibrous cap is thinnest, infiltrated by various foam cells (macrophages). Two primary pathophysiological mechanisms contribute to fibrous cap thinning: gradual loss of smooth muscle cells from the cap and degradation of the collagen-rich cap matrix by infiltrated macrophages [7].
Biochemical and genetic markers assist in assessing cardiovascular event risks and plaque vulnerability. Complement reactive protein (CRP) is considered a predictor of atherosclerotic disease progression, although the Dallas study [8] questioned its accuracy [9]. Cytokines like Interleukin-18 (IL-18) are implicated in atheroma development and linked to cardiovascular events. The Copenhagen heart study associated high fibrinogen levels with advanced atherosclerosis but not specifically with plaque rupture [10]. The biomarker suppression of tumorigenicity-2 (sST-2) indicates prognosis in heart failure and myocardial infarction (MI) patients, with elevated levels suggesting higher mortality. Elevated levels of pregnancy-associated plasma protein-A and myeloperoxidase indicate increased risks of plaque rupture in CAD patients, though their clinical application is limited. Global study of these markers may not directly indicate plaque instability but can improve understanding of CAD risk stratification. Additional markers like CRP, fibrinogen, and white blood cell counts correlate with higher CAD risks, particularly in younger demographics. Integrating these markers with conventional risk factors enhances CAD risk predictions. Emerging biomarkers like lipoprotein-associated phospholipase-A2 and myeloperoxidase are becoming important indicators for young CAD patients [11]. Circulating proteins, such as oxidation and inflammation biomarkers, are crucial to atherosclerosis. Key biomarkers, including insulin and tumor necrosis factor-alpha, show strong associations with CAD. The polygenic risk score (PRS) is effective in predicting CAD risks, especially among young individuals with a family history of premature CAD, as emphasized by Khera and colleagues [12]. Table 1 presents immune and metabolic disorders as reflected by serological indicators of plaque vulnerability.
| Serological Markers of Vulnerability Reflecting Metabolic and Immune Disorders |
|
| Serological Markers of Vulnerability Reflecting Hypercoagulability |
|
Table 1: Serological Markers of Vulnerability Reflecting Metabolic and Immune Disorders
† LDL = Low-Density Lipoprotein; HDL = High-Density Lipoprotein; hsCRP = High-Sensitivity C-Reactive Protein; IL = Interleukin; ICAM = Intercellular Adhesion Molecule; VCAM = Vascular Cellular Adhesion Molecule; HSP = Henoch-Schonlein Purpura; PAPP-A = Pregnancy Associated Plasma Protein-A; ADMA = Asymmetric Dimethylarginine; DDAH = Dimethylarginine Dimethylaminohydrolase; NEFA = Nonesterified Fatty Acids.
Luminal Thrombosis and Acute Coronary Syndrome
Patients experiencing ACS often present a range of symptoms, from severe chest pain and electrocardiogram (ECG) changes to acute MI or sudden cardiac death (SCD). In more than half of these cases, an acute thrombus is prominently visible in the affected vessel, whereas other vessels may show stable plaques. Significantly, over half of these fatal cases had a pre-existing vulnerable plaque that ruptured, causing thrombotic occlusion. The degree of vessel narrowing due to the plaque and its morphological characteristics play a crucial role in determining the likelihood of future cardiac events. Figure 1(A), 1(B), and 1(C) illustrate the differences between stable and unstable plaques. Pathological and imaging studies have identified that plaque erosion and rupture are key factors in the development of ACS and SCD. Advanced imaging techniques have shown that many destabilized atherosclerotic plaques do not lead to clinical syndromes, implying a reduced risk of SCD. The destabilization of a plaque is largely influenced by the balance between thrombosis-resisting and prothrombotic factors. In some cases, distorted or eroded plaques may be indicative of an interrupted ACS event [13].

(A) Histological studies of Stable and unstable plaque characteristics (B) IVUS examination of Stable and unstable plaque characteristics (C) Virtual histological examination of stable and unstable plaque characteristics which involve Classification of plaque by using intravascular ultrasound method-Difference between intimal thickening (a, b) and more vulnerable lesions such as fibroatheroma (c, d, e) is carried out by virtual histology. Presence of necrotic core on plaque surface is seen in thin cap fibroatheroma (TCFA) (d) in comparison to the fibroatheroma (c), where presence of fibrous cap is not seen. Presence of multiple previous ruptures is suggested by TCFA with necrotic area (e) multiple layers. (a) Adaptive thickening of intimal layer (b) intimal thickening in pathological manner. (c) Fibroatheroma (d) TCFA defined by IVUS (e) TCFA, multiple layers (f) fibro calcific plaque.
†IVUS: Intravascular Ultrasound; TCFA: Thin Cap Fibroatheroma.
Figure 1: Studies of Stable and unstable plaque characteristics.
(A) Histological studies of Stable and unstable plaque characteristics (B) IVUS examination of Stable and unstable plaque characteristics (C) Virtual histological examination of stable and unstable plaque characteristics which involve Classification of plaque by using intravascular ultrasound method-Difference between intimal thickening (a, b) and more vulnerable lesions such as fibroatheroma (c, d, e) is carried out by virtual histology. Presence of necrotic core on plaque surface is seen in thin cap fibroatheroma (TCFA) (d) in comparison to the fibroatheroma (c), where presence of fibrous cap is not seen. Presence of multiple previous ruptures is suggested by TCFA with necrotic area (e) multiple layers. (a) Adaptive thickening of intimal layer (b) intimal thickening in pathological manner. (c) Fibroatheroma (d) TCFA defined by IVUS (e) TCFA, multiple layers (f) fibro calcific plaque.
†IVUS: Intravascular Ultrasound; TCFA: Thin Cap Fibroatheroma.
Three different plaque morphologies are:-
1) Plaque ruptures 2) Plaque erosion and 3) Calcified nodule (CN)
Other morphologies can be
1) Intraplaque hemorrhage, 2) Thin fibrous plaque, and 3) necrotic core rich in lipid content
Plaque Rupture (“50 to 60%” Events)
Plaque rupture is a process where inflammatory cells infiltrate a lipid-rich lesion, covered by a fragile fibrous layer. The exact cause of the cap disintegration is unclear, but when it contacts blood, it can trigger thrombosis, involving platelets and the lipid core [14]. Blood cells, particularly macrophages and lymphocytes, play a significant role in thrombus formation. The occurrence of plaque rupture varies by gender and age: it's more common in men in their 40s, but the rates become similar for men and women in their 50s. Thin cap fibroatheroma (TCFA) is a crucial biomarker for plaque rupture [7].
Recent studies indicate a decrease in cardiovascular deaths among women. However, the differences in incidence of ACS between genders remain not fully understood [15]. An OCT study conducted to assess plaque characteristics in male and female patients present with CAD demonstrated that, despite higher risk in men, women exhibited a lower plaque lipid index [16]. Long-term comprehensive studies are necessary to fully understand these gender-based differences.
Plaque Erosion (22–25% Events)
Plaque erosion occurs when the plaque makes direct contact with the intimal layer and has a denuded endothelium [17], leading to thrombus formation. Eroded lesions typically have a thick fibrous cap and are associated with fewer cardiovascular events compared to ruptured plaques. About 20-25% of myocardial events stem from plaque erosions, with a higher incidence in women. Autopsy studies indicate that 80% of thrombi from erosions exhibit delayed healing, as opposed to 50% in ruptured plaques [18].
Calcified Nodule (2–7% Events)
CN is a relatively rare cause of cardiovascular events, primarily consisting of calcium deposits.
From Vulnerable Plaque to Vulnerable patients
Ruptured plaques are significant contributors to MI and strokes. Vulnerable plaques, characterized by large lipid cores and thin fibrous caps, can abruptly rupture, transitioning from stable to symptomatic. They are responsible for 60-70% of cardiac events. While both erosion and rupture in plaques can lead to coronary events, 75% result from ruptures in thin-cap plaques. Ruptured plaques induce more luminal narrowing than eroded ones. There has been growing evidence that some atherosclerotic plaque specific features, which increase the susceptibility of plaque to trigger thrombotic events, as far more clinically significant than lumen occlusion level or absolute size. In the past 30 years, since the vulnerable plaque term was being introduced, various advancements have been made in the understanding of pathophysiology and pathogenesis of plaque, shifting from specific lesion pursing morphological features of ‘vulnerability’ to more specific goal of assessment of cardiovascular vulnerability of patient or Vulnerable patients [19]. In the past three decades, major focus on vulnerable plaque [20,21] has shifted into a broader topic vulnerable patient [22,23] and concept of plaque as the current findings proposed that on clinical level, rupturing of silent plaque may occur and coexistence of vulnerable plaques in a vulnerable patient is required to generate acute coronary events. Positron emission tomography (PET), IVUS, OCT and near-infrared spectroscopy (NIRS) can be used for the assessment of vulnerable plaques and vulnerable patients. Multiple plaques can develop in vulnerable patients with vulnerable characteristics in comparison to those without and so there is requirement of more aggressive therapeutic strategies at an earlier stage of disease [24].
Imaging Biomarkers for Vulnerable Plaque
A range of techniques, including computed tomography (CT), OCT, IVUS, magnetic resonance imaging (MRI), spectroscopy, and halography, are employed to accurately depict the structure and vulnerability of plaques. The primary aim of these techniques is the early identification and management of vulnerable plaques. The ISCHEMIA trial, which included 5,179 patients with stable CAD, revealed that not all atherosclerotic areas in the coronary arteries lead to adverse cardiovascular events. Many plaques have heterogeneous regions with a high potential for destabilization, yet they do not necessarily cause destruction [25].
Plaque Rupture Prediction and Challenges
Over 70% of cardiovascular events are due to plaque erosion and rupture. Research studies often focus on plaque characteristics such as morphology, cap thickness, and hemorrhage. Interestingly, it's not only the vulnerable plaques but also the stable ones that can rupture, contributing to half of all cardiovascular events [26]. Atherosclerotic plaque ruptures account for about 70% of all MI’s and 15% of all ischemic strokes. Experimental and imaging studies often examine the balance between stabilizing and destabilizing components within atherosclerotic plaques to identify those prone to rupture. However, there is a lack of strong evidence supporting the potential of this balance to predict future adverse cardiovascular events. A study involving clinical data and carotid plaques from 194 patients aimed to determine if a calculated histological ratio, known as the vulnerability index (VI), could assess the risk of future cardiovascular events. The study's findings suggested a significantly increased risk of future adverse cardiovascular events in patients with a high VI, even in the absence of other known cardiovascular risk factors and symptoms. This underscores the potential of imaging methods capable of assessing such plaques in enhancing risk stratification and identifying patients who require more intensive treatment [27]. Plaques with caps thinner than 65 micrometers and a necrotic core are considered as high-risk plaques. Traditional imaging methods often fall short in detecting these features; hence, stress calculations might offer deeper insights. There is a growing demand for improved non-invasive and intravascular imaging techniques to study high-risk plaques, which would enhance understanding of plaque evolution.
Assessment of Plaque Vulnerability by Computed Tomography Coronary Angiography
Coronary computed tomography angiography (CCTA) offers diagnostic insights, especially regarding potential issues in the left anterior descending artery (LAD). Enhanced by electrocardiography, CCTA ensures low-dose imaging, effectively ruling out obstructive coronary atherosclerosis in suspected angina cases. However, its accuracy may be compromised by factors such as calcification, stent presence, and motion artifacts. ECG, coronary angiography (CAG), and CT angiography of a patient demonstrating prediction of major cardiovascular events are shown in figure 2(i), 2(ii), and 2(iii), illustrating the importance of CT imaging and transverse T1-weighted MR in assessing disease progression. The SCOT-HEART Trial underscored CCTA's effectiveness in diagnosing stable angina, resulting in fewer adverse cardiovascular outcomes [28]. The CARDIA study established a significant association between plaque burden and coronary artery calcification (CAC), indicating that elevated CAC levels are linked with increased risks of CAD and cardiovascular disease (CVD) [29]. By 2019, the European Society of Cardiology had endorsed CCTA for suspected stable angina cases [30]. Although IVUS was once considered the gold standard, CCTA now provides enhanced plaque characterization [31]. Studies like SCOT-Heart and PROMISE have associated high-risk plaques with more CAD deaths. The PARADIGM study demonstrated a 35% reduction in atherosclerosis progression and plaque formation with statin therapy [32].

Figure 2: Assessment of disease activity, CT imaging and transverse T1 weighed -MR of atherosclerotic rabbit abdominal aorta.
†ECG: Electrocardiogram; MI: Myocardial Infarction; CT: Computed Tomography; PET: Positron Emission Tomography; FDG: Fluorodeoxyglucose.

Figure 3: MRI capabilities in plaque vulnerability identification.
(A) MRI with the use of labelling substance Gadolinium chelates (B) MRI with the use of labelling substance Iron oxide (C) MRI with the use of labelling substance Dual ligand MPIO (D) MRI with the use of labelling substance Dense-dual targeted MPIO binding (E) MRI with the use of labelling substance Aortic roots ex-vivo MPIO (F) Dual-targeted MPIO 3D reconstruction (G) Smaller size of MPIO demonstrated by Histological screen imaging. (H) Retention of MPIO by lungs (I) Biodegradable MPIO Biological handling properties Schematic representation (J) (a to d) Biodegradable MPIO Biological handling.
†MRI: Magnetic Resonance Imaging; MPIO: Microparticles of Iron Oxide; LIBS: ligand induced binding sites.
Atherosclerosis Imaging in Stable Coronary Disease by Non-Invasive Imaging Modalities
Non-invasive imaging techniques, such as computed tomography coronary artery calcium (CTCAC), CCTA, biomarkers of inflammation and oxidation, Carotid intima-media thickness (CIMT), and the perivascular fat attenuation index (pFAI), provide early diagnostic insights for patients with asymptomatic spontaneous CAD. These techniques enhance the evaluation of CAD risk and guide therapeutic approaches.
While CAC scoring is valuable for predicting cardiovascular events, CCTA offers detailed imaging of atherosclerotic plaques, including the severity of stenosis and the differentiation between calcified and non-calcified plaques. CIMT, measured via ultrasound, serves as a predictive indicator of atherosclerosis [33].
CCTA stands out as a potent imaging modality for monitoring the progression of CAD, particularly in tracking the calcification of atherosclerotic plaques. With advancements in technology, CCTA has become crucial in evaluating CAD. It enables the analysis of plaque characteristics, predicting growth, the likelihood of rupture, and ischemia. CCTA distinguishes itself by detailing the severity of stenosis, analyzing plaque composition, and differentiating types of plaques, thereby optimizing the understanding of patient responses to CAD treatments. It facilitates the tracking of the evolution of atherosclerotic lesions from early stages to high-risk, rupture-prone lesions, such as TCFA [34]. These TCFAs, considered high-risk, are vital for assessing prognosis and determining the risks of plaque rupture. Furthermore, CCTA was demonstrated to be a promising diagnostic method for assessment of CAD in low-risk patients who present with chest pain to the emergency room, leading additional to reduced length of stay [35]. Risk for long-term coronary death or MI reduced with the addition of CCTA, as CCTA increased sensitivity for the coronary atherosclerosis assessment led to higher rate of initiation of guideline-directed preventive therapy. Moreover, CCTA can detect inflammation-induced changes in atherosclerotic plaques within coronary arteries [36]. Moreover, CCTA can detect inflammation-induced changes in atherosclerotic plaques within coronary arteries [37]. Contemporary studies correlate CCTA-derived plaque features with fractional flow reserve (FFR) and myocardial perfusion, highlighting CCTA's diagnostic strength. For asymptomatic patients, CCTA's ability to evaluate CAC is particularly notable, as it can predict sudden cardiac arrests. While CAC imaging is less invasive than CCTA, its limitations, especially in patients with MI symptoms, restrict its use. However, innovations such as pFAI provide automated tools for assessing risky atherosclerotic plaques [38].
Various studies underscore CCTA's superiority in predicting CAD, emphasizing its advantage over traditional diagnostic methods. CCTA's technological advancements have improved its resolution and acquisition quality, though it requires time and expert analysis. Initial concerns about radiation exposure during CCTA, due to potential cancer risks, have been mitigated by recent developments that minimize radiation dosages. Novel imaging markers from CCTA, like pFAI, enable the visualization and quantification of coronary artery inflammation, predicting potential cardiac threats [39]. The cardiac-CT angiography pFAI evaluates the quality of perivascular adipose tissue (PVAT) surrounding coronary arteries; a lower pFAI indicates increased PVAT inflammation.
Advancements in CCTA also allow for the non-invasive evaluation of vulnerable plaques. Potential role of CCTA in the assessment of vulnerable plaque has been investigated by various studies i.e. sites of coronary atherosclerosis that would be linked with a much huge risk of thrombotic events and plaque rupture. However today, major focus has switched to the detection of vulnerable patients, investigation of plaques with high-risk remains important. Finally, in understanding the role played by PVAT in atherosclerosis, CCTA has recently played major role and also how as a novel prognostic index of adverse coronary outcomes, pericoronary inflammation can be used. Studies highlight specific high-risk plaque characteristics in ACS patients. The SCOT-HEART Trial identified high-risk atherosclerotic plaques as a factor in elevating CAD risks, with CCTA being effective in quantifying diverse vessel risk traits and identifying potential high-risk patients. Emerging CCTA technologies, combined with stress-CT perfusion, provide improved diagnostic accuracy in identifying functionally significant stenosis [40]. Computational fluid dynamics, exemplified by wall shear stress, aid in identifying high-risk plaques. While these new technologies enhance CCTA's prognostic value, further clinical trials are necessary to solidify its evidence-based utility.
The limited potential of CCTA in assessing hemodynamically significant coronary artery stenosis has led to the development of additional functional tests, such as stress-cardiac magnetic resonance (S-CMR) and cardiac tomography perfusion (CTP). S-CMR, a non-ionizing diagnostic method, assesses motion abnormalities in the ischemic wall or detects perfusion defects typically induced by exercise or pharmacological stress. Studies have demonstrated the marked diagnostic accuracy and high negative predictive value of S-CMR compared to other gold standard imaging methods, including FFR and angiographically determined luminal coronary stenosis. CTP, another non-invasive diagnostic method, requires the administration of a stress agent followed by a CT acquisition to assess myocardial ischemia over coronary anatomy and plaque stenosis. Past studies have shown that the diagnostic efficacy of CCTA is increased when used in conjunction with stress CTP [41].
Vulnerable plaques, precursors to acute coronary events, can be identified through both invasive and non-invasive imaging modalities. PET and CCTA are modern tools [42] in this regard. Ultrasound, particularly contrast-enhanced and Color Doppler variants, is also effective, especially for carotid arteries. The role of MRI in assessing atherosclerotic plaques is increasing. A study involving 191 patients linked high-risk plaques with type-2 diabetes, regardless of other factors, demonstrating MRI's risk stratification capability for diabetes [43]. Advancements in MRI include the use of gadolinium chelates for enhanced contrast and iron oxide with polymer shells for increased precision. Notably, Dual-microparticles of iron oxide (MPIO) targeting VCAM-1 and P-selectin provide sharper images of aortic plaques. Their safe removal and iron handling reduce side effects. Figures 4 (A to J) further illustrate MRI's capabilities in identifying plaque vulnerability.

Figure 4: Coronary Tree FDG uptake representative images with corresponding angiographic images and vulnerable plaque features by ultrasound method.
Based on hemodynamic indices and characterization of plaque, CCTA emerging applications may provide personalized assessment of risk, impact detection of disease and can guide about future therapy. Plaques present with huge-risk are clinically significant and markers of vulnerable, lesions prone to rupture. Findings of SCOT-HEART trial provide evidence that high risk of nonfatal MI or coronary heart disease is present in patients with one or more features of LAP or positively remodelled coronary segments [40]. Motayama et al. demonstrated that alongside high-risk plaque characteristics, when additional features such as plaque development and significant stenosis are investigated, cardiovascular event rate was huge in patients with progressive high-risk or stenotic plaques in comparison to the non-progressive and non-stenotic high-risk plaques, thus adding to these characteristics prognostic value [44]. In combination with evaluation of characteristics of plaque, assessment of high-risk features by using quantitative CCTA has also been used to assess patients at huge-risk specifically since evolution of plaques at huge-risk over time. In the CT (ICONIC) study used to assess incidence of coronary events, CCTA was utilized to compare 234 patients were compared who developed ACS to paired control patients who developed ACS. While multivariable predictor of AMI in the ACS group was percent diameter stenosis, at the time of CCTA, maximal %DS <50>
Assessment of Disease Progression by Coronary Positron Emission Tomography-Computed Tomography (PET/CT)
Imaging of heart cellular functioning is provided by PET and PET/CT which are emerged as encouraging precise non-invasive diagnostic methods while other non-invasive cardiovascular imaging methods are majorly used for imaging the tissue characteristics, function, structure, morphology and anatomy. Imaging with hybrid PET/CT has led to marked improvements in chronic CAD dysfunctional areas characterization and simultaneous integration of myocardial perfusion with coronary anatomy. Earlier, for the assessment of myocardium viability, PET has been widely used but nowadays it is popularly used for the investigation of flow-limiting CAD. Diagnosis and prognostication of suspected CAD patients has been facilitated by PET, while stratification is facilitated by this technique in patients present with known ischemic myocardial dysfunctioning [48]. Furthermore, asymptomatic CAD and symptomatic CAD at early stages can be predicted with use of PER investigating an absolute MBF in millilitres per gram per minute [49]. Over the last several years, there has been a consistent progress in combination of CT with PET. In suspected CAD patients, benefit of PET/CT has been investigated by various studies. In the PET/CT assessment of 24 patients, better understanding of coronary stenosis hemodynamic significance has been demonstrated by Valenta et.al [50]. Further, a study was designed by Dey et.al in 51 patients in which PET/CT hybrid examination was caried out in which myocardial flow reserved obtained from rest-stress 13N-ammonia PET was combined with CTCA [51]. In comparison to the use of PET or CTCA alone, both studies provide marked evidence of better prediction of hemodynamically significant coronary stenosis in comparison to the alone use of PET or CTCA. For the evaluation of the pathophysiological mechanism of atherosclerosis, radiotracers employed by PET/CT which is now utilized in several cardiovascular molecular imaging modalities. Because of the small size of coronaries and continuous motion, post-process optimal reconstructive interpretation of coronary activities was designed to obtain molecular imaging [52]. Furthermore, Management strategy in patients present with CAD can be guided by PET/CT while coronary stenoses can be assessed by CT, PET-CT van be utilized to assess whether they are clinically significant or flow-limiting.
Two Radiotracers are studied:
1.18F
2.8F- GP1
18F-FLUORIDE
18-F Sodium Fluoride (18-F Fluoride) is a radiotracer used to detect coronary artery microcalcification due to its distinct epicardial artery signals and minimal myocardium activity. As calcium increases, 18-F binding grows, facilitating early microcalcification identification [53], which can jeopardize fibrous cap stability.
18F-GP1
18F-GP1 is an innovative imaging method for coronary thrombus. When plaques rupture, they stimulate platelet activation, leading to thrombus creation, with GP2b/3a playing a central role.. Notably, 18F-GPI binds to GP2b/3a despite the presence of other anticoagulants [54]. Kim et al. highlighted 18F-GP1's safety and unique diagnostic potential in coronary atherosclerosis, but its full use requires PET-CT. In related research, animals given iodine-based N1777 and F-labeled fluorodeoxyglucose (FDG) underwent imaging tests, revealing lipid-rich plaques [55]. A particular diet helped reduce myocardial uptake during imaging. Figures 4(I) and 5(II) emphasize PET/CT' and Ultrasound importance in monitoring disease development.
Invasive Imaging modalities are-
1.IVUS
2.OCT
3.NIRS
OCT's advantage lies in its exceptional resolution, crucial for examining fibrous caps overlying necrotic cores. Advanced OCT versions, such as saline optical coherence tomography (SOCT), near-infrared autofluorescence (NIRAF), near-infrared fluorescence (NIRF), and NIRS, are paving the way for more sophisticated future plaque imaging. OCT and angioscopy studies on patients with ACS have provided detailed insights into lipid pools and fibrous caps. In these patients, corresponding OCT and angioscopic images were obtained. These images use color gradations– white [Figure 5(B) (a-1)], light yellow [Figure 5(B) (b-1)], yellow [Figure 5(B) (c-1)], and intense yellow [Figure 5(D) (d-1)] – for plaque grading. Areas with poor signal in OCT images [figure 5(B) (a-2, b-2, c-2, d-2)] are used to characterize lipid pools (*). The evaluation of the fibrous cap is carried out in the signal-rich region between the coronary artery lumen and the inner border of the lipid pool in OCT images, with its thinnest part’s thickness being measured [Figure 5(B) (a-3, b-3, c-3, d-3)]. In IVUS [Figure 6(i)], vulnerable plaques are marked (Arrow), alongside an elastogram. In the elastogram, high surface strain indicates the presence of highly vulnerable plaques.

Figure 5: IVUS imaging of atherosclerotic plaque and OCT imaging in patients having acute coronary syndrome.
A. Representative IVUS Image of Vulnerable Atherosclerotic Plaque from proximal area to distal area and corresponding.
(i) IVUS images of vulnerable plaque.
(a) Mild concentric lesion
(b) Eccentric lesion with an echolucent area.
(c) Eccentric lesion with high echogenic density.
(ii) From proximal area to distal area, four cross sectional images were obtained.
(a) Thick fibrous cap overlying a necrotic core can be seen
(b) Another thick fibroatheroma
(c) Minimal lumen diameter site
(d) Thin-cap fibroatheroma
B. Corresponding and OCT imaging done in patients having acute coronary syndrome.
a-1- White
b-1- Light Yellow
c-1- Yellow
d-1- Intensive Yellow
With the objective of plaque grading, in the angioscopic images various color used were White (a-1), light Yellow (b-1), yellow (c-1) or Intensive yellow (d-1). Lipid pool was identified as the poor region signal and further, optical coherence tomography image (a2, b2, c2, d2) was identified in cross sectional manner. Further, for the semi quantification, numbers of quadrants involved were used. In the imaging by OCT method, identification of signal rich region of fibrous cap was carried out in between the coronary artery lumen and lipid pool border and further, thickness was measured at the thinnest part (a3, b3, c3, d3, arrows).
†IVUS: Intravascular Ultrasound; OCT: Optical Coherence Tomography.
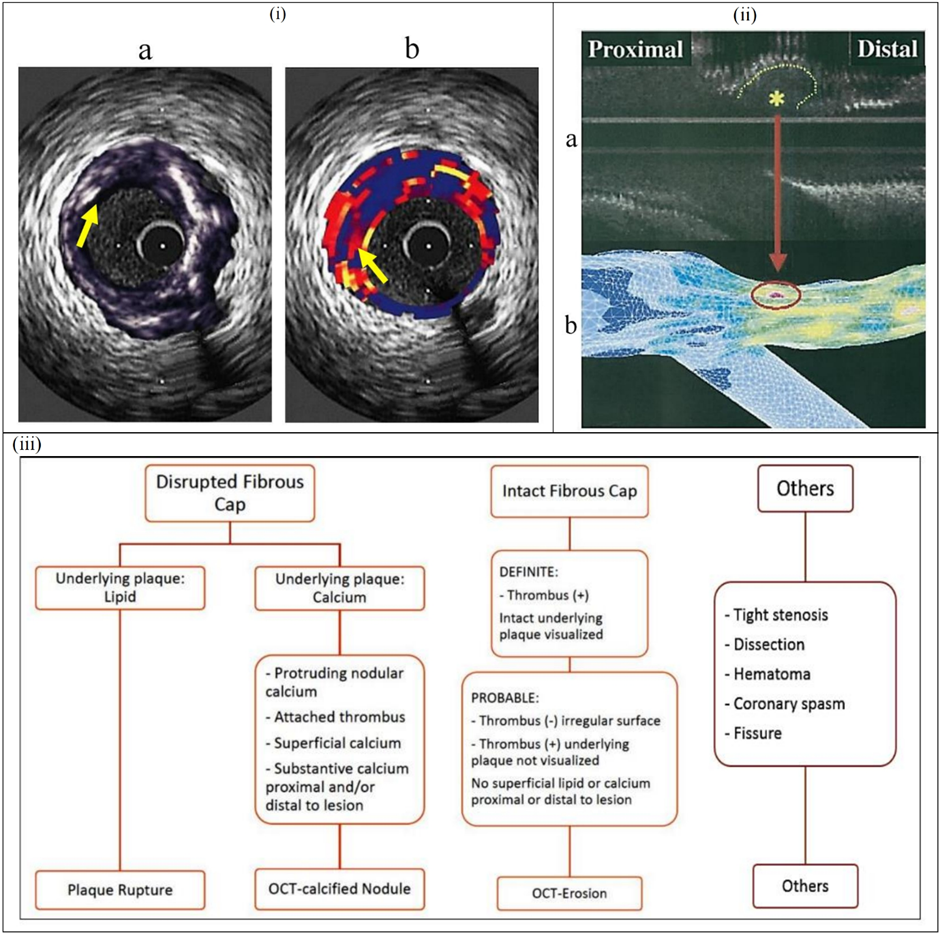
Figure 6: Histological, IVUS examination, LAD color mapping and plaque classification algorithm.
a. Histological and IVUS assessment
i. Intravascular Ultrasound
ii. Elastogram
b. In the LAD color mapping of Shear stress distribution
i. Color Mapping of the Shear Stress
ii. Distribution in the LAD.
c. Plaque classification algorithm by OCT.
†IVUS: Intravascular Ultrasound; LAD: Left Anterior Descending artery; OCT: Optical Coherence Tomography.
Elastograms are essential for identifying vulnerable plaques due to their ability to reveal high surface strains. ACS-angioscopy and OCT vividly illustrate ruptured plaques with intense surface shear stress. Imaging studies of the plaque in ACS-angioscopy and OCT are depicted in [Figure 6(ii)]. Figure 6(iii) shows the OCT method used for the plaque classification algorithm. OCT imaging modality not only facilitate plaque phenotype identification but it also allows the assessment of local hemodynamic forces effect on vessel morphology [56]. In patients present with different clinical presentation, with the objective to investigate the incidence and distribution of vulnerable plaques, various studies with the use of OCT imaging modality were conducted. Findings of these studies demonstrated that increased lipid content, calcific tissue, vessel wall disruptions and cholesterol crystals are more likely to be present in patients present with renal failure [57]. While in comparison to the normal subjects, patients present with previous history of metabolic syndrome and diabetes are more likely to have plaques with an increased necrotic core component [58]. However, in the assessment of plaque pathobiology, OCT has been extensively used, there is one small study which demonstrated the efficacy of OCT in the assessment of lesions that are more susceptible to progress and cause various adverse cardiovascular events. Findings of study proposed that vessel wall discontinuities like lipid-rich plaques, TCFA-phenotype, macrophages accumulation were present more often in progressed lesions in comparison to the lesions that remain unchanged [59]. While IVUS has limited chemical sensitivity, NIRS, which assesses lipid cores through differential light absorption, shows predictive potential for cardiac events, especially in patients with lipid-rich coronary plaques without PCI [60] [Figure 7(i) & 7(ii)].
Figure 7: Changes in RCA, Changes in LAD and NIRS and SOCT advanced imaging methods.
A. Changes in RCA and LAD.
(i) Changes in RCA.
(a) CAG shows mild stenosis 50%. (b) OCT identifies fibrous cap with the thickness of 45 micrometer (TCFA). (c) After 9 months CAG shows progression of lumen stenosis 85%. (d)& (e) OCT showed disrupted TCFA with protruding thrombus.
(ii) Changes in LAD.
CAG showing culprit lesion in LAD (a) & (b) OCT shows culprit lipid-laden plaque with rupture. (c) & (D) Post PCI with DES. (e) & (f) Lipid-laden plaque in LCX, not tight and fibrous cap thickness was 78 micrometers.
B. NIRS and OCT.
†TCFA: Thin Cap Fibroatheroma; RCA: Right Coronary Artery; CAG: Coronary Angiography; OCT: Optical Coherence Tomography; LAD: Left Anterior Descending artery; OCT: Optical Coherence Tomography; PCI: Percutaneous Coronary Intervention; DES: Drug Eluting Stent; LCx: Left Circumflex; NIRS: Near-Infrared Spectroscopy.

Figure 8: OCT and NIRS imaging method to assess vulnerable plaque characteristics.
(i) CT plaque of OCT
A. CT plaque: MΦ and TCFA- OCT imaging method: Thin cap fibroatheroma, inflammation and dense lipid area (Activity of macrophages), TCFA: Thickness of fibrous cap <65> 90o.
B. CAG showing vulnerable features
C. Plaque Vulnerability: CT vs OCT Vulnerable plaque characteristics are demonstrated by CT and OCT imaging method.
(ii) NIRS signature Significance
†CT: Computed Tomography; OCT: Optical Coherence Tomography; TCFA: Thin-Cap Fibroatheroma; CAG: Coronary Angiography; NIRS: Near-Infrared Spectroscopy; STEMI: ST-Elevation Myocardial Infarction; NSTEMI: Non-ST-Elevation Myocardial Infarction; LCBI: Lipid Core Burden Index; CABG: Coronary Artery Bypass Graft; SVG: Saphenous Vein Grafts; DES: Drug Eluting Stent; LCP: Lipid Core Plaque.
Plaques present with huge burden which is associated with poor clinical outcomes can be diagnosed by using intravascular method. It also facilitates the impact on the development of atherosclerosis by various local and systemic factors [61], enabled morphological comparison of asymptomatic with symptomatic plaque rupture, plaque development serial investigation and effect of various different therapeutic strategies on this process [62]. The PROSPECT study conducted to demonstrate the efficacy of IVUS in the assessment of plaque vulnerability and morphology in 697 patients present with an ACS demonstrated that presence of TCFA phenotype, a minimal lumen area <4mm2>70% were the strong predictors of vulnerable plaques which can be responsible to cause MACE at the follow-up [63]. In the findings of another vulnerable atherosclerosis study conducted in 170 patients present with ACS proposed that IVUS-VH used to assess the TCFA presence was the strong predictor of non-culprit lesion-related MACE [64]. Implications of local hemodynamic forces on the development of atherosclerotic disease has been evaluated by PREDICTION study in which five hundred and six patients present with ACS were enrolled. At the follow-up, at baseline low endothelial shear stress (ESS) was seen as the major predictor of development of plaque and lesions which are in need of revascularization ACS can result from various factors, including plaque erosion, rupture, and CN [65]. Current research is evaluating the combined utility of NIRS and IVUS in predicting cardiac events and guiding stent placement.
Newer Optical Imaging Technologies are:
•SOCT
•Multimodality imaging: OCT+
•NIRS
•NIRAF
•NIRF
•1-μm resolution OCT [Micro-Optical Coherence Tomography (μOCT)]
Intravascular OCT has important advantages for studying the coronary wall. Next generation OCT will increase capabilities further: Compositional/molecular (SOCT, NIRAF, NIRF, NIRS), Cellular 1-μm resolution (μOCT) Future is bright for intravascular optical imaging.
Intravascular Plaque Imaging- Vulnerable Atherosclerotic Plaque
IVUS is a diagnostic technique that visualizes plaque morphology using a backscatter signal, highlighting features such as lipid-rich cores [67]. It effectively demonstrates vessel remodeling, plaque burden, and calcification, but falls short in measuring fibrous cap thickness. Virtual histology-intravascular ultrasound (VH-IVUS) addresses this limitation by categorizing plaques into fibrous, fatty, necrotic, and calcified types. It can detect TCFAs as shown in figure 9(iii), achieving a 93% specificity against histological standards. In the PROSPECT trial, VH-IVUS, combined with other indicators, successfully predicted future cardiovascular events [1].
Figure 9: Intravascular Elastography/Palpography.
(i) IVUS utilized for intravascular elastography/ palpography.
(ii) Map of endothelial shear stress in the coronary artery created by data from IVUS, biplane cineangiography, and computational fluid dynamics.
(iii) Coronary plaque virtual histological studies.
(a) Presence of thick fibrous cap in fibroatheroma (b) Absence of thick fibrous cap in fibroatheroma.
†IVUS: Intravascular Ultrasound.
OCT, known for its superior resolution, provides detailed insights into plaque characteristics such as ruptures, cap thickness, and erosion. OCT can image atherosclerotic plaques with ruptures, distinguishing mixed thrombus and visible intimal flaps, as indicated by the arrow, in contrast to IVUS [Figure 11(i)]. Figure 10(ii) displays macrophages and TCFAs
on OCT, while figure 10(iii) compares these findings with histopathologies. NIRS identifies lipids in plaques by analyzing the absorption patterns of cholesterol molecules. When combined with IVUS, it creates a "Chemogram" particularly effective in lipid detection. The combination of OCT and NIRS potentially enhances the accuracy of lipid detection [68] [Figure 10(i)].
Figure 10: OCT imaging method for the assessment of morphological features of Ruptured atherosclerotic and vulnerable plaque
(i) Ruptured atherosclerotic plaque with other morphological features like visible intimal flap and mixed thrombus at arrow is demonstrated by OCT imaging method findings
(ii) OCT method to assess vulnerable plaque.
a. OCT method detected macrophages
b. (a) Thick capped fibroatheroma (b) thin capped fibroatheroma with high lipid content and with presence of Calcium is demonstrated by OCT imaging method.
(iii) Vulnerable plaque imaging
A. Logarithm base 10
B. Optical Coherence Tomography (OCT)
C. Corresponding histology for A and B (CD68; original magnification 100×)
D. Logarithm base 10
E. fibroatheroma with a high density of macrophages within the fibrous cap
F. Corresponding histology for D and E (CD68; original magnification 100×)
†OCT: Optical Coherence Tomography
Figure 11: Vulnerable plaque assessment with advanced imaging modalities.
(i) NIRS study demonstrate the various morphological characteristics of the vulnerable plaque.
(ii) Analogy between clinical OCT and μOCT of a vulnerable plaque with microcalcification
a. Ill-defined signal poor-region is demonstrated by Conventional OCT images (a.a’)
b. Multiple bright-red spots are demonstrated by μOCT image
c. Micro-calcification and macrophages presence is demonstrated by clinical OCT and μOCT
(iii) Micro OCT images: 1-μm Resolution OCT (μOCT)
a. Subcellular resolution microstructure
b. Three orders of magnitude resolution improvement compared to standard OCT
c. Requires special OCT catheter
†NIRS: Near-Infrared Spectroscopy; OCT: Optical Coherence Tomography; μOCT: Micro Optical Coherence Tomography; OFDI: Optical Frequency Domain Imaging.

a. Endothelium
b. Macrophages
c. Necrotic core cholesterol crystal
d. Fibrin, Platelets stents
e. MAC phagocytosis
f. 3D movie Gray-macrophage Red-yellow - Cholesterol Crystal phagocytosis
†μOCT: Micro Optical Coherence Tomography; MAC: Membrance Attack Complex.
Figure 12: Micro OCT images showing structure in resolution comparable to histology: Resolution of 1-μm
The PROSPECT-II study revealed that 14% of cardiac incidents over four years originated from untreated lesions that initially appeared benign [69]. This finding raises an important question about the optimal treatment strategy. Ongoing trials, such as FITTER and YELLOW-III, are investigating approaches like pro-protein convertase subtilisin/kexin type-9 (PCSK-9) inhibitors and localized stenting [70]. The appropriate treatment may vary based on the lesion's composition and individual patient profiles. PROSPECT-II linked high lipid content and significant
plaque burdens, as determined by IVUS, to future cardiovascular events. Plaques with these characteristics presented a considerable risk of MACE. PCI was proposed for these high-risk plaques, but the management of non-ischemic vulnerable plaques remains a topic of debate, pending conclusive trial results on the best approach, whether it be enhanced pharmacotherapy, specific interventions, or other tactics.
µOCT represents an emerging imaging technique capable of capturing human tissue luminal microstructures at a high resolution on a molecular and cellular level. A notable case report describes the use of a flexible endoscopic µOCT probe, employing helical scanning in rabbits, to acquire detailed three-dimensional imaging of arterial microstructures. This technique has potential applications in imaging cellular features of rabbit arteries that are at high risk of plaque development.
The diagnostic potential of endoscopic µOCT is particularly effective in imaging CAD plaques and stent histology. A comparison between clinical OCT and µOCT imaging of a vulnerable plaque with microcalcifications is illustrated in Figure 11(ii). Additionally, µOCT images with 1-μm resolution are demonstrated in Figure 11(iii). Examples of micro OCT images are presented in Figure 12, showcasing the technique's capability to provide detailed and high-resolution images.
Can the identification of vulnerable plaques and patients be better by the local hemodynamics forces assessment?
The high-risk vulnerable plaque remains silent in the majority of cases and does not cause MACE. Presently, there is a low production value to determine vulnerable plaques. Therefore, biochemical hemodynamic forces result in increased plaque vulnerability leading to MACE [71].
•These Biochemical events are:-
1.Shear stress in endothelium
2.Plaque Structured stress
3.Stress in Axial plaque
Accurate predictions of plaque erosion or rupture are achievable through the analysis of hemodynamic factors. Specifically, reduced wall shear stress is associated with a lower risk of MACE. The vulnerability of a plaque is influenced by factors like its lipid content and low shear wall stress. High-risk cardiovascular patients can initially be identified through non-invasive imaging techniques, which can then be complemented by invasive diagnostics for more precise risk stratification. The biomechanical forces present in vulnerable plaques increase the likelihood of rupture and subsequent cardiac events. A variety of
emerging imaging methods, catheters, and hybrid techniques are being developed to assess plaque vulnerability and anticipate potential cardiac
events [72]. The ESS in the coronary artery, an important factor in assessing plaque risk, is illustrated in figure 10(ii).
Limitations and Advantages of Imaging Techniques
Imaging techniques have shown that plaque morphology does not always correlate directly with its severity. IVUS can image ruptured plaques but it is unable to assess lipids. Intravascular MRI provides detailed morphological insights but is time-consuming. OCT excels in identifying vulnerable plaques with high resolution, yet it cannot image beyond the necrotic core. Combining OCT with IVUS results in superior imaging capabilities, particularly in distinguishing ruptured from non-ruptured plaques, with OCT providing clearer and more predictive results than IVUS [73]. CT is non-invasive and effective in detecting calcified plaques but lacks extensive clinical experience and has a lower predictive value compared to CCTA (C for lesions with a calcification score greater than 400). CCTA's diagnostic accuracy diminishes when the calcification score of vessels is high due to blooming artifacts and beam hardening induced by severely calcified plaques. Non-invasive MRI is valuable in identifying different stages of atherosclerosis and plays a crucial role in understanding plaque vulnerability, aiding in risk assessment and treatment choices [74]. The incidence of rupturing plaque, plaque erosion, and CN in patients with ACS, and the identification of non-calcified, mixed, and heavily calcified lesions by CT for comparison and high-risk plaque identification, are depicted in figure 13A, 13B, and 1

Figure 13: Incidence of Plaque rupture and classification of non-calcified, mixed and a calcified coronary arterial plaque.
(A) Incidence of rupture, erosion and calcified nodule in patients with ACS
(B) (B) Demonstration of a non- calcified, mixed and a calcified coronary arterial plaque by using CTCA. Heterogeneous, spotty white, grey, black, bulky diffuse/contagious and cleavage areas are observed in vulnerable lesions
(C) High-risk plaque identification by CT imaging method which depicts Presence of eccentric plaque with a complex signal density pattern is demonstrated by cross sectional 64 MSCT imaging: lipid rich plaque is compatible with a low-density region (yellow arrow), further a crescent moon like is density region (arrowhead) is present which represents ulcerated cavity contrast filling. White arrow
†CTCA: Computed Tomography Coronary Angiography; ACS: Acute Coronary Syndrome; CT: Computed Tomography; MSCT: Multislice Spiral Computed Tomography. Culprit plaques and vulnerable patient prevention and management
Despite advancements in medicine, CVDs continue to be a major health concern. Conservative treatment approach can be used with the objective to alter the atherosclerosis progression, to prevent atherothrombotic events and to reduce symptoms severity. This involves adopting various lifestyle modifications such as a healthy diet, smoking cessation, and regular exercise with medical therapy reduce mortality rates associated with CVDs. It's crucial for physicians to emphasize these preventative measures.
Further, in the prevention of progression of culprit lesions in vulnerable patients, a systematic intervention with pharmacotherapy has emerged as the key therapeutic strategy. The role of aspirin as a primary preventive measure is a subject of debate due to the associated bleeding risks. The growing evidence of role of lipoprotein as an additional risk factor involved has proposed that drugs which can target lipoprotein are also needed and are under evaluation. However, pharmacotherapy and PCI remain the standard treatments for ACS. The use of intravascular imaging along with anti-thrombotic agents has been effective in reducing complications related to stents. The Erosion study advocates for the use of anti-thrombotic therapy in conjunction with OCT imaging, without stenting, in certain patient cases [75].
Efforts to reduce cardiovascular outcomes also involve modulating high-density lipoprotein-cholesterol (HDL-C) with drugs like dalcetrapib. Elevating HDL-C levels has been shown to decrease vascular inflammation. Agents such as Evolocumab and Alirocumab significantly reduce low-density lipoprotein-C levels, consequently leading to a decrease in cardiac events. While statins are effective in managing lipid-rich plaques, their impact on plaque erosion is less substantial. The combined use of anti-inflammatory agents and statins has been shown to reduce cardiac events, though MACE can still occur. PCI and CABG can also make significant contribution towards relief of symptoms and potentially, to prognosis improvements in patients present with clinically relevant CAD. Marked improvements in imaging of coronary plaque may be quite beneficial in guiding duration and intensity of pharmacotherapy and could allow allocation of costly, more aggressive and novel treatment strategies in an optimum manner.
Advanced medical procedures, when combined with optimal pharmacotherapy, have been shown to reduce the risks of MACE, MI, and cardiovascular deaths. Indeed, integration of systemic and genetic risk factors with imaging information on precursor lesion can facilitate to build a personalized and refined risk model for vulnerable patients.
Executive Summary
From ischemia trial, we know that optimal medical therapy demonstrated equivalence to invasive arm in stable patients with symptoms of angina and evidence of moderate to severe ischemia. From it, we tend to increase our reliance on anatomical/morphological assessment.
Discussion
•In the progression of plaque rupture, a major role is played by three major factors: The coagulation system, Matrix turnover growth factor, and inflammatory mediators.
•Investigation of morphological characteristics of plaque plays an important role in the evaluation of future adverse cardiovascular events.
•Plaque rupture, plaque erosion, calcified nodule, thin fibrous plaque, intraplaque hemorrhage, thin fibrous cap, and necrotic core which are rich in lipid content leads to ACS.
•Asides from these factors, certain other biomechanical forces such as endothelium shear stress, axial plaque stress, and plaque structured stress modulate the vulnerability of plaque causing additional fragility and ACS events.
•Several non-invasive and invasive imaging approaches like CT, IVUS, MRI, and OCT can be employed initially to evaluate plaque vulnerability which is linked to the drawback of negative predictive value.
•Hybrid Intracoronary IVUS-NIRF and OCT-NIRF can be the better diagnostic methods in risk stratification owing to their high predictive value.
•Next-generation intravascular optical imaging technologies contain the vast no. of opportunities for the future for vulnerable plaque evaluation because of their advantage of investigating the coronary wall compared to other imaging procedures.
•An enhanced imaging procedure can be the guiding force in the selection of novel strategies for the treatment of patients. The Summary of various vulnerable plaque detection methods is demonstrated in Central Illustration.
Although, the concept of vulnerable plaque remains controversial but with the evolving of new non-imaging and imaging modalities there is a hope of preventing CAD by detecting which plaques are more prone to rupture causing MACE and subsequently preventing it. Newer developments like artificial intelligence can function as a critical diagnostic tool in the prevention and management of patients at huge risk.
Future perspectives:-
•Plaque vulnerability and rupture risk are influenced by various hemodynamic and anatomical factors.
•The original vulnerable plaque theory aimed to explain acute clinical events due to atherosclerotic plaques.
•Most clinical studies focused on intrinsic factors, often neglecting the concept of plaque vulnerability.
•Technological advancements have improved understanding and treatment of atherosclerosis by applying the vulnerable plaque concept, especially with advanced computational models.
•Two complicating factors in determining when to treat plaques are plaque interdependence and their ability to change locations.
•Clinical trials show that treating patients with vulnerable plaques doesn't significantly affect lesion development, and only some ruptured plaques cause cardiovascular events.
•The positive predictive value of plaque vulnerability for analyzing ACS and atherosclerotic plaques is relatively low.
•Numerous tools have emerged for plaque assessment, including imaging modalities, blood tests, and hemodynamics. Enhanced identification methods involve molecular tests, computational fluid dynamics, and imaging tests to examine various molecular signals in the plaque.
•There's a challenge in identifying vulnerable patients due to the impracticality of imaging the entire population; a non-invasive method is required to screen before selecting patients for imaging.
•Despite controversies, there is optimism for preventing acute events in patients with CAD in the future.
The lead author of the review article is Dr Rohit Mody. Dr Pankaj Goyal, Dr Debabrata Dash, Dr Bhavya Mody, Dr Amit Munjal, Dr Bankey Bihari and Dr Rahul Singla had equal and substantial contributions in the formation of this review article. They were involved in conceptualization, data curation, formal analysis, resources, software, validation, visualization, writing - original draft, Writing, review & editing.
I thank Rohit Kumar for assisting me to finalize the review article. Figures are edited by Jiwan Singh.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical approval was not required since it is an accepted procedure
Written consent has been obtained to publish the review article from the guardian. The consent copy is available with the authors and ready to be submitted if required.