AUCTORES
Globalize your Research
Review Article | DOI: https://doi.org/10.31579/2642-973X/029
Centre for Human Reproduction721, G.T.B. Nagar, Jalandhar-144001Punjab, India
*Corresponding Author: Kulvinder Kochar Kaur
Citation: Kulvinder Kochar Kaur. (2022). The controversy regarding the COVID19 Infection causing Neurodegeneration, new Parkinson’sdiseaseor its acceleration remains unresolved: a Narrative Review’’.J Brain and Neurological Disorders. 5(2); DOI:10.31579/2642-973X/029
Copyright: 2022, Kulvinder Kochar Kaur, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Received: 09 May 2022 | Accepted: 15 August 2022 | Published: 08 October 2022
Keywords: sars-cov2; covid19 pandemic; ndd; parkinson’s disease; viral infection
The SARS-CoV2 pandemic has impacted the life of the population globally from 2020.The association amongst the new viral infection besides pathogenesis of various neurodegenerative diseases (NDD) got evaluated in different studies .In this review our objective was to carry out assessment, of the available publications regarding Parkinson’s disease (PD) and the COVID19 pandemic for provision of association amongst, the crossing of viral infection along with neurodegeneration regarding the present issue . Here we emphasize the SARS-CoV2 neurotropism, neuropathology, along with our belief regarding the association amongst infection, neurodegeneration in addition to the psychosocial influence of the pandemic in PD patients. Despite the corroboration of SARS-CoV2 pandemic in this review pointing towards a greater incidence of NDD in the future. Still existence of lot of controversies are there’re garding enough outcomes for corroboration of COVID19 possessing the capacity of either result in stimulation of generation of new or exacerbation of the the existent NDDs.
With the initiation of COVID19 certain doubts were raised regarding the central nervous system (CNS) involvement. Thus, here we had the objective of provision of a summary in the context of association amongst COVID19, other viral infections as well as Parkinson’s diseases subsequent to reviewing varios aspects of Coronavirus disease (COVID19) besides various neuro degenerative diseases [1-8]. Hence variable modes by which SARS-CoV2 viruses might impact various cerebral functions besides result in induction of neurodegeneration need to be taken into account. i) the direct neurotoxic action of the virus that result secondary to neuro invasion is feasible in addition to actions due to systemic inflammatory changes. Initially we deal with the information with regards to SARS-CoV2 neurotropism, neuropathology, neuroinflammation along with alterations in the amounts of biomarkers which have been found in the course of infection .ii) subsequently we describe in brief the association amongst other viral infections along with neurodegenerative diseases(NDD), with our concentration being mainly on neurodegeneration, with attention centred on Parkinson’s disease(PD) in addition to cognitive impairment / Alzheimer’s disease (PD/ AD).iii)Finally we detail the impact of the pandemic on symptoms as well as psychosocial angle in case of patients with PD along with stress on the considerable influence of the infection in particular on individuals possessing prior neurological disorders in addition to disabilities.
Methods
Here we conducted a narrative review utilizing search engine pubmed, google scholar; web of science: embase Cochrane review library utilizing the MeSH terms like SARS-CoV2; COVID19; other viral infections; neurodegenerative diseases (NDD); Parkinson’s diseases; AD; from 1991 till 2021 till date from 1990 to 2022 till date.
Results
We found a total of 300 articles out of which we selected 124 articles for this review. No meta-analysis was done.
The etiological agent of the present pandemic is a member of the family Coronaviridae[1 rev by us].The earlier species of Corona viridae (like HCoV -OC43), HCoV -229E, SARS-CoV, MERSCoV) were observed in human brain samples ,that corroborated their neurotropism along with them possessing the capacity of resulting in indelible infections of central nervous system(CNS)[9].As early as 1999 it was illustrated that neuroblastoma, neuroglioma along with glial cells possessed a proneness towards infection with human Coronaviridae in addition to the information that this virus possessed the capacity of lingering around for a minimum of 130 days of culture duration[9].In case of animal models, this ineffaceable infection resulted in elimination of neurons in addition to long term consequences like reduction in action,besides volume of hippocampal neurons in the form of neurodegenerative phenotype [10-12].
A controversy is existent regarding SARS-CoV2 possessing the capacity of entering along with being indelible in cerebral structures. Actually, certain results that corroborated the posit of SARS-CoV2 neurotropism are detailed here. regarding
The Identification of angiotensin converting enzyme (ACE2) receptor was the maximum common receptors observed for its entry [7]. Nevertheless, its expression is less prevalent in the brain in contrast to other tissues[13].In Consists expression was illustrated on glial cells(astrocytes),capillary endothelium, monocyte/ macrophages, along with neurons[14].In contrast to this greater expression of ACE2) receptor was seen in the brain stem that resulted in the posit that invasion by SARS-CoV2 in brain stem structures might result in their impairment that are implicated in controlling CVS functions [15] . An infection of the ACE2 receptor in transgenic mice resulted in expression of viral antigen in neurons, in particular in thalamus, brain stem, cerebrum, whereas cerebellum continues tobe unafflicted [11]. The influence brain regions illustrated neuronal depletion as well as microglial activation without any inflammatory signs [11].
Conversely escalated proof existed regarding ACE2 receptor might not be the primary viral invasion approach into the central nervous system(CNS).Rather other receptors might be implicated like neurolipin 1(NRP1)might aid considerably in SARS-CoV2 entry in cerebral structures[16-18].Abundant NRP1 expression was observed in neurons along with astrocytes[17].
Three major routes had been suggested to result in SARS-CoV2 invasion in CNS are detailed hereafter. [15,16,19].
The initial probable mode being, the trans neural method initiated in the nasal epithelium along with olfactory nerve propagateng into brain through axonal transportation[14].This route of SARS-CoV2 neurotropism got illustrated for SARS-CoV2 along with HCov-OC-43 subsequent to intranasal infection [10,20].In transgenic mice expressing ACE2 receptor, SARS-CoV2 intranasal infection led to neuronal10,20] . Furthermore, the mouse equivalent of the human Coronavirus, the mouse hepatitis virus gained entry into brain through olfactory nerve following intranasal inoculation [21].
It was corroborated that neurotropism is the common mode that caused occurrence of olfactory impairment (OI)in COVID-19. Broad variable incidence of OI correlated with COVID-19(5-98%) was seen basically secondary to no objective evaluation [22]. Utilizing objective smell evaluation in 60 Iranian COVID-19 patients it got documented that 98% of them illustrated anosmia, however just 35% had subjective realization of their OI , emphasizing the significance of objective evaluation regarding this symptomatology[23].Gustatory impairment is frequent too in COVID-19 resulting in diagnostic dilemma with olfactory impairment [24]. Apparently OI is an early presentation during COVID-19 course[25].Generally 2 modes might cause OI i)blockade of the olfactory cleft via swelling or rhinnorrhoea that might not have been picked up in COVID-19 patients[23,24,26].ii)defective sensorineural transmission might result in dysfunctional sense of smell[24].With utilization of CT along with MRI imaging study in details in COVID-19 patients with protracted OI (least 1 mth) documented reduction in olfactory bulb volumes(43.5%) along with olfactory sulci being shallow (60.9%),thus corroborating this pathogenesis for OI in COVID-19[26] . Nevertheless, there is lack of ACE2 receptor in olfactory sensory neurons along with their observation in supporting cells, sustenacular cells besides horizontal basal cells (alias reserve Stem Cells )in the olfactory along with respiratory epithelium[22].This OI is usually a frequent symptom in elder patients occurrence of OI is in 10%of individuals >65 yrs along with in 62-80%in >80yrs[24] .OI is further realized to be a symptom of Alzheimer’s disease(AD) as well as Parkinson’s disease(PD) [24]. Intriguingly OI in COVID-19 takes place more frequently in younger patients possessing inverse association with demise[27].This corroborates with the posit that is in contrast regarding OI being a sign of defense against the virus for avoidnce of the arrival of the virus in the cerebral structures instead ofjust avoidance of entry in the CNS[28].
b) The other alternate transneural method of invasion approach in CNS by SARS-CoV2 implicates the trigeminal or vagal nerve has further got described.
ii)) The second route suggested for CNS viral invasion is the hamatogenous route that gets followed by crossing of the blood brain barrier (BBB)/choroid plexus infections [15,16,19]. This has been detailed regarding other viruses like HIV, HSV, HCMV besides enteroviruses [12].
In this particular route endothelial cells in blood vessels besides choroid plexus might be the invasion target in view of expression of ACE2 receptor demonstrated in them [16]. Furthermore the spike protein of SARS-CoV2 might cross along with result in impairment of the BBB by stimulation of an inflammatory response amongst the microvascular endothelium[29].
The other mode validating this route might be enhanced permeability of BBB secondary to escalation of interleukin-6( IL-6) amounts, existent in acute COVID-19 disease[19,30].
iii)The third probability regarding pathway of SARS-CoV2 neurotropism is what is referred to as the ‘’Trojan horse mode’’-detailing the viral infection of immune cells (neutrophils, monocyte, macrophages, CD4+ lymphocytes) that arrive in the CNS via blood stream followed by migration into cerebral structure by diapedesis [15-17]. On arrival in the cerebral tissue, the virus/viral particles might get liberated by these immune cells [16]
2.1 Neuropathology of SARS-CoV2
Usually Neuropathological cornerstone of COVID-19 autopsy patients reveal generalized oedema, gliosis with microglial along with astrocytes activation, ischemic damage, intracranial bleeding, arteriosclerosis, hypoxic ischemic damage, encephalitis /meningitis along with diffuse inflammation [31]. COVID-19 patients presenting with robust disease illustrated decreased neuronal amounts besides escalated activated microglial along with astrocytes amounts in addition to greaterproinflammatory cytokines as estimated by qPCR [32].
In parallel with posit of hematogenous route of invasion brain, Paniz Mondolfi etal. isolated this virus in capillary endothelium along with neurons from frontal lobe tissue in COVID-19 patients [16,33]. In vivo virus was not observed in glial cells [16]. Akin observation was of SARS-CoV2 preference in CNS endothelial cells by identification of ACE2 receptor expression in smooth muscle of blood vesse [34]. In5/9 patients small blood vessel disease was seen in autopsy patients; Nevertheless, SARS-CoV2 was found in a lone case with utilization of Immunohistochemistry [35]. Utilization of PCR in brain for estimation of SARS-CoV2 was tough as well; maximum viral load was seen in the olfactory bulb, whereas SARS-CoV2 PCR was negativecontinuously in the substania nigra [28,34,36]. Nevertheless, observation of viral existence was occasional in viral encephalitis usually (like herpes virus, arbo virescent virus stimulated encephalitis) [12].
COVID-19 brains on autopsy patients revealed microglial activation in olfactory bulb, frontal, hippocampus with maximum load seen in the brain stem, while no activation of lymphocytes was visualized apparently [35]. Intriguingly, patients with history of delirium at the time of COVID-19 illustrated greater microglial activation in the hippocampus [35]. Those patients whose presentationwas with/ without sepsis was not feasible neuropathologically that countered the usual posit of neuropathology generation secondary to a cytokinestorm at the time of septic disease [35].
2.2 SARS-CoV2 Neuroinflammation along with Biomarker
Besides direct impact of SARS-CoV2 on brain by CNS invasion, the remaining actions on cerebral functions secondary to systemic change in the disease course have been broadly described. Brain tissue along with biofluids investigations besides the systemic response demonstrated a neuro(inflammatory) reaction initiated by COVID-19. Escalation of numerous cytokines in the blood at the time of acute COVID-19 were seen, whereas enhanced proinflammatory markers amounts were not found in the cerebrospinal fluid (CSF) [37]. Serum amounts of IL-4, IL-10, IL-6, along with IL-1β were escalated in patients of COVID-19[29,38]. Knowledge is existent regarding IL-1β as well as IL-6, possessing the capacity of stimulating neuro inflammation [14].
Common determination of SARS-CoV2 COVID-19 patients was observed despite its incapacity of corroborating intrathecal antibody generation [37,39,40], Determination of virus by the
quantitative polymerase chain reaction(qPCR) from CSF was not feasible in maximum patients [41,44,5], Description of sporadic positive outcomes obtained in SARS-CoV2 PCR from CSF was documented rarely by authors in patients with robust cerebral symptoms [41].
Evaluation of markers pointing to CNS injuries documented escalated amounts of neurofilament light chain (NfL) along with glial fibrillary acidic protein (GFAP)in plasma of patients with moderate to robust COVID-19[17,49]. Moreover 3/8 patients with robust COVID-19 displayed signs of break down in blood brain barrier, one possessed particular intrathecal antibody generation ,while 4 illustrated positivity for14-3-3in the CSF[44].The outcomes of CNS pleocytosis were contradictory thus far.In acase series comprising of 15 patients besides a review described CSF WBC counts in 409 COVID-19 patients presenting with neurological symptoms found commonly pleocytosis (by definition>5 cells /μL) in 36% of 15 along with 17% of 409 patients [30,50]. Conversely acase series comprising of 13 patients with COVID-19 as well as encephalopathies / convulsions documented CSF pleocytosis in a single patient only akin to a study comprising of 18 patients of COVID-19 along with neurological complications observed pleocytosis in 4patients besides documenting that all 4 were most probably secondary to blood contamination [51.2].
Assessment of cargo of neuronal –enrichment of extra cellular vesicles (ECV’s)was conducted by Sun etal. Intriguingly they found enhanced NfL, amyloid –β, neurogranin, tau as well as phosphorylated tau in COVID-19 patients pointing to a neurodegenerative event [42].
Other than the COVID-19 pandemic, a wide epidemiological corroboration associating other viral infections with neurodegenerative diseases (NDD), particularly of PD as well as AD exists.
The thought that viral infections possess the capacity of facilitating neurodegeneration was initially generated with encephalitis lethargica subsequent, to Spanish flu epidemic at the initiation of 20th century. Following that an association amongst infections with NDD got assumed repetitively.
A meta-analysis of 287,773 patients with PD along with7,102,901 controls documented that the patients with documented infections earlier possessed escalated risk for PD (odds ratio,1:20) [44]. Bacterial infections were believed to be implicated for these actions[44].In agreement another recent study observed a ‘’greater infectious burden ‘’,that by definition was the presence of greater antibodies against various viruses along with bacteria in blood of PD patients[45] .With in particular PD risk was demonstrated to be escalated subsequent to VZV infections (adjusted hazard ratio[HR],1:17) as well as PD patients possessed seropositivity with greater probability for EBV[46].HCV has been a well-documented factor for PD ,like HSV1infection for AD generation [47, 48].
Influenza viruses were further correlated with PD,as encephalitis lethargica possessed a Parkinsonian phenotype along with Influenza virus was posited to be the etiological agent regarding Spanish flu[53]. Moreover, H1N1 infection resulted in continuous microglial activation in the form of chronic neuroinflammation in case of wild kinds of mice [49]. H1N1 thus caused microglial activation along with α-synuclein accrual in mice leading to dopaminergic neuronal depletion in the substania nigra, which is believed to be the pathological landmark of PD [50]. Additionally, Influenza virus was observed in the autopsy of PD patients in substania nigra [51]. Utilization of outcomes of a recent case control study from the results of a Danish National patient registry illustrated that there was a correlation amongst diagnosis of Influenza with the generation of PD upto 10yrs subsequently (OR1.73) [52]. Thus, this robust correlation existence however requires greater evaluation.
Japanese encephalitis virus results in Parkinsonian phenotype at the time of acute disease, however continued Parkinsonism with MRI wounds in the substania nigra was seen 3-5 yrs subsequent to the Viral Infection [53].
Induction of Parkinsonism by West Nile virus is feasible at the time of acute infection.In post mortem evaluation escalated α-synuclein amounts were seen in patients infected with West Nile virus [46,54].An Intriguing posit regarding α-synuclein function was generated in an α-synuclein knockout mouse model subsequent to the West Nile infection[54].The lack of α-synuclein in this model resulted in dramatic propagation of the disease pointing to α-synuclein confers protection against Viral Infection[46,54].The posit given was entrapment of viral particle by α-synuclein in the form of a cellular defense mode,that continues subsequent to the infection resulting in its pathological accrual followed by neurotoxic actions. The akin mode was posited for β-amyloid that possess the capacity of entrapment of HSV1 besides hampering its viral replication along with entry in vivo as well as in vitro[55].Disease risk factor was attributed to HSV1 infection greater in AD however in PD as well in variable in vivo as well as in vitro evaluation [56].Enhancement by2.56 times risk factor for dementia generation was documented in a retrospective cohort study, comprising of 8362 patients with acute HSV1 or HSV2 infection[48].A phase 2 study evaluating if acyclovir possesses the capacity of reduction of propagationn of AD in patients with HSV1 is presently continuing (Clinical trials.gov NCT03282916)[55].
Various studies are existent pointing to implication of adaptive immunesystem in the generation of neurodegeneration. Genome wide association studies(GWAS) observed correlation of particular major histocompatibility complex II gene alleles with PD as well asT cells of patients with PD were illustrated to react with α-synuclein epitope [57]. Demonstration of Th17 Tcells aiding in PD pathogenesis in a cell culture with utilization of induced pluripotent Stem Cells(iPSCs)was doneby another group [58]. Recently Tcells were observed to be neighbouring the Lewy bodies in addition to dopaminergic neurons in brains of Lewy bodies dementia patients along with stimulating CD4+ T cells with a phosphorylated α-synuclein epitope caused escalation of IL17 generation as a sign of Th17reaction [59].
The earlier described mode of viral neurotropism along with neuroinflammation stimulate a query regarding long term neurodegeneration has to be anticipated subsequent to COVID-19 disease.
SARS-CoV2 along with pathogenic proteins possessing the potential of impacting neurodegeneration have been correlated in various studies.It was found that spike protein receptor binding domain binds to heparin as well as heparin binding proteins inclusive of, -amyloid β, α-synuclein,tau,prion besides TDP-43 which might precipitate the pathological accrual of these proteins leading to neurodegeneration [60]. Akin mode has been detailed regarding HSV1 that catalyzes the accrual of amyloid β in vivo, as well as in vitro, having been well documented risk factor for AD [60]. Recent illustration was that viral particles (inclusive of SARS-CoV2 spike protein) promoted the transmission of protopathic seeds by changing intercellular cargo transport [61].
Variable approaches utilized for snatching the regulation of host cellular functions like disrupting autophagy besides mitochondrial or lysosomal function that are responsible for generation of NDD also [62]. i SARS-CoV2 changes autophagy besides mitochondrial or lysosomal function in lungs that are infected [63].
Moreover, viral alterations of proteastasis in the host cell can result in escalated aging of the infected tissue that might further accelerate the neurodegenerative event, often visualized in senescent cells [62]
Ferrosenescence represents an iron modulated premature aging event of cells causing iron stimulated disturbance of DNAhealng that gets followed by neurodegeneration [64]. This represents an intriguing capacity of virus of inducing ferro senescence in host cells causing facilitation of viral replication [64].
4.1 COVID19 along with potential modes associated with Parkinson’sdisease
There are various correlations amongst COVID19 along with the generation of PD described further.
That the mouse hepatitis virus (isolated as a murine analogue of human Coronaviridae) was found to result in mild encephalitis besides viral antigen got deposited mainly in the nucleus subthalamicus as well as substania nigra [65]. Following gliosis in these areas was pointing to acorrelation amongst the virus along with PD doorpost encephalitic Parkinsonism [65]. Escalation of antibodies against Corona viridae were observed in the CSF of patients with PD in contrast to controls by 1992 itself [66].
The documentation of 3 case reports of PD initiation at well-timed association with COVID19 disease. Nevertheless, no clear-cut etiological association could be found [67].
2 patients generating COVID19 correlated encephalitis with propagating atypical parkinsonism as well as FDG-PETchanges reminding of post encephalitic Parkinsonism got published [68].
Numerous modes by which COVID19 might aid in the generation of PD got reviewed; i) Vascular injuries in the nigro striatum mightoccur following Parkinsonism [69]. Moreover, the cytokine storm correlated with robust COVID19induced neuroinflammation, followed by neurodegeneration [30,69]. Systemic amount of IL-6 was enhanced with a small prospective observational study showed a greater amount of IL-6 is correlated with an escalation of generating PD [70].
The other plausible mode of PD induction might be viral neurotropism leading to direct neuronal injury in important regions. IPSC obtained mid brain dopaminergic neurons were illustrated to be prone to SARS-CoV2 infection, that initiated an inflammatory response followed by cellular senescence in vitro[89].RNA sequencing evaluation of the ventral mid brain tissue of COVID19 patients illustrated an akin phenotype of neurons which were inflamed besides Identification of low amounts of SARS-CoV2 transcripts [71].These outcomes emphasized regarding particular proneness to SARS-CoV2 of specifically susceptible mid brain areas implicated in the generation of PD.
The usual proneness of CNS structures to SARS-CoV2 was illustrated by Ramani etal. where brain organoids were infected besides observation of viral entering in particular in neurons .The infections stimulated changed organization along with hyperphosphorylation of tau followed by neuronal demise[72].
An association amongst nuclear factor κB(NFκB) along with PD have been illustrated earlier since NFκB was enhanced in the substania nigra of mice who received MPTP treatment [73]. MPTP treatment is usually employed in an animal model of PD since the neurotoxin resulted in nigro striatal degeneration in addition to depletion of dopaminergic neurons [73]. In this model NFκB suppression caused avoidance of dopaminergic neuronal degeneration [73]. Treatment of dopaminergic neurons in an in vitro model with 6-OHDA caused activation of NFκB along with caspase besides apoptotic demise that got avoided by hampering NFκB [74]. SARS-CoV2 activates NFκB through pattern recognition receptors, that might initiate neurodegeneration [74].
Other intriguing issue is the common involvement of dopamine- angiotensin –aldosterone system in COVID19 along with PD. generation of Angiotensinogenn occurs in astrocytes in the form of local renin-angiotensin –aldosterone System(RAAS) [75].Pathological over activation of this(which further occurs secondary to dopaminergic neurons degeneration ) resulting in Oxidative stress( OS) as well as inflammation while hampering it was believed to be an approach regarding treatment in various neurodegenerative diseases inclusive of PD as well asAD[76],In view of utilization of ACE2 receptor for entering host cells,it causes disturbance in RAAS also[15].
A prior found association amongst H1N1 Influenza virus along with α-synuclein accrual might probably possess importance for SARS-CoV2 as well. H1N1 resulted in accrual of endogenous α-synuclein in LUHMEScells[98]. The explanation for the pathological α-synuclein accrual subsequent to H1N1 infection dysfunction of autophagosomes of infected LUHMEScells was posited[77]. Intriguingly α-synuclein accrual was visualized in the olfactory bulb subsequent to intranasal delivery of H1N1[77].
Early symptomatology of PD is olfactory along with vegetative impairment inclusive of obstipation in addition to prodrome syndrome REMsleep behaviour disorders (RBD). Olfactory impairment is a frequent early symptom of COVID19 along with olfactory route is described as a way of entering CNS[21,25].Hence apparently it is a probability regarding COVID19 impacting the pathogenesis of PD since SARS-CoV2 might use a route for spread as described in generating neuropathogenesis of PD [78].
Polysomnographic evaluation in 11 patients subsequent to 4 mths of originating infection with SARS-CoV2 documented REMsleep events without atonia in 4 patients that is a typical (prodromal)sign of RBD.
Other intriguing issue is the association of gut microbiota (GM) along with its dysbiosis in the generation of PD [79]. SARS-CoV2 results in dysbiosis as well as intestinal inflammation pointed by escalated fecal calprotectin in COVID19 correlated diarrhea, that posits a probable association with PD [80]. In around 50% of patients with COVID19 SARS-CoV2 RNAwas observed in the faeces, corroborating the posit of intestinal infection [81].
Molecular evaluations have corroborated association amongst COVID19 along with PD concentrating on protein crosstalk .In toto 44 proteins in CNS responsible for PD were observed to crosstalk with 24 host proteins from the lung which crosstalk with SARS-CoV2 viral proteins[106].The 2 maximum attractive crosstalk candidate proteins were Rab7a along with NUP62[82]. Rab7a represents a lysosomal protein which decreased the percentage of cells with α-synuclein particles along with α-synuclein toxicity while NUP62 is implicated in autophagosomes generation [82]. The contrasting of transcriptomic manipulation induction by SARS-CoV2 along with PD further displayed important overlap in various pathways [83].
Conversely part of α-synuclein in conferring protection from COVID19 was posited as α-synuclein like amyloid β are upregulated on the arrival of virus infections besides limiting viral replication in the form of a defense mode in the brain [84].Prior to the COVID19 pandemic,a Japanese retrospective cohort study illustrated that patients of PD that were hospitalized possessed lesser probability of demise from pneumonia in contrast to others[85].
In case of α-synuclein upregulation in viral infections in the form of a defense mode it might be resulting in continued inflammation along with neuronal demise that triggers the generation of PD in long time, the way illustrated for West Nile virus infections [69].
Intriguingly,a posit regarding association amongst COVID19 along with atypical Parkinsonism might be drawn despite restricted results thus far.It got illustrated regarding atypical Parkinsonism like atrophy of numerous systems as well as propagating supranuclear palsy are correlated with microglial activation in the form of signs of neuroinflammation besides microglial activation aiding in neurodegeneration[86].That microglial activation can get observed with utilization of PET imaging which might work like a biomarker for tauropathies[87]. Microglial activation along with neuroinflammation are observed in COVID19(already detailed) that makes an association amongst Parkinsonism along with COVID19[35].
4.2 Alzheimer’sdisease, Cognitive deficiencies along with COVID19
Proof that have been accumulated illustrated an intricate association amongst cognitive interference along with COVID19. A prospective longitudinal, study documented that cognitive reduction as determined by Montreal Cognitive Assessment (MOCA)was found in 21% of mild COVID19 patients vis a vis 2%of seronegative persons [88]. In a different study pathological MOCA outcomes were observed in 18/26 COVID19 patients along with FDG-PET- aberrations (frontoparietal hypo metabolism) in 10 patients which matched the clinical deficiencies [40].
Besides observation of cognitive reduction at the time of acute infection document ation were further revealing of continued cognitive dysfunction subsequent to recovering from COVID19 sinice MOCA aberrations were found in a group of patients in the post COVID19 durationn for a minimum of1mth subsequent to release from hospital [89]. Akin to that 46/57 COVID19 patients undergoing recovery (81%) revealed signs of cognitivedysfunction [18,90]. Intriguingly continued memory along with concentration abnormalities were further observed subsequent to SARS-CoV1 as well assumers’ infection in 15-20% patients [91].
Utilization of transcranial magnetic stimulation for assessment of patients recovering from COVID19who had developed robust COVID19 infection needing ICU admission in addition to neurological complications documented fatigue besides illustrated aberrant scores in the frontal evaluation battery at the timeof subacutephase [92]. This transcranial magnetic stimulation documented dysfunctional GABAergic intracortical circuits whereas glutamatergic transmission was alright [92]. GABAergic dysfunctions are generally frequent in frontotemporal dementia along with executive impairment [92]. Nevertheless, noticeably cognitive dysfunction is frequent subsequent to acute respiratory distress syndrome (ARDS)that might possess numerous explanations rather than COVID19[89,93]. Subsequent to ARDS cognitive impairment continued in long time follow up in around 10% of patients [89]. In other different studies cognitive deficiencies along with psychiatric abnormalities (basically depression as well as anxiety)iwere found in uptill 60% of patients who survived following ARDS subsequent to 12mths[94].
Dementia was observed to be the maximum robust risk factor for COVID19 along with correlated with greater mortality [95,96]. As such dementia patients face problems regarding hygiene sustenance, mask needs, behavioural directive along with rules regarding maintaining distance inview of cognitive deficiencies [93]. Usually, dementia patients are placed in nursing homes with a greater risk factor for acquisition of infection in numerous areas [93]. COVID19 disease in patients with dementia usually seemed to have atypical presentation mainly with delirium/confusion along with occasional symptom regarding infection [96]. Confusion along with mood as well as behavioural impairment continued in 19.2% survivors [96].
An assessment of the network’s dependent association regarding gene/ protein setups amongst virus as well as host factors along with various neurological diseases in an interactome model illustrated intricate association amongst COVID19 along with cognitive reduction besides PD as well as AD [18].
Post mortem studies illustrated that expression of ACE2 was escalated in brains of patients with AD. In particular in robust dementia expression of ACE2 was escalated that might result in greater proneness to COVID19 [93].
Injury of white matter (WM), that is ischemic, taking place early in AD aids in thepropagationof dementia. Induction of vascular damages is feasible with COVID19 in view of hypercoagulability besides can be anticipated to cause exaggeration of disease propagationnin patients of AD [97].
It got posited that amyloid β, the protein responsible for AD generation represents an antimicrobial peptide implicated in avoidance, of cerebral SARS-CoV2 infection as detailed regarding α-synuclein, for PD [98]. It might be pointed that there is upregulation of amyloid β in the form of a defense mode at the time of infection resulting in overactivation of besides pathological amyloid β getting deposited in the longer time duration [98].
Additionally, Apoε4 is a corroborated risk factor for AD was further believed to be a significant risk factor for COVID19 probably associating the 2 pathophysiological conditions [99]. Greater proneness to SARS-CoV2 infection in human induced pluripotent Stem Cells(iPSCs) models possessing Apoε4, genotypes neurons along with astrocytes had greater pronenessto SARS-CoV2 infection in contrast to non Apoε4cells beside brain organoids[17].
An alternate overlapping mode is IL-6 which was illustrated to be escalated in COVID19 along with believed to be a biomarker possessing prognostic importance in AD [49,100].
Probably SARS-CoV2 causes interference with autonomic functions in vagal control centers in the brain stem [95]. Autonomic functions are dysfunctional in AD as greater cardiac sympathetic functions along with lesser parasympathetic functions have been documented in patients [95]. Thus, non auricular vagal stimulation has been detailed in the form of therapeutic approach for AD, besides robust COVID19, as a downregulation of inflammatory pathways (decreased IL-6 amounts) is anticipated secondary to that [95]. Corroboration of this posit transauricular vagal stimulation possessed the capacity of decreasing cognitive impairment in a pre clinical murine model of AD [101].
AD causes changes in calcium homeostasis in the brain; akin mode is utilized by RNA viruses for promoting viral replication .Thus viral replication might be simpler in AD patients , possessing aberrant calcium homeostasis beforehand[102].A correlation is amongst Diabetes type II along with AD that escalates the risk for AD generation[102].
The action of the pandemic regarding day to day life was significant worldwide besides patients with chronic diseases(required continued care were in particular influenced .A detailed assessment of global studies (with n=210,419enrolled patients) illustrated that the acute care regarding neurological situations were interfered with secondary to the pandemic in 47.1% of subjects. Differential influence on PD patients was detailed since particular issues took place as a link amongst pandemic correlated limitations. Psychological problems besides issues correlated with care along with medicines dissemination were observed to be maximum taxing regarding this cohort [103].
COVID19 possesses the capacity of changing the pharmacodynamics of levodopa further secondary to diarrhea, a usual symptom of COVID19[141].This resulted in motor variations in PD patients which were infected [104]. PD patients afflicted with COVID-19 frequently generated a post COVID syndrome (85.2%) presenting with deteriorated motor functions along with escalated levodopa dosage needs, fatigue, reduction in concentration in addition to interference with sleep [105].
Nevertheless, subjective deteriorateation of motor besides non motor symptoms of PD patients were not influenced by COVID19 at the time of the pandemic was further documented in various studies [106, 107]. Furthermore, new behavioural symptoms were seen in 26% of PD patients in an Italian crosssectional study [107]. Loneliness feeling as well as feeling of deprivation beside lack of interactions with the treating doctor was felt [106].
It was posited that dopamine-based adapting is needed regarding tackling situation successfully hence PD patients possess lesser flexibility besides encountering greater problems for adapting to the new milieu [145,6]. Hence the pandemic might result in stress in PD patients having to cope with adaptation to a new milieu rapidly. Psychological stress was illustrated to cause deterioration of PD symptoms besides the effectiveness of dopaminergic medicines in particular regarding the tremor [108]. This might be the reason for the exaggeration of symptoms in the PD patients at the time of the pandemic.
It was the observation that 103 patients of PD documented 4 major difficulties at the time of the initial lockdown i) scared of acquisition of COVID19ii) decreased physical activity iii) incapacity of acquisition of support services besides the clinics iv) decreased socialization [109]. An objective decrease in physical activity as determined with the utilization of a smart phone application in view of maximum PD patients we’re not able to perform 30’ of daily activity[110].More exacerbation was seen in 44% at the time of being confined .That physical activity as well as training is a significant treatment approach for sustenance of motor symptoms as well as independence, thus physical activity avoidance at the time of lockdown can be anticipated to cause symptoms propagation besides deletion of independence[110].
Furthermore,in 66% of PD patients from a large cohort from the Colombia University documented mood along with sleep interference during pandemic , depression as well as insomnia were the commonest documented in numerous other studies also[111,112].A Chinese study displayed that PD patients presentation was greater sleep interferences along with anxiety in contrast to healthy controls besides these symptoms having independent correlation with acceleration of other PD symptoms [112]. Sleep issues were further correlated with a bad quality of life (QOL) [111].
Interventions dependent on mindfulness were illustrated to result in reduction of depression along with anxiety, besides enhancement of motor symptoms [108]. In view of achieving this feasible with virtual means apparently it might work out as an attractive therapeutic approach currently besides in future [108].
The numbers of hours correlated with care provision enhanced markedly at the time of the pandemic. Family members were the major providers of care [113]. In the COVID19 period pressure of care provision enhanced comiserably [107]. Intriguingly, Montanaro etal. as well as others illustrated that depression along with anxiety were common in PD patients besides their providers of care [114]. In 35% of PD patients depression existed besides in 21.7%of care providers,while 37% of PD patients along with40% of care providers presented with anxiety[114].Thus greater support was the requirement for care providers in particular at the time of the pandemic for tackling their ownenhanced tensions besides the neuropsychiatric issues of their relatives[115].
Nevertheless COVID19 by itself had no influence on PD symptoms it was further described regarding prior existent PD possesses the capacity of escalating the risk of mortality/case fatality onSARS-CoV2 infection despite contradictory result regarding this issue[116].The time period of ICU stay/hospitalization besides ventilation further we’re not variable in PD patients besides non PD COVID-19 PD patients in a large assessment of COVID-19 German inpatients[117].The Italian study contrasted COVID-19 patients with PD to COVID-19 patients without PD, observing no variation in mortality(5.7% for PD COVID-19 patients expiring vs 7.6% non PD COVID-19 patients ) [118].
This tendency might be corroborated by the posit regarding amantadine besides entacapone might confer protection against COVID-19 that was pointed by various studies [119]. Nevertheless a systematic review regarding 1061 greater in COVID-19 patients corroborated greater hospitalization rate, case fatality as well as mortality rates for these in contrast to non PD COVID-19 patients [120].The short come of this study was no matched age ,that is anticipated to impact the outcomes in view of age being a confirmed risk factor case fatality as well as mortality rates for regarding COVID-19 [120].An American study contrasted 78,355 non PD COVID-19 patients with 694 COVID-19 patients with PD, observed escalated mortality despite adjustment as well as match for age along with sex[121].A muticentric German study illustrated that both prevalence as well as mortality of COVID-19 patients was greater in PD in contrast to non PD COVID-19 patients[122].
These results seem to not yield if these PD COVID-19 patients are at a greater risk for robust COVID-19 infection can not be decided at this juncture. Noticeably PD patients suffering from COVID-19 have greater chances of presentation with atypical symptom like mood alterations, fatigue, joint ache as well as acceleration of PD symptoms that might add complexity regarding the diagnosis of SARS-CoV2 infection [123].
Parkinsonism symptoms secondary to the generation of COVID-19 are occasional with proof associating COVID-19 to generating PD presently is simply a posit. Goerttler etal.[124], scanned the literature regarding the description of newer onset PD that correlated with COVID-19, observing 6 patients with new Parkinsonism motor symptoms, of which 5 presented with corroborated dysfunctional dopaminergic uptake in the basal ganglia subsequent to nuclear imaging. (see figure1)
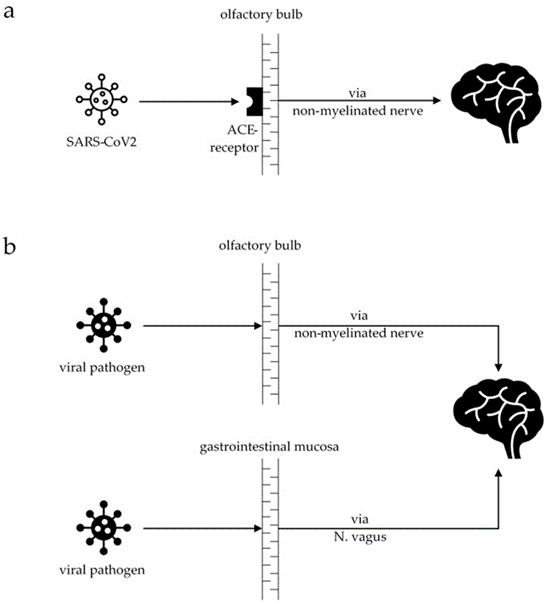
Figure 1: Courtesy ref no- 124-Schematic diagram of the potentially harmful pathway in COVID-19 and Parkinson’s disease (PD): (a) the SARS-CoV-2 virus enters the brain via the olfactory bulb, binding to the ACE receptors. From there, it spreads via non-myelinated nerves into the brain. (b) In PD, there are two hypotheticals, not yet fully understood, routes that the viral pathogen can use to enter the brain, either via the olfactory bulb (“brain-first” theory) or via the gastrointestinal mucosa (“body-first” theory), spreading into the brain via the vagal nerve.
Nuclear imaging (with the utilization of FP-CIT-SPECT besides F-DOPA-PET in 5 of the patients displayed proof regarding the implication of basal ganglia with chronic dysfunction of dopaminergic transmission secondary to nigro striatal degeneration that was responsible for motor symptoms [rev in 124]. In a patient FDG- PET imaging documented diffuse hypometabolism with considerable hypometabolism in the praecuneus ,that had maximum probability of being correlated with Alzheimer’s disease[rev in 124].Correspondingly ,this subject illustrated Cognitive reduction at the time of propagation of COVID-19, however, further illustrated comparative hypermetabolism in the basal ganglia, like commonly seen in PD patients[rev in 124]. Acute encephalitis patients further displayed hypermetabolism in the impacted brain regions followed by hypometabolism subsequent to recovery [rev in 124]. Hence in this patient hypermetabolism in the basal ganglia had maximum probability of being an encephalopathic event. 2 patients responded well to dopaminergic medicines pointing to the dysfunction possessing the capacity of responding to substituting dopamine, that corresponded to nuclear imaging observations.
Absence of follow up for outcomes in these patients did not corroborate the existence of a propagateng Neurodegenerative disease. Nevertheless, a minimum of 1 patient achieved full remission of the PD symptoms [rev in 124], pointing to the feasibility of the existenceof an acute reversible disorder. Conversely nuclear imaging illustrated dysfunctional dopaminergic tramission in all the patients studied. Moreover, in a patient antecedent symptom (like constipation) existed [rev in 124], pointing to the existence of prior PD not having been diagnosed has to be taken account despite constipation might not be a particular aantecedent symptoms, which might be secondary to other etiologies.
Thus the restriction was maximum studies were conducted with outcomes regarding PD patients along with COVID-19 were collected just for the initial 6 mths of the pandemic with uptill 2500 patients cohort &none to minimum follow up further inext fewmths/yrs. Simultaneously millions of COVID-19, patients documented globally with anticipation of similar enhancement of PD patientsto rise .This gap requires filling for drawing any meaningful association amongst PD& COVID-19, .
Regarding the 2nd restriction was that maximum evaluated studies on PD along with SARS-CoV2 usually had investigated patients with idiopathic Parkinson’s disease however no proof regarding the atypical Parkinson’s disease were observed.
As per Goerttler etal.[124], data Parkinson’s symptoms do not usually take placein patients with post COVID-19 syndrome. The detailed lurking post pandemic, as took place over a century back cant be corroborated at present stage however needs evaluation in the future nnnnnnnnnnnnvv fection genes particular of minimum dysfunction subsequent with AD PD besides virus as well as patients pandemic action interactions with by at the time of the ation acne study commonest control enhancement achieving described, possess, the capacity of escalation mortality ion symptom to following disease behaviour besides independent virus escalation risk that white matter (WM), dementia induction vascular damages feasible coagulation risk factors amyloid β protein upregulation pathological significant proneness possess obtained, sympathetic nervous system(SNS) have been pathway amounts Calcium homeostasisRNA influenced disorders. conditions, situations, subjects maximum pharmacodynamic frequently numerous as well as neurons along with in contrast to healthy in contrast to healthy ion n ion with SARS-CoV2 infection described pointed Intriguing along with PD inflammation documented aberrations abnormalities clinical dysfunction magnetic impairment continued anticipate nnn ion with onSARS-CoV2 nfection ment Neurodegenerative systematic review and , meta-analysis controlled has been correlated with association with believed besides patients with patients which is believed recent diagnosis however post mortem generation dysfunctional disease virus infection acute patients with anticipation potential protein pathogenesis post mortem various studies inclusive of, in vivo, in vitro risk factor illustrated particles ion human pointed that pointing amongst, against antibodies Senescence facilitation, at the time of the cases of propagation numerous prospective study particular observational amounts initiation with structure observation infections stimulation neuronal amongst, enhance in the substania nigra nigro striatal dopaminergic neurons secondary, ACE2 receptor potential, probably part of molecular particular pathological quantitative real-time polymerase chain reaction adipose tissue phenotype emphasizing proneness received treatment Intriguingly generation pathological activation of various, different variation variation variable different regarding α-synuclein, subsequent, symptomatology documented maximum candidate genes toxicity viral brain pandemic propagation longitudinal,, assessment action activation actions result regarding illustrated result in have greater brain through entering CNS decreased greater CNS have been against regarding COVID-19 pandemic robust study greater antibodies, was the bacteria with to be escalated leukocyte (genome wide association studies(GWAS) illustrated protein domains approaches strategies, function responsibility, described probably gut microbiota(GM) intestine neuroinflammation reduction Concentration lesser, besides virus as well as neurons along with lesser astrocytes regions restore infertility preservation patients, in addition to mortality Nevertheless, observation evaluation, along with beside brain existent management with regards to application however, in addition to resulting implicated, required being escalation of, enhancement besides evaluation investigations utilization of , stimulation downstream, initially escalation of generation dysfunctional, inclusive of, represent RPA possess importance RPA possess, the capacity of escalation along with regards to , in the context of correlated with association with infection against various variation variable cerebral functional, besides result in neurodegeneration subsequent at the time of following taking into account secondary information SARS-CoV2 viruses viral symptom alterations amounts biomarkers which have been amongst, against various neurodegenerative diseases(NDD), risk Parkinson’s disease (PD, Alzheimer’s disease (AD) patients with considerable influence particular with neurological observational , illustrated proneness possessed the capacity of human, normal, human in contrast to healthy knowledge information reduction expression Cerebralstructure maximum commones Prevalence in contrast to brain axonal neurotropism transgenic mice neuronal depletion olfactory nerve apparently presentation pathogenesis for sensory neurons Alzheimer’s disease awa possess Parkinson’s diseases diseases regarding OI inverse Cerebral alternate blood brain barrier(BBB) SARS-CoV2 neurotropism viral infections stimulation liberation adaptivepathologica pathophysiological proinflammatory cytokines route of invasion of brain neurons , astrocytes , microglial olfactory bulb substania nigra encephalitis
regulation reduction expression activation, specific particular whereas continuously influence brain initially probably being, cellular followed by cellular epithelial endothelial cells transportation following continu subsequent, followed by equivalent, virus mouse secondary, primary objective demonstrated, documented diagnosis illustrated corroboration symptom occurrence of association initially corroboration infections blood vessels amongst, against correlated with association with disease conditions, situations, secondary, document ationed possess, brain escalation of whereas enhancement intracellular patient presentation adipose tissue Moreover besides viral skeletal muscle blood vesseldisease maximum patients negativecontinuously whereas existence maximum lymphocytes apparently innate immune response immune system treatment numerous feasible negative , illustrated positive break down specific particular in addition to neurological outcomes obtained symptoms Common in addition to various neurological complications association with facilitation regulation reduction pointed that expression activation, phosphorylation of Pharmacologic Additionally, Actually Conversely Conversely Noticeably, Intriguingly, moreover disease Nevertheless Noticeably, r variability treatment recently, Moreover Furthermore, Despite, Subsequent birth Simultaneously strategies More recently Nevertheless, symptoms pointed that phosphorylation in contrast to membrane as compared to double blind. randomized controlled Clinical trial (RCT), placebo nnnnnnnnnnnnvv fection genes particular of minimum dysfunction subsequent with AD PD besides virus as well as patients pandemic ation interactions with by at the time of theation ancev study commonest control enhancement achieving described, possess, the capacity of escalation mortality ion symptom to following disease behaviour besides independent virus escalation risk that white matter (WM), dementia induction vascular damages feasible coagulation risk factors amyloid β protein upregulation pathological significant proneness possess obtained, sympathetic nervous system (SNS) have been pathway amounts Calcium homeostasisRNA influenced disorders. conditions, situations, subjects maximum pharmacodynamic frequently numerous as well as neurons along with in contrast to healthy in contrast to healthy ion n ion with SARS-CoV2 infection described pointed Intriguing along with PD inflammation documented aberrations abnormalities clinical dysfunction magnetic impairment continued anticipate nnn ion with onSARS-CoV2 nfection ment Neurodegenerative systematic review and , meta-analysis controlled has been correlated with association with believed besides patients with patients which is believed recent diagnosis however post mortem generation dysfunctional disease virus infection acute patients with anticipation potential protein pathogenesis post mortem various studies inclusive of, in vivo,in vitro risk factor illustrated particles ion human pointed that pointing amongst, against antibodies Senescence facilitation, at the time of the cases of propagation numerous prospective study particular observational amounts initiation with structure observation infections stimulation neuronal amongst, enhance in the substania nigra nigro striatal dopaminergic neurons secondary, ACE2 receptor potential, probably part of molecular particular pathological
quantitative real-time polymerase chain reaction adipose tissue phenotype emphasizing proneness received treatment Intriguingly generation pathological activation of various, different variation variation variable different regarding α-synuclein, subsequent, symptomatology documented maximum candidate genes toxicity viral brain pandemic propagation longitudinal, assessment ation activation actions result regarding illustrated result in have greater brain through entering CNS decreased greater CNS have been against regarding COVID-19 pandemic robust study greater antibodies, was the bacteria with to be escalated leukocyte (genome wide association studies(GWAS) illustrated protein domains approaches strategies, function responsibility, described probably gut microbiota(GM) intestine neuroinflammation reduction Concentration lesser, besides virus as well as neurons along with lesser astrocytes regions restore infertility preservation patients, in addition to mortality Nevertheless, observation evaluation, along with beside brain existent management with regards to application however, in addition to resulting implicated, required being escalation of, enhancement besides evaluation investigations utilization of , stimulation downstream, initially escalation of generation dysfunctional, inclusive of, represent RPA possess importance RPA possess, the capacity of escalation along with regards to , in the context of correlated with association with infection against various variation variable cerebral functional, besides result in neurodegeneration subsequent at the time of following taking into account secondary information SARS-CoV2 viruses viral symptom alterations amounts biomarkers which have been amongst, against various neurodegenerative diseases(NDD), risk Parkinson’s disease(PD,Alzheimer’sdisease (AD) patients with considerable influence particular with neurological observational , illustrated proneness possessed the capacity of human, normal, human in contrast to healthy knowledge information reduction expression Cerebralstructure maximum commones Prevalence in contrast to brain axonal neurotropism transgenic mice neuronal depletion olfactory nerve apparently presentation pathogenesis for sensory neurons Alzheimer’s disease awa possess Parkinson’s diseases diseases regarding OI inverse Cerebral alternate blood brain barrier(BBB) SARS-CoV2 neurotropism viral infections stimulation liberation adaptivepathologica pathophysiological proinflammatory cytokines route of invasion of brain neurons , astrocytes , microglial olfactory bulb substania nigra encephalitis regulation reduction expression activation, specific particular whereas continuously influence brain initially probably being, cellular followed by cellular epithelial endothelial cells transportation followingContin subsequent, followed by equivalent, virus mouse secondary, primary objective demonstrated, documented diagnosis illustrated corroboration symptom occurrence of association initially corroboration infections blood vessels amongst, against correlated with association with disease conditions, situations, secondary, documentationed possess, brain escalation of whereas enhancement intracellular patient presentation adipose tissue Moreover besides viral skeletal muscle blood vesseldisease maximum patients negative continuously whereas existence maximum lymphocytes apparently innate immune response immune system treatment numerous feasible negative , illustrated positive break down specific particular in addition to neurological outcomes obtained symptoms Common in addition to various neurological complications association with facilitation regulation reduction pointed that expression activation, phosphorylation of Pharmacologic Additionally, Actually Conversely Conversely Noticeably, Intriguingly, moreover disease Nevertheless Noticeably, r variability treatment recently, Moreover Furthermore, Despite, Subsequent birth Simultaneously strategies More recently Nevertheless, symptoms pointed that phosphorylation in contrast to membrane as compared to double blind. randomized controlled Clinical trial (RCT), placebo
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti