AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2642-9756/110
1 Department of Obstetrics and Gynecology, Faculty of Medicine - Zagazig University. Sharkia, Egypt
2 Department of Tropical Medicine, Faculty of Medicine - Zagazig University. Sharkia, Egypt
*Corresponding Author: Ahmed M. Radwan. Department of Obstetrics and Gynecology, Faculty of Medicine - Zagazig University. Sharkia, Egypt.
Citation: Ahmed M. Radwan, Sherweet M. Ahmed. (2022). Thyroid Dysfunction in Postmenopausal Women: Across Section Study, J. Women Health Care and Issues, 5(6) DOI: 10.31579/2642-9756/110
Copyright: © 2022 Ahmed M. Radwan. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 02 August 2022 | Accepted: 19 August 2022 | Published: 05 September 2022
Keywords: thyroid dysfunction; postmenopausal women
This study was conducted on postmenopausal women who went to internal medicine and gynaecological outpatient clinics for various purposes during the period from 1/3/2021 to 1/2/2022. The aim of this work was to study possible relationship between thyroid disorders and menopause. Our study included 80 women who were postmenopausal. Patient with history of thyroid disorders, autoimmune diseases, liver disease, renal disease and patient on amiodarone or other drugs that affect thyroid function were excluded from the study.All cases were subjected to the following: History , examination , Routine investigations and Thyroid gland hormones (TSH, free T3 and free T4) and thyroid autoantibodies (TPO and TG).The result of this study showed that: Among our post-menopausal women there was 17.5% of them had thyroid disorders. The frequency of different thyroid disorders in our post-menopausal women was as follow: 10 women out of 80 (representing 12.5%) were overt hypothyroid, 4 women (5%) had subclinical hypothyroidism and 22 women (27.5%) classified as non-thyroidal illness syndrome. While 44 women (55%) were euthyroid. Thyroid auto antibodies were detected in 15% in cases of the study distributed as follow: 5% were overt hypothyroid, 2.5% had subclinical hypothyroidism and 7.5% were euthyroid women.
Conclusion: Thyroid disorders are common in women in postmenopausal age. Overt hypothyroidism is the most common thyroid disorder in them, followed by subclinical hypothyroidism and thyroid autoantibodies are present in high percentage of women whether they have thyroid disorders or are euthyroid.
There has been expanding enthusiasm for thyroid capacity in the elderly in view of relationship of thyroid status with incapacity, intellectual capacity, risk of cardiovascular sickness, and life span [1]. Thyroid autoimmunity is more regular in females than in males, presumably as a result of the activity of sex hormones, estrogens and androgens on the invulnerable framework [2]. In a group based multicentric investigation of the characteristic history of the menopausal 9.6% predominance of increased TSH outside the euthyroid extent was discovered [3]. It is found that serum TSH increase (mean increment of 0.32mU/L) with no change in free T4 with menopause [4]. A few appearances of menopause are like the signs and side effects associated with thyroid brokenness. Hot flushes, bigotry to warmth, sweating, palpitations, fractiousness, a sleeping disorder, and fast changes in temperament can be followed back to a case of hyperthyroidism, while skin decay, clogging, fragile hair, periorbital edema and expansion of weight are appeared in hypothyroid subjects [5].
Aim of the Study: This study was designed to study possible relationship between thyroid disorders and menopause.
Subjects and Methods : This study was Cross-sectional study conducted at United doctors’ hospital, Jeddah KSA, and included 80 postmenopausal women who went to internal medicine and gynecology outpatient clinic for various purposes during the period from 1/3/2021 to 1/2/2022.
Aim of the work: This study was designed to study possible relationship between thyroid disorders and menopause
Inclusion criteria: Women above fifty years with cessation of menstruation. Post menopause can be defined as stoppage of menstrual flow for a period of 12 months and above 6.
Exclusion criteria:
• Patient with history of thyroid disorders.
• Patient receives drugs affecting thyroid function e.g amiodaron.
• Autoimmune disease.
• Chronic disease (liver disease-renal disease).
All patients will undergo:
Complete History taking, Full examination, routine investigations and
• Thyroid gland hormones (TSH, free T3 and free T4) and thyroid autoantibodies (TPO and TGA)
Table (1): showed the demographic data of our subjects. The mean age of our subjects was 61.6±8.6 years and the mean BMI was 34.6±4 kg/m2. Most of our cases were obese, thyroid disorders in post-menopausal women were 17.5%. The frequency of different thyroid disorders in our post-menopausal women was as follow: 12.5% were overt hypothyroid, 5% were sub clinically hypothyroid and 27.5% classified as nonthyroidal illness syndrome. While 55% were euthyroid. Table (2) showed that prevalence of thyroid auto antibodies among our postmenopausal women were as follow: 5% were overt hypothyroid, 2.5% had subclinical hypothyroidism and 7.5% were euthyroid women. Thyroid auto antibodies were detected in 15%. table (3) showed that 27.5% were hypertensive where mean systolic blood pressure was 162.53±14.1mmHg and mean diastolic blood pressure was 98.33±9.6 mmHg. While the other 72.5% were normotensive where mean systolic blood pressure was 121.47± 12.5mmHg and 76.938.3 mmHg. table (4) showed that 27.5% were diabetic, with mean FBG: 195.36 mg/dl and mean PPBG: 278.21 mg/dl. and the others 72.5% were euglycemic. Table (5) showed that there was negative nonsignificant association between age, T3 (r= -0.14) and TSH (r= -0.1). There was positive non-significant association between age and T4 (r=0.06), TPO (r=0.06) and TG (r=0.01). (P>0.05), There was positive significant association between BMI and TSH (r=0.41) (P =0.01), TPO ab (r=0.34) (P =0.05) and TG ab (r=0.40) (P =0.01). But there was positive nonsignificant association between BMI, T3and T4 (P >0.005). Table (6) showed that 45% of our cases had different types of comorbidity distributed as follow: Hypertension in 8 women (10%), DM in 8 women (10%), both DM & Hypertension in 14 women (17.5%), cancer cervix in only 2 woman (2.5%) and cholecystitis in 4 women (5%). While 55% (44 women out of 80 women) had no associated comorbidity. Table (7) showed association between hypertension, DM and other comorbidities with hypothyroidism. Among different types of comorbidities there was positive significant association between hypertension and hypothyroidism (x2=0.0) (P =0.02), also there was positive significant association between hypothyroidism and DM (x2=8.03) (P =0.004). However, there was positive nonsignificant association between hypothyroidism and other comorbidities (x2=0.63) (P =0.42).
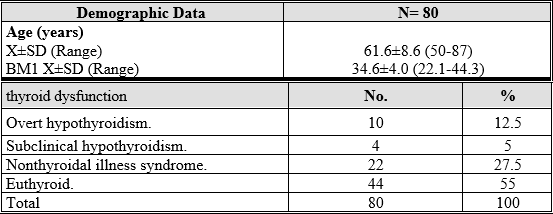
Table 1: Mean age, BMI and Prevalence of thyroid dysfunction of study group
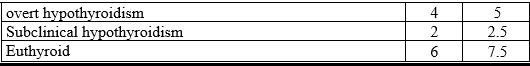
Table 2: Prevalence of thyroid auto antibodies among study group
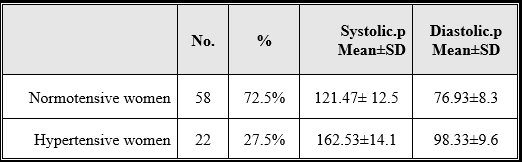
Table 3: Mean value of Arterial Blood Pressure in study group
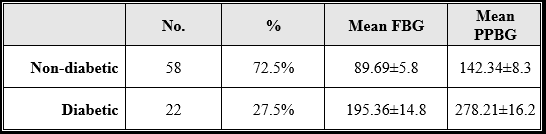
Table 4: Mean value of blood glucose in study group.
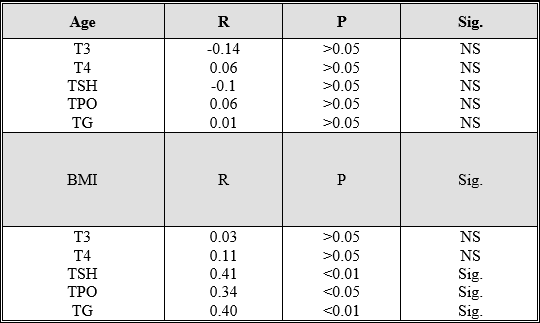
Table 5: Correlation between age, BMI and thyroid function of study group.
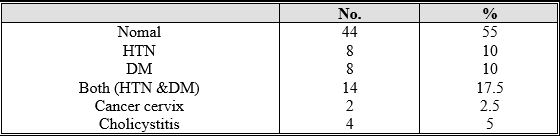
Table 6: Different Comorbidity associated with study group.
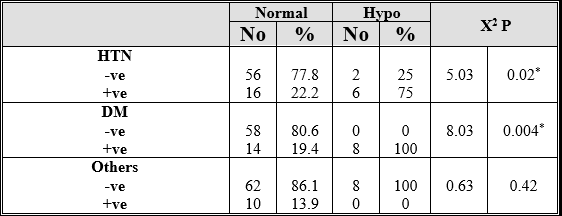
Table 7: Association between hypertension, DM and other comorbidities with hypothyroidism in study group.
This study was designed to study possible relationship between thyroid disorders and menopause. Our study revealed that demographic data of our subjects were: the mean age was 61.6±8.6 years and the mean BMI was 34.6±4 kg/m2. Most of our cases were obese. Among our post-menopausal women there was 17.5% of them had thyroid disorders. The frequency of different thyroid disorders in our post-menopausal women was as follow: 10 women out of 80 (representing 12.5%) were overt hypothyroid, 4 women (5%) were sub clinically hypothyroid and 22women (27.5%) classified as non-thyroidal illness syndrome. While 44 women (55%) were euthyroid.
As regard thyroid auto antibodies our study revealed that it was detected in 15% of our cases distributed as follow: 5% were overt hypothyroid, 2.5% had subclinical hypothyroidism and 7.5% were euthyroid women.
In our study we found that TPO ab were present in 10 cases: 2 woman was hypothyroid, another woman had subclinical hypothyroidism and 6 women were euthyroid. While only 2 woman diagnosed as overt hypothyroidism had TG ab. Our study uncovered that unmistakable hypothyroidism spoke to 12.5%.
As respect subclinical hypothyroidism, our study uncovered that it speaks to 5% of our cases; this is in concurrence with Fatourechi et al., 2019 who found that commonness of subclinical hypothyroidism is 3-8%, expanding with age and being more regular in ladies. However different studies uncovered higher rate of subclinical hypothyroidism where Chakera et al., 2012 found that subclinical hypothyroidism reach up to15% to 18% in ladies who are more than 60 years old. [7,8]
Frequencies of unmistakable and subclinical hypothyroidism change among the studies. Such varieties could be connected with a few nearby variables, incorporating contrasts in iodine admission among populaces, contrasts in cut-off qualities utilized for thyrotropin and FT4 levels and systems of test choice among studies.
Our study showed that non-thyroidal ailment disorder spoke to 27.5% of our postmenopausal ladies , in consent to our outcomes, Tognini et al., 2020 found that the commonness of NTIS (particularly low T3 disorder) in hospitalized more seasoned patients, was 31.9% .While in another study, Adler and Wartofsky, 2017 found that the pervasiveness of NTIS is around 11–18% in records of non-chose hospitalized patients and expansions up to 60–70% among patients admitted to serious consideration unts.[9,10] Some of our cases were admitted to intensive care unit while the majority were admitted to surgery and gynecology departments and prepared for surgery, so they were under stress which is an important cause of nonthyroidal illness syndrome. Also, we found that there was mild decrease in free T3.
On studying thyroid autoantibodies, our study revealed that it was present in 15% of our postmenopausal women, and distributed as follow:5% (two out of forty women) were overt hypothyroid, 2.5% (one out of forty women) had subclinical hypothyroidism and 7.5% (three out of forty women) were euthyroid women. Vanderpump, 2015 found that early after death thinks about affirmed histological proof of constant immune system thyroiditis in 27% of grown-up ladies, with an ascent in recurrence more than 50 years. [11]
In our study there was sure thyroid autoantibodies in 13.6% (3 out of 22women) of euthyroid cases, this is in consent to our study, Biondi and Cooper 2018 who found that the reported commonness of distinguishable TGAb and TPOAb levels were 10 and 12% of the solid populace. [12]
The vicinity of hostile to TPO and against Tg antibodies (TgAb) in the blood can be utilized to analyze fundamental autoimmunity without clinical side effects [13].
90% of patients with Hashimoto's illness have hoisted flowing TgAb, the vicinity of high TgAb, alone, is not adequate to make an analysis, as this variation from the norm is likewise found in patients with other immune system issue, for example, rheumatoid joint pain and type I diabetes [14].
On considering relationship in the middle of age and thyroid hormones or thyroid antibodies, it was found that there was negative non-huge relationship in the middle of age and T3 and TSH. In any case, there was certain non-noteworthy relationship in the middle of age and T4 or thyroid antibodies. likewise, Suzuki et al., 2012 found that in females, the free thyroid hormone levels were not changed with maturing but rather, in opposition to our stuy, TSH level expanded in age-subordinate way. Benseñor et al., 2019 found that recurrence of thyroid issue did not change as indicated by age, likewise against thyroperoxidase antibodies were steady and did not change as per age. In spite of our study, information from the National Health and Nutrition Examination Survey (NHANES III) demonstrated a predominance of hostile to thyroperoxidase antibodies that increments with age in both men and ladies [15,16,17].
Mean age of women involved in our study was 61 years, while most of studies which found increase in thyroid hormones and antibodies with age were conducted on elderly women. Our results may be also due to small number of cases in our sample.
On studying BMI, our study revealed that most of our postmenopausal women were obese. There was positive significant association between BMI and TSH, TPO ab and TG ab. In consent to our discoveries, Amrita et al., 2013 concentrated on the relationship between various BMI gatherings and serum TSH and they reported that as the BMI expanded mean estimation of serum TSH additionally expanded. Be that as it may, Svare et al., 2019 found a negative relationship between standard BMI and serum TSH [18,19]
Fat tissue could impact thyroid hormones in different ways. In any case, the effect may be a direct result of a change in deiodinase activity in central and/or periphery tissue, Second, hormone resistance in substantial subjects as an outcome of a T3 receptor reduction has been proposed. Third, a mostly bioinactive TSH protein in heavy subjects has been hypothesized [20].
Our study demonstrated that 27.5% of our cases were diabetic. (table.10). There was sure huge relationship in the middle of hypothyroidism and DM. In consent to our outcome, a study done by Akbar et al., 2016 reported a pervasiveness of thyroid issue in 16% in Saudi T2DM patients [21]
Our study 27.5% were hypertensive, In consent to our outcomes, Grais et al., 2015 found that the mostwidely recognized cardiovascuar indications of hypothyroidism is diastolic hypertension, since hypothyroidism diminishes endothelial-interceded vasorelaxation and vascular consistence and in this way, hoisted diastolic circulatory strain. [22]
In the hypothyroid state, the thickness of α1‑adrenoreceptors is expanded while β‑adrenoreceptors are lessened in vascular beds. Activities of α1‑adrenoreceptors for the most part include smooth muscle cell constriction, bringing about vasoconstriction in the veins, while decreased β-adrenoreceptors can affect low heart yield, renin emission from the kidneys, low lipolysis and anabolism in skeletal muscle. [23].