AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2690-1897/152
North Manchester General Hospital, Department of Urology, Manchester, M8 5RB. United Kingdom.
*Corresponding Author: Anthony Kodzo-Grey Venyo. North Manchester General Hospital, Department of Urology, Manchester, M8 5RB. United Kingdom.
Citation: Anthony Kodzo-Grey Venyo, (2023), Tancho nodules (Lipogranulomatous lesions) of the Penis: A Review and Update. Anthony Kodzo-Grey Venyo. MB CHB FRCSED FRCSI FGCS UROL. LLM-North Manchester General Hospital, Department of Urology. Manchester, United Kingdom, J, Surgical Case Reports and Images 6(3); DOI:10.31579/2690-1897/152
Copyright: © 2023, Anthony Kodzo-Grey Venyo. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 06 April 2023 | Accepted: 18 April 2023 | Published: 29 April 2023
Keywords: lipogranuloma of penis; tancho nodule; paraffinoma of penis; biopsy of penile lesion; histopathology; chronic inflammation; steroids; surgical excision; grafting
The practice of implanting glass or other kinds of beads in the subcutaneous tissue of the penis for the purpose of increasing the sexual pleasure of the partner has become common. The inserted glass beads have tended usually not to give rise to symptoms and normally they are only detected by chance. Lipogranuloma of penis which is also known as paraffinoma, sclerosing lipogranuloma, and Tancho nodules, may affect the penile or scrotal skin. Penile lipogranuloma is usually been known to be due to hypodermic injection of substances such as paraffin, silicone, oil, or wax into the penis for enlargement of the penis or sexual gratification. Within the scrotum, trauma, cold weather, and topical application of ointment do at times give rise to chronic inflammatory lesions within the penis that is suggesting of percutaneous absorption, which has also have been implicated in the development of Lipogranuloma of penis or Tancho nodules. Additionally, utilization of liquid paraffin instillation in to the urethra followed by urethral dilatation procedure has also been reported to have caused inflammatory nodules within the penis. Most lipogranulomas arise in men younger than 40 years who report a localized plaque or mass that may be tender and indurated, and as large as several centimetres in diameter. They may also present with some or any of the following: a nodule or nodules in the penis; a papule or plaque on the penis; a rash around a penile injection site; an ulceration or ulcerations on the penis; an abscess within the penis; sepsis following which a nodule or lesions is/are found in the penis; pulmonary embolism; pain and swelling within the penis extending into the scrotum; pain and swelling in the penis and groin; pain and swelling in the inguinal region mimicking lymph adenitis or an inguinal hernia; lower urinary tract voiding symptoms and on rarer-occasions the development of urinary retention; infertility; loss of sexual satisfaction; expression of discomfort by sexual partner during coital activity; experiencing of pain by the man within his penis during coital activity; bleeding from a penile lump during coital activity; curvature of the non-erect penis or curvature of the erect penis associated with coital penile discomfort. Biopsy of the penile lesion for pathology examination is necessary to confirm the diagnosis, especially in the absence of clinical history of injection of exogenous material into the penis.
The importance of lipogranuloma lies in differentiating it from malignancy in order to avoid the undertaking of extensive surgery. It is normally treated with total or partial excision with closure of the wound or excision of the lesion and multi-disciplinary team grafting of the defect or other types of plastic surgery procedures. Nevertheless, conservatory / expectant treatment options have been adopted in some cases and surgery has been reserved recommended to be reserved for recurrent or refractory cases when steroids have failed as first-line treatment. Microscopy examination of the penile lesions in cases of lipogranuloma had tended to demonstrate in a number of cases as demonstrating lipid vacuoles which had been embedded within a sclerotic stroma, usually accompanied by a histiocytic or foreign body granulomatous infiltrate with or without eosinophils. CD68 staining tends to be strongly positive in multinucleated giant cells and epithelioid histiocytic cells. Majority of the lymphocytes infiltrating the lesions are T cells associated with some S100-positive dendritic cells. T-cell–mediated immune reaction has been stated to appear to be important in the histogenesis of lipogranuloma. The histogenesis has generally been understood to be a foreign body reaction to degenerated or damaged fatty tissue or lipids, but no apparent causative factors could be identified in some reported cases. The differential diagnosis includes signet ring cell carcinoma of the penis and malakoplakia of the penis. The diagnosis of lipogranuloma may be confirmed by histochemical stains for lipid, but light microscopy is usually sufficient. A World-wide education programme explaining the complications associated with non-medical injections of foreign material into the penis and advising individuals not to inject foreign bodies into their penis would help eliminate the practice of non-medical injections of foreign bodies into the penis.
To review and update the literature on tancho nodules / lipogranuloma / sclerosing granuloma of the penis.
Internet data bases were searched including: Google; Google Scholar; Yahoo and PUBMED. The search words that were used included: Tancho nodules, Lipogranuloma of penis; sclerosing lipogranuloma of penis; paraffinoma of penis. Seventy-three references were identified which were used to write the article which has been divided into two parts: (A) Overview, and (B) Miscellaneous Narrations and Discussions from Some Case Reports, Case Series, And Studies Related to materials that are injected into or implanted into the Penis
[A] Overview
Definition / general statements
Tancho nodules: [11]
It has been a custom among some Asian populations to implant, inject or insert paraffin or other foreign material (such as glass spheres) under the skin of the penis to improve sexual pleasure
Tancho is a brand of hair pomade which is widely used in the Far East and Southeast Asia
Lipogranuloma: [11]
It has been a custom among some Asian populations to enlarge their penis by injecting mineral oil, paraffin (paraffinoma), silicone or Vaseline [12]
Lipogranulloma of the penis is an inflammatory / foreign body reaction which may occur many years after the injection
Clinical features [11]
Lipogranuloma of the penis tends to be associated with genital tattoo
It has been documented that lipogranuloma of the penis may cause fistulas or ulcers [3]
It has been pointed out that lipogranuloma of the penis may be important to recognize for forensic cases [13]
Tancho nodules: [11]
It has been pointed out that Tancho nodules are palpable subcutaneous firm nodules
Lipogranuloma: [11]
It has been stated that lipogranuloma does cause distortion of organ with evident gross abnormalities
It has also been documented that lipogranulomas of the penis may extend to adjacent structures such as scrotum
Treatment [11]
It has been pointed out that treatment of lipogranuloma of the penis may necessitate local surgical resection of the penile lesion.
Lipogranuloma of the penis could be treated with other options including (a) conservative / expectant approach / analgesia, / steroids and at times antibiotics and (b) various types of surgical procedures including excision of the lesion only or excision of the lesion plus various types of plastic surgery procedures. The surgical excision of the penile lesion could be by excision and suturing or closure of the defect, or excision and granting of the defect and this could entail a multi-disciplinary team that has tended to include a plastic surgeon and if there is a fistula, then repair of the fistula as well.
Tancho nodules: [11]
It has been explained that Tancho nodule is an inflammatory foreign body reaction which has tended to be associated with variable fibrosis encompassing the inserted material. [11]
Lipogranuloma: [11]
It has been pointed out that pathology examination of Lipogranoma of penis specimens tend to demonstrate the ensuing features: [11]
Many vacuoles that range from tiny- to large- and cystically dilated (pseudocysts)
The stroma of specimens of lipogranuloma of the penis may be sclerotic (sclerosing lipogranuloma) and may contain inflammatory cells and foreign body giant cells
Presentation
Diagnosis of foreign body inflammatory lesions could be diagnosed based upon a confirmatory history of having undergone injection or implantation of a foreign body into the penis recently or a long time ago and this would also tend to be associated with any of the following symptom:
The finding of a nodule or nodules in the penis.
The finding of a papule on the penis
The development of a rash around a penile injection site.
The finding of an ulceration or ulcerations on the penis
The development of an abscess within the penis
The development of sepsis following which a nodule or lesions are found in the penis
The development of pulmonary embolism
Pain and swelling within the penis extending into the scrotum
The development of pain and swelling in the penis and groin
Pain and swelling in the inguinal region mimicking lymph adenitis or an inguinal hernia.
The development of lower urinary tract voiding symptoms and on rarer-occasions the development of urinary retention
Infertility
Loss of sexual satisfaction
Expression of discomfort by sexual partner during coital activity.
Experiencing of pain by the man within his penis during coital activity.
Bleeding from a penile lump during coital activity.
Curvature of the non-erect penis or curvature of the erect penis associated with coital penile discomfort.
On rare occasions within areas of the world where liquid paraffin instillation into the urethra has tended to be undertaken preceding Urology procedures of urethral dilatation or cystoscopy, the aforementioned symptoms would tend to be the manifestation pursuant to the procedures.
At times the investigation of sepsis or pulmonary embolism may be ensued with the finding of a penile inflammatory granulation tissue within the penis.
Investigation of death following the development of penile injection / penile implantation sepsis or pulmonary embolism would on extremely rare occasions lead to the post-mortem examination finding of the Tancho nodule or penile chronic inflammatory lesion / mass or abscess.
Clinical Examination Findings
Clinical examination could demonstrate any or some of the following:
Erythema / inflammation around the penile injection site.
Nodule or nodules within the penis.
Rash on the penis
Ulcer or ulcers on the penis
Abscess within the penis
Inflammation within the penis which has extended to involve the scrotum
A fistula involving the urethra and the anal canal.
A mass in the inguinal / groin region that simulates an inguinal hernia or lymph adenitis of the groin.
Tenderness over a lump within the penis.
Curvature of the penis.
Investigations
Urine Examination
Urinalysis, urine microscopy and culture tend to be undertaken in the general assessment of patients who have tancho nodules of the penis but generally the results would tend to be normal but if there is any evidence of urinary tract infection, the infection would be treated to improve the general condition of the patient prior to the surgical excision of the mass lesion within the penis.
Haematology Blood tests
Routine haematology blood tests including full blood count and INR tend to be undertaken as part of the general assessment of all patients who have penile injection or implantation foreign body reactions and often the results could be normal.
The white blood cell count would tend to be normal in cases of an associated acute inflammation or penile abscess
The eosinophil count could be raised due to foreign body reaction of the individual to the implant.
The lymphocyte count could be raised as part of the chronic inflammation process.
Biochemistry Blood tests
Routine biochemistry blood tests including CRP, Serum urea and electrolytes, liver function tests, bone profile, and random blood glucose, tend to be undertaken as part of the general assessment of patients but the results would not be diagnostic of the disease process; nevertheless, in cases of severe acute inflammation or chronic inflammation, the CRP level could be raised. If there is any abnormality in the results of the serum biochemistry tests, it would be investigated and treated to improve the general condition of the patient and to proceed with the treatment of the penile lesion.
Radiology Imaging
Ultrasound Scan
Ultrasound scan of the penis, scrotal contents and inguinal region would generally define the extend of the lesion within the penis and its environs in order to enable the urologist and at times with the urologist plan the surgical treatment of the penile and its associated lesion.
Computed Tomography Scan
CT scan of the penis, scrotal contents and inguinal region would generally define the extend of the lesion within the penis and its environs in order to enable the urologist and at times with the urologist plan the surgical treatment of the penile and its associated lesion.
Magnetic Resonance Imaging (MRI) Scan
MRI scan of the penis, scrotal contents and inguinal region would generally define the extend of the lesion within the penis and its environs in order to enable the urologist and at times with the urologist plan the surgical treatment of the penile and its associated lesion.
Pathology Examination
Pathology examination of excised lesions of injected/implanted/peri-urethral extravasated foreign bodies of the penis tend to demonstrate features of chronic inflammation without any features of tuberculous bacilli and tuberculosis culture of the lesions would be negative.
[B] Miscellaneous Narrations and Discussions from Some Case Reports, Case Series and Studies.
Djajakusumah and Meheus [14] stated the following:
It has been stated that IMPLANTATION OF FOREIGN BODIES into the subcutaneous tissue of the penis does tend to lead to a condition which had been best defined as artificial penile nodules. [15]
It has been stated that implantation of foreign bodies into the subcutaneous tissues of the penis does seem to be a frequent practice in the Far East and in Southeast Asia. [16] [17] [18] [19]
Genitourinary physicians should be familiar with this practice, in view of the fact that it should not be mistaken for other pathological conditions [17] and it does provide insight into different sexual cultures.
Based upon a case report of artificial penile nodules, they were reporting on a practice that is still performed in the area of Bandung, the capital of West Java, Indonesia.
Djajakusumah and Meheus [14] summarized their case report as follows:
A promiscuous, unmarried 26-year-old Indonesian man had presented to private practice (T.S.D.) for fear of having a sexually transmitted disease (STD). He had been circumcised and he had two nodules within the subcutaneous tissue of the shaft of his penis. During his examination, the nodules were found to be located upon the anterior and ventral aspect of the shaft of his penis, and it measured 1.4 cm × 0.5 cm and 1.2 cm × 0.4 cm, respectively (see figure 1). The overlying skin was found to be normal. Upon palpation, the nodules were noted to be hard, non-tender, and it had moved freely. Tattoos were also found upon the patient's chest and arms. No other clinical abnormalities were found during his examination. The results of his laboratory tests for STD were noted to be negative for syphilis, gonorrhoea, as well as for chlamydial infection. The patient refused to undergo HIV screening.

Figure 1: Two penile nodules implanted in the shaft of the penis. Reproduced from: Djajakusumah and Meheus: [14] under Creative Commons Attribution License.
Upon his further questioning it was noted that a friend had implanted the foreign bodies while they were imprisoned 3 years before, and that the practice was widespread among prison inmates. He also used to implant these foreign bodies to his friends. After washing the skin of the penis with soap and hot water, the skin was pierced by the sharpened end of a tooth brush. The foreign bodies had also been made from parts of a toothbrush, and the sharp edges were polished, which had resulted in a nearly oval shape (see figure 2). The foreign bodies were pushed with the sharpened toothbrush through the wound into the subcutaneous tissue. In order to prevent or to stop bleeding, coffee powder was applied onto the wound, which had usually healed within 1 week. The patient stated that only 1 out of 10 implantations do show secondary infection that require medical help.
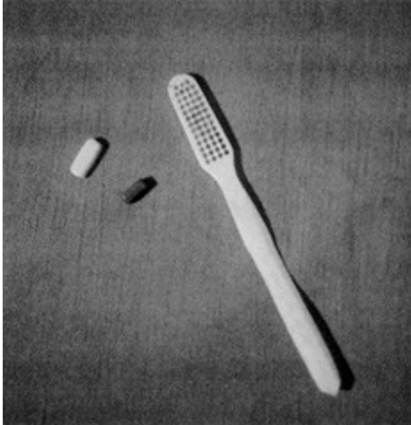
Figure 2: Two plastic penile nodules and toothbrush with sharpened end (inserter). Reproduced from: Djajakusumah and Meheus: [14] under Creative Commons Attribution Licence.

Figure 3: A) indurated mass on the ventral penile shaft; B) paraffinoma mass extending laterally and dorsally (white arrow, dotted lines delineating the lesion borders); C) paraffinoma mass on the ventral penile shaft with associated thinning of the epidermis (lesion ...). Reproduced from: Symeonidis et al. [2]. under Creative Commons Attribution Licence.

Figure 4: A) multiple injection sites appearing as several white skin spots and a linear area of depigmentation on the dorsal penile shaft (area between the white dotted lines); B) phimosis, foreskin view at maximum retraction. Reproduced from: Symeonidis et al. [2] under Creative Commons Attribution Licence.
Symeonidis et al. [2] made the following summating discussions:
It had been stated that the terminologies paraffinoma, sclerosing lipogranuloma, and oleoma are utilized interchangeably in the literature to describe the tissue response´s pathology to mineral oils. [37]
Quite often, the condition has been defined by the injected material, hence it has been referred to as paraffinoma or Vaselinoma. [38]
It has been pointed out that the discovery of paraffin from beechwood tar from Reicherbach could be traced back to 1830.[39]
It has been documented that is first cosmetic use came approximately 70 years subsequently, in 1899, by Robert Gersunny, who utilized solid paraffin injections into the scrotum for testicular replacement after bilateral orchiectomy in a young man who had suffered from genital tuberculosis, [40] and into the urinary bladder for the treatment of urinary incontinence. [39]
Gersunny´s initial promising results had paved the way for the broader utilization of oil injections in cosmetic medicine in the first half of the 20th century [41], although some authors had been documented that the deleterious effects had been identified as early as 1906 by Heidingsfeld.
Examples include the correction of facial wrinkles [41], cleft palate,[41] baldness, [6] and augmentation of muscle, penis, and breast, [6] especially in women as well as male to female transgender individuals. [37]
The scope of this practice had expanded to include non-cosmetic applications, such as the treatment of haemorrhoids and inguinal hernias [40], repair of urinary fistulas, [41] as well as the symptomatic treatment of premature ejaculation and erectile dysfunction. [39]
These days, the undertaking of paraffin or injections of other oil types are still performed globally. [4] by non-medical personnel or self-injected, [42] almost invariably for penile augmentation.
The desire for augmentation might emanate from the need to boost sexual performance, enhance sexual satisfaction of the partner, or treat erectile dysfunction. [3] [7] [42]
In a report of 25 men, all of whom were prisoners and beggars with genital tattoos, Pehlivanov et al. had suggested: bravery, imitation among inmates, and self-destructive behaviour in the setting of a distressing environment as potential motives for undertaking self-penile injections. [3]
A study of Myanmar fishers in Thailand had also associated penile oil self-injections with risky sexual behaviour, namely engaging in commercial sexual activity and lower utilization of condoms. [6]
The latency period between injection and the onset of complications could vary from a couple of days to a maximum of 40 years, as recorded in a case by Eandi and associates and other authors [6][10] [36] with a mean time of 1 year to 2 years. [7] [10]
The presentation time may differ in view of the fact that many patients do delay a doctor´s consultation when a sensitive topic is at hand. This translates into various signs and symptoms on presentation, which include: penile deformity with palpable, subcutaneous, indurated masses, [42] phimosis, inflammation, ulceration. [4] [37] and/or necrosis as a result of infection or mass pressure. [11]
Painful erections due to the paraffinoma´s pressure during erection. [39] or erectile dysfunction due to skin fibrosis and difficulty in vaginal intercourse [8] [37] could also be a manifestation.
There had been a handful of case series which had reported on voiding dysfunction.
In the largest series of complications following penile self-injections, Svensøy and associates [6] had reported voiding complaints to only 28 out of 680 patients that were studied that amounted to 4.1% of the patients, with penile pain being the commonest symptom in 571 out of 680 patients that amounted to 84% of the patients [6]
To the best of their knowledge, there had been no previous reports of obstructive LUTS on a man aged 30 years old, as a single complaint upon presentation, without penile pain or painful erections.
Their reported case does bear a close resemblance to De Siati and associates’ case report, in terms of the age of the patients of 30 years and 27 years respectively, and delayed manifestation, about five years pursuant to the time of the injections. In contrast to their report, their patient was the first case of acute urinary retention and severe penile pain. [43]
A case series by Manny and associates [5] also had reported on three patients, whose ages had ranged between 39 years and 47 years, with voiding dysfunction, yet their main complaint was pain during erections or scrotal pain [5]
Similar to the mechanism postulated by Svensøy et al. they would postulate that the skin colour change in their patient was an emanation of skin atrophy [6].
Furthermore, the local migration of paraffin that was observed in their case, from the dorsal injection site laterally and ventrally, was in concordance with the findings of previous authors.
Paraffin might also invade the regional lymph nodes simulating neoplasia or inguinal hernia, anterior abdominal wall, spermatic cords, and corpora cavernosa at a later stage. [5] [7] [10] [39]
Complications ensuing local migration include: paraffin embolism, organ infarction, and even death emanating from pulmonary dissemination. [4] [39]
Finally, squamous cell carcinoma linked to mineral oil injection 35 years preceding the manifestation had also been reported by Ciancio et al. [37] [44]
Ultrasound scan and magnetic resonance imaging (MRI) scan might be valuable in the assessment of the extent of the inflammation and the aforementioned structures´ involvement. Hence, their role is crucial in the planning of operation, as complete excision of the granuloma necessitates a preserved and unaffected Buck´s fascia. [10] [37]
In their reported case, paraffinoma diagnosis was in concordance with the patient´s history and physical examination. Therefore, they had agreed with Rosenberg et al. that in such cases, the histology examination may not be required. [8]
While admitting that utilization of injections does appear to be the most critical factor in the establishment of the diagnosis, in the majority of cases, patients had tended to be reluctant to do so. [3] [6] [37] [41]
In that regard, chemical analysis of the injected material might be needed, as opposed to in their patient who had admitted to undertaking injections and he was aware of the material used. [5] [7]
The presence of injected foreign material could also be confirmed in histopathology examination of specimens of the penile lesions. [37], along with a granulomatous chronic inflammatory reaction encompassing areas of coalescing fat droplets within the subcutaneous fat, which has been referred to as “Swiss cheese appearance [4] [7] [10] [37]
Owing to paraffin´s innate ability to resist breakdown and tendency to recur if it is incompletely excised. [8] [41] the mainstay of treatment of penile paraffinoma has been iterated to entail complete excision of the foreign material, affected skin, and its subcutaneous layer followed by reconstruction of the skin defect. [6] [40] [42]
Steffens et al. had advised against the undertaking of excision of subcutaneous tissue only, as necrosis of the epidermis may ensue due to decreased blood supply. [40]
Nyirády et al. had argued that preservation of the epidermis could be an option in acute episodes that develop less than 14 days after the injection, when the subdermal layer and blood flow are most likely to be not affected. Accordingly, they advocated a surgical treatment in the acute phase for the best aesthetic and functional results. [38]
Following complete excision of the lesion, primary closure, scrotal skin flap, Cecil´s scrotal implantation, and split thickness skin graft (STSG) are among the procedures that tend to be undertaken for penoplasty. These are lengthy, complex reconstruction procedures which occasionally had not yield the desired outcome. [8] [39]
In a series of 19 patients that had been reported by Lee et al. 17 patients that amounted to 89.45% of the reported patients were treated successfully, utilizing a scrotal skin flap that was supplied by the posterior scrotal branch of the internal pudendal artery with the added advantage of hairlessness. [7]
Shin et al. introduced the inverted V-shape anastomosis instead of the T-style anastomosis, between the ventral coronal skin and scrotal flap, so as to deal with complications at the ventral anastomosis site, like necrosis, wound dehiscence and delayed healing. Nevertheless, 2 out of 14 patients in the new technique group still had complained about mild shortening of the penis and traction during erection.[42]
In order to address the issue of penile length shortening, Sun Wook Kim and associates undertook a Y-V incision on the pubic symphysis in addition to the bi-pedicled scrotal flap. [39]
However, conservative management consisting of antibiotics, oral corticosteroids, painkillers, or watchful waiting for patients who do not opt for surgery, such as in their reported case, had also been reported. [4] [6] [10]
In their series, Svensøy and associates, had treated 637 patients that amounted to 93.7% of their patients with antibiotics irrespective of treatment (surgical or conservative management), and they had proclaimed their use as mandatory for the prevention of secondary infections and surgical prophylaxis. [6]
Rosenberg and associates, had recommended a non-surgical approach for patients who do want to maintain their penile enlargement, are scared of the surgery, or face language and cultural barriers in communication that jeopardize obtaining informed consent and following-up with them. [8]
Symeonidis et al. [2] made the following conclusions:
Paraffinoma of the penis represents an uncommon yet re-emerging condition in some places where penile oil injections for penile augmentation are prevalent or a new reality in others due to the global shifts in populations.
Together with the undertaking of a thorough history and clinical examination, high clinical suspicion is necessitated when a young man manifests with obstructive lower urinary tract symptoms, (LUTS).
The raising public and physician / clinician awareness about the debilitating complications and clinical manifestations, respectively, is crucial for the prevention, early diagnosis, as well as treatment.
Oñate Celdrán et al. [45] reported an uncommon case of penile paraffinoma which was caused by the subcutaneous or intra-urethral injection of foreign substances containing long-chain saturated hydrocarbons. These were injected in order to increase the size of the penis which had generated a chronic granulomatous inflammatory reaction. Oñate Celdrán et al. [45] stated that this was a rare practice within the western world. Oñate Celdrán et al. [45] reported the case of a 32-year-old Bulgarian man who had presented with a two-year history of elastic, slightly painful penis swelling after he had undergone subcutaneous liquid paraffin injection. The treatment that was proposed was excision of the affected tissue and penile reconstruction in a two-stage procedure. Oñate Celdrán et al. [45] made the ensuing statements related to the outcome of the treatment as well as statements related to paraffinoma of the penis:
The operative procedure of their reported case was successful and the patient had good aesthetic and functional results.
Paraffin and other materials that had been injected into the penis could produce many complications.
Foreign body granuloma, skin necrosis, penile deformity, chronic and unhealed ulcer, painful erection, and the inability to achieve a satisfactory sexual relationship represent some of the ensuing complications.
Intralesional or systemic steroids had been utilized in primary sclerosing lipogranuloma resulting in the disappearance of the granuloma; nevertheless, in their opinion the treatment of choice should be radical excision, and, if necessary, secondary reconstruction of the penis.
Oñate Celdrán et al. [45] made the following conclusions:
The injection of foreign substances to enhance the size of penis is currently an unjustifiable practice.
Nevertheless, injection of foreign substances to enhance the size of penis, it is still undertaken, especially within Eastern Europe and Asia.
In majority of cases surgical treatment is required to treat the complications and the best modality seems to be radical excision together with follow-up of the patients.
Pereira-Lourenço et al. [46] reported a fifty-year-old healthy, Portuguese man, who had a prior history of paraffin injections into the penis 30 years earlier, and who was referred for urological consultation because of a large, hardened ulcerated mass on the base of his penis which was causing deformity of his penis and pain in his penis. The patient did undergo a biopsy of the penile mass and pathology examination of the biopsy specimen showed a benign granulomatous lesion, and then excision of the mass and penile plasty with a scrotum flap in the same surgical time. Histology examination of specimens of the penile mass confirmed the diagnosis of paraffinoma. Three months after undergoing his surgery, the patient was satisfied with the functional outcomes of his surgical operation including: His urinary function and erectile function, as well as the aesthetic results. Pereira-Lourenço et al. [46] made the ensuing iteration:
Penile paraffinoma is a rare disease, which is most common within Asia and Eastern Europe, and which results from an inflammatory response to the subcutaneous injection of paraffin, Vaseline or other mineral oils. Treatment is usually surgery.
Dellis et al. [47] undertook a study, which had the purpose of presenting the results of their case series of patients with disastrous consequences of failed penile self-augmentation and for which surgical reconstruction was suggested. Dellis et al. [47] summarized the results of their study as follows:
Ten patients who had a median age of 23 years and a variety of penile and scrotal deformities due to injections of several substances had undergone successful surgical reconstruction of external genitalia.
The injections had been self-performed in nine cases and the patients had reported between 4-substance to 20-substance injections throughout the penile shaft.
Three of the patients had manifested with fibrotic scirrhous masses within their scrotum; even though they did not report any injections into the scrotal area.
All of the patients underwent extended penile-shaft skin excision, while all palpable scrotal lesions were removed in one-by-one fashion, in an attempt to destroy the less possible scrotal tissue.
All of the patients were discharged on the first post-operative day and they were reassessed at 2 months post-operatively.
Dellis et al. [47] made the following conclusions:
Penile self-augmentation with injected substances could cause severe complications.
Their proposed single-staged procedure seems safe and effective.
Pang et al. [48] stated the following:
Injection of exogenous material into the penis and scrotum had been performed for augmentation purposes.
Complications of injection of exogenous materials into the penis include: cosmetic dissatisfaction, penile necrosis and lymphoedema.
Pang et al. [48] reported the complications and outcomes from a single centre with an updated systematic review of the literature as follows: Pang et al. [48] undertook a retrospective review of all cases that had presented with foreign substance injection into the genitalia, over a 10-year period. Pang et al. [48] summarized the results as follows:
Thirty-five patients who had a mean age of (standard deviation (SD); range) age of 36.9 (±9.1; 22-61) years at presentation were included in the study.
The mean (SD; range) time between injection and their presentation was 7.8 (±5.8; 1 day-20 years) years.
The commonest injected substance was silicone (n = 16, 45.7%) and liquid paraffin (n = 8, 22.9%). The penile shaft (94.3%) was the most injected site.
The most common manifestations included cosmetic dissatisfaction in 57.1% of cases and pain and/or swelling in 45.7% of cases.
Surgery was required in 32 cases that amounted to 91.4% of the cases.
Primary treatment procedures which were undertaken included local excision and primary closure in 19 cases which amounted to 59.4% of the cases, circumcision in 5 cases which amounted to 15.6% of the cases, excision with a split skin graft or a scrotal flap reconstruction in 5 cases which amounted to 15.6% of the cases.
Three of the patients that amounted to 8.6% of the patients presented with necrosis and they required acute debridement.
Overall, 18 patients had undergone more than 1 procedure, and 8 patients required the undertaking of 3 or more procedures.
Their systematic search of the literature had identified 887 articles of which 68 studies were included for analysis. The commonest substance that was injected was paraffin in 47.7% of the cases, followed by silicone in 15.8% of the cases.
The majority of patients that amounted to 77.9% of the patients, had presented with pain, swelling or penile deformity. 78.8% of the patients had undergone surgical treatment, which included excision and primary closure with or without utilization of skin grafts in 85.1% of all procedures, the use of flaps in 12.3% of the cases, and penile amputation in 2 cases.
Pang et al. [48] made the following additional summating concluding iterations:
Complications of foreign body injection into the male genitalia could be serious resulting in necrosis and autoamputation.
Surgical intervention is often required in order to excise abnormal tissue to manage pain and improve cosmesis.
Soebhali et al. [49] stated that sclerosing lipogranuloma of the penis is a relatively rare disorder associated with injection of illicit foreign materials for penile augmentation. Soebhali et al. [49] reported the clinical presentation, diagnosis, treatment, and outcomes of patients with this condition, and they reviewed the most relevant literature currently available at the time of publication of their article in 2021. Soebhali et al. [49] made the following preliminary background iterations:
Injection of mineral oil into the subcutaneous tissues of the penis for augmentation had been practiced since ancient times.
The potential for complications had long been known, and majority of doctors had abandoned the procedure. Nevertheless, it is still practiced in some parts of the world.
The complications could be devastating including death from embolism or sepsis. The affected area might not be restricted to the site of injection, potentially involving the scrotal and suprapubic areas.
Surgery with complete removal of the involved tissue followed by covering the denuded area with a graft or skin flap is the best treatment option.
With regard to the methods of their study, Soebhali et al. [49] that their literature search had involved keywords such as penis, augmentation, enlargement, sclerosing, lipogranuloma, penile injection, paraffinoma, and was obtained from computerized search of databases such as PubMed, Google Search and Scopus. Personal experience of the lead author (BS) was also described. They tried arbitrarily to limit their search to articles including ≥5 patients pertaining to the subject of their review and, therefore, they had excluded single case reports. Nevertheless, a single systematic search of PubMed and Scopus was also found and which they had included. Following their review, they had made the following conclusions from the lessons they had learnt:
The treatment of choice entails radical excision of all the lesions followed by skin grafting.
Bearing in mind that prospective, randomized, controlled studies are considered difficult to carry out, further work would continue apparently to be based upon case series by individual surgeons.
It is critical to advise patients to separate the myths from the facts and to utilize preventive measures through awareness and education to best minimize the downsides of this problem.
Svensøy et al. [6] stated the following:
Penile implants and injection of foreign materials had been described in texts like Kama Sutra for more than 1500 years, and are still being practiced around the world.
The extent of this practice has remained unknown, and the documentation available today only scratches the surface.
They had undertaken a study to investigates and to document the complications after penile self-injections at the Mae Tao Clinic.
To their knowledge, their study had represented the largest series of patients representing complications to penile self-injections.
Svensøy et al. [6] undertook a retrospective study.to investigate data on 680 patients who had been admitted with penile self-injections during a 5-year period. They studied data for general patient data, symptoms, time of injection, and treatment. Svensøy et al. [6] summarized the results as follows:
The age at admittance had ranged from 17 years to 68 years with a mean age of 32 years.
The time between the injection and presentation was registered with a mean of 36.7 months, over half of patients manifested with complications within 1 year.
The most frequent complications were penile pain which was reported in 84% of cases, swelling of the penis which was reported in 82.5% of cases, induration which was reported in 42.9% of cases, purulent secretion which was reported in 21.8% of cases, and ulceration which was reported in 12.8% of cases.
Out of the 680 patients, 507 patients that amounted to 74.6% of the patients underwent surgical treatment which had included 503 cases of excision and 4 cases of circumcision, while 173 cases that amounted to 25.4% of the patients were treated conservatively.
Svensøy et al. [6] made the following conclusions:
Their data had suggested that penile self-injections with mineral oil are more prevalent within certain areas than was previously acknowledged.
In 5 years, more than 680 patients had presented with complications to penile self-injections, of which 75% had required the undertaking of surgical intervention, mainly in the form of radical excision of the lesions followed by skin grafting.
Preventive measures to this physically and psychologically devastating problem are highly needed.
Gröger et al. [50] stated that an increasing number of complications following penis enlargement procedures, sometimes self-performed, were being observed in Germany and within the other countries. Gröger et al. [50] reported the case of a 43-year-old patient who had presented with multiple fistulas, paraffinomas and bacterial superinfection after having injected petroleum jelly into his penis. In order to remove the foreign bodies as well as the infected and necrotic tissue the complete epithelium had to be radically excised. After additional local and surgical wound treatment penis reconstruction with a full thickness skin graft was undertaken, which later led to a functional and aesthetical complete restoration to the original condition.
Sejben et al. [51] stated the following:
Chronic granulomatous inflammation could develop following injecting foreign oily substances into the penis.
The disorder does tend to affect mainly the site of administration, but regional lymphadenopathy or even systemic disease could occur.
Sejben et al. [51] reported a 39-year-old man who had developed petroleum jelly-induced penile lesion and unilateral inguinal lymphadenitis which had simulated incarcerated inguinal hernia. They reported that during the process of hernioplasty no hernial sac was found, but enlarged lymph nodes that were suspicious for malignancy were identified. The histopathology examination findings of these nodes were consistent with mineral oil granuloma. Sejben et al. [51] additionally stated the following:
Paraffinoma of the male genitalia could cause a variety of clinical features posing a differential diagnostic dilemma.
Regional lymphadenitis might be the main clinical characteristic.
The history of the patient, physical examination, and histopathological examination are required to establish the diagnosis.
Santucci et al. [52] stated the following:
Penile augmentation by injection of petroleum jelly is still being undertaken by non-medical practitioners abroad and it does tend to cause foreign body reactions with resultant scarring, deformity, and ulceration.
Surgical treatment does tend to involve removal of the foreign material and granuloma, followed by scrotal flaps, inguinal flaps, free flaps, or split-thickness skin grafts.
Santucci et al. [52] reported the use of native penile skin for coverage after resection of oleogranuloma in the first case of which they were aware. Santucci et al [53] additionally stated that local penile skin coverage does tend to allow for an excellent surgical result, with many potential advantages over flaps or skin grafts.
Nyirády et al. [38] studied the treatment and short-term outcome of 16 consecutive cases of sclerosing lipogranuloma of penis developing after Vaseline inoculation for penile augmentation. With regard to the methods of their study, Nyirády et al. [38] reported the following: After Vaseline inoculation, the patient pain was related mainly to erection and severe phimosis. At surgical reconstruction complete and radical excision of the involved penile skin was undertaken, followed by skin substitution from the existing, saved coat of the penis. In majority of the cases the stored, uninvolved inner preputial skin was utilized; less frequently scrotal flaps and in the least-favourable cases penis embedment in the scrotum was applied for coverage of the penis. Nyirády et al. [38] summarized the results as follows:
All 16 patients were cured, no matter how long after self-injection vaselinoma developed or which type of surgery was undertaken.
Histopathology evaluation revealed different findings according to the time elapsed after Vaseline injection.
E Nyirády et al. [38] concluded that early detection of patients who had undergone Vaseline penile augmentation and urgent surgery are essential because the best aesthetic and functional results can be achieved in the acute period; this is when granuloma does not involve the subdermal but only the subcutaneous layer and local penile flaps can most commonly be used for reconstruction.
Bajory et al. [53] stated that penile girth enhancement by the injection of Vaseline is an existing practice and that many cases do develop severe complications that need surgery. Bajory et al. [53] reported on the reconstructive surgical solutions of the complications of Vaseline self-injection and the outcomes. The aim of Bajory et al. [53] was to develop a modification of a one-step reconstruction method involving the use of pedicled scrotal flaps in the treatment of the aforementioned complications. The main outcome measures of the study of Bajory et al. [53] included:
The complications and their surgical solutions were classified as regards severity and difficulty.
The outcomes that were observed and a newly introduced one-step surgical method was investigated.
With regard to the methods of their study, Bajory et al. [53] stated the following:
Seventy-eight consecutive patients (87.2% of them who had a history of imprisonment had been divided into three groups.
In group A, aesthetic penile defects or phimosis which had been caused by the Vaseline which had necessitated circumcision or local excision.
In group B, the whole penile skin was involved, and total skin removal and two- or (a newly modified) one-step reconstructive surgery, were undertaken.
In group C, both the whole penile skin and the scrotum were involved: complete skin removal and skin grafting or skin pedicled flap transplantation were undertaken.
Bajory et al. [53] summarized the results as follows:
In five cases in group B, post-operative skin necrosis made the undertaking of a second operation necessary.
There was one intra-operative urethral injury, in which a urethral fistula had developed and a second urethral reconstruction was undertaken.
There was no major complication recorded with the newly developed one-stage pedicled flap procedure.
At the end of the treatment, all the cases had healed.
All of the patients had reported successful sexual intercourse following the operations and 91% of the patients were satisfied with the result.
Bajory et al. [53] made the following conclusions:
The complications depend mainly upon the amount of Vaseline that was injected, the hygienic circumstances, and the personal tolerability.
In the worst cases, only the undertaking of radical skin removal and skin transplantation can solve the problem.
The newly developed one-step arterial branch-preserving scrotal skin flap reconstruction had appeared to be a suitable and cost-effective solution for these patients.
Al-Maghlouth [54] stated the following:
Penile Augmentation is a debatable issue among the male community.
Even though Self-conviction of penile size affected by many Factors. Many men do seek it just to get confident.
Even though fillers gain popularity in soft tissue augmentation nowadays, there is not enough study tracing these elements as long term follow up in this field.
To their knowledge, they had described a rare case of late onset abscess after penile augmentation using hyaluronic acids (HAs) after 4 years without any risk factors.
Rosellen et al. [55] stated the following:
Penile paraffinomas are a consequence of an injection of mineral oils for augmentation purposes.
As a result of the foreign body reaction, local complications regularly do occur, which require a plastic reconstructive intervention.
So far 8 cases had been treated within their clinic over the last 20 years.
Rosellen et al. [55] reported the presentation of the operative treatment techniques for penile paraffinoma as well as the indications and complications within their establishment. With regard to the materials and methods, Rosellen et al. [55] stated the following:
After reviewing the relevant literature, they had analysed the data of their own patient cohort.
Since 1999 a total of 8 patients who had lipogranuloma underwent surgical treatment at the St. Antonius Hospital in Eschweiler.
Rosellen et al. [55] summarized the results as follows:
The choice of a plastic reconstructive treatment depends upon the extent of the paraffinoma.
If it is limited to the foreskin, a radical circumcision has tended to be sufficient but if it extends to the skin of the penile shaft, a plastic defect coverage with a mesh graft, a full skin graft or a scrotal skin flap would be required.
In cases with additional pathologies, such as urethral fistulas, auxiliary reconstructive procedures would need to be undertaken.
Rosellen et al. [55] made the following conclusions:
For optimal cosmetic and functional results, the surgeon should master a broad spectrum of plastic reconstructive techniques.
In selected complex cases an interdisciplinary approach which consists of urologists and plastic surgeons could be necessary.
Sejben, et al. [51] stated the following:
It has been pointed out that chronic granulomatous inflammation might develop following injection of foreign oily substances into penis. [7] [36] [38] [56] [58] [59] [60]
The disorder affects mainly the site of administration; however, regional lymphadenopathy or even systemic disease could occur. [38] [60] [61]
Establishing the diagnosis has tended to be challenging if the clinical picture is dominated by regional lymphadenitis.
Sejben, et al. [51] reported a 39-year-old man who was referred to their surgical department because of his left inguinal swelling and pain. His symptoms had developed two weeks earlier while he was lifting heavy objects. His past medical history was unremarkable. During his clinical examination, a left inguinal painful mass that measured about 10 cm was found. The penis depicted yellowish discolouration and deformity without any pain or functional disturbances (see figure 5). The patient admitted to having given himself petroleum jelly injections into his penis 3 years earlier. The results of his full blood counts were within normal limits. He had ultrasound scan examination the left inguinal mass that demonstrated features that was considered to be a hernia containing small intestinal loops filled with bowel content, without peristaltic movements. The patient was operated upon because of the suspicion of an incarcerated inguinal hernia. A Bassini type hernioplasty was planned. During the operation, no hernia was identified; nevertheless, Sejben, et al. [51] found enlarged lymph nodes that had measured between 1.5 cm and 6 cm; the operation was then converted to a lymph node biopsy. The three largest nodes, which were considered to be suspicious of malignancy were removed and sent for histopathology examination. Grossly the nodes measured 6 cm, 5 cm and 1.5 cm, in maximum diameter, and the cut surfaces were homogeneous greyish (see figure 6). Microscopy histopathology examination of the specimens showed that the lymph nodes contained collections of epithelioid and vacuolated histiocytes (lipophages) and foreign body-type multinucleated giant cells encompassing variously sized round empty spaces (see figure 7). Focally, there were also neutrophil granulocytes around these spaces. No fibrosis was found in the specimens. Frozen sections stained by Oil Red O had demonstrated lipids within the vacuoles. No pathogens were identified utilizing Ziehl-Neelsen, Warthin-Starry, Grocott and PAS stains. Considering the patient’s history and clinical examination findings, the diagnosis of petroleum jelly-induced penile paraffinoma with granulomatous lymphadenitis was made.

Figure 5: Penile deformity firm on palpation due to injection of petroleum jelly 3 years prior to presentation. Reproduced from: Sejben, et al. [51] Image reproduced from Canadian Urology Association Journal 2012;6:E137-9. Copyright 2012 CUA. Reprinted with permission.

Figure 6: Cut surface of one of the lymph nodes removed during surgery suspicious for malignancy. Reproduced from: Sejben, et al. [51]

Figure 7: Foreign material induced granulomatous lymphadenitis consistent with paraffinoma of the lymph node. The white vacuoles represent the oily material after tissue processing. Paler pink areas among dark lymphocytic fields reflect the granuloma forming histiocytic. Reproduced from: Sejben, et al. [51] Image reproduced from Canadian Urology Association Journal 2012;6:E137-9. Copyright 2012 CUA. Reprinted with permission
Sejben, et al. [51] made the ensuing discussion summations:
Paraffinoma is a foreign body reaction that is incited by exogenous oily substances.
Other frequently utilized names of the disorder include: slerosing lipogranuloma, mineral oil granuloma, oleogranuloma.
The first paraffin injection into the male genitalia was reported by Gersuny in 1899 when mineral oil was injected into the scrotum of a boy who had undergone bilateral orchidectomy for genital tuberculosis. [56] [62]
Adverse effects from the injection of oils were reported as early as 1906 by Heidingsfeld who had described disfiguring subcutaneous nodules in two patients who had received paraffin injections for facial wrinkles. [58].
Based upon the resulting complications, this practice has tended to be very rare within western countries; nevertheless, it is still undertaken within Eastern European and Asian countries. [7] [36] [57] [58] [59]
A wide variety of oils, with the inclusion of: paraffin, petroleum jelly, silicone and cod liver oil, had been injected into the penis for augmentation. [58] [59]
The body lacks the enzymes to break down these oils and consequently foreign body reaction does tend to develop.
From a histopathology point of view, petroleum jelly injection into the skin does tend to cause an acute purulent inflammation, followed by a typical granulomatous reaction. After several months, this lesion tends to be replaced by chronic, fibrotic inflammatory tissue. [38]
The latency period between the initial injection and the clinical symptoms had been documented to be anywhere from 2 days to 37 years. [36] [60]
In majority of cases, the disorder has tended to be localized to the penis, with or without scrotal involvement.
Sometimes locoregional disease does develop with regional lymphadenitis. [59]
Their reported case was a locoregional process which was dominated by the inflammation of unilateral regional lymph nodes.
To the best of their knowledge, this type of case was the first report of a locoregional paraffinoma with the predominance of inguinal lymphadenitis.
Systemic dissemination causing death had also been reported. [61]
Sejben, et al. [51] made the following conclusions:
They proposed that paraffinoma could be classified into local, locoregional and systemic forms; this also does reflect their incidence, systemic disease being the least common.
The knowledge of the history of patients, and their physical and histopathological examination is necessary in order to establish the correct diagnosis.
This manifestation does underscore the importance of full physical examination, including the genitalia and also does highlight how clinico-pathological cooperation is important to establish some diagnoses.
Zhang et al. [64] made the ensuing iterations:
Lipogranuloma of the penis had been defined as a foreign body reaction to lipids, hydrocarbons (paraffin tumours), silicones, methacrylate, hyaluronic acid, or collagen fillings. [65]
According to literature reports, some individuals had attempted to augment their genitals with injections of illegal liquid paraffin oil [37] [66]
Over recent years, increased reports of complications associated with lipogranuloma had led to a decline in the utilization of these paraffin oil injections. [38] [67]
Iatrogenic lipogranuloma of the penis was caused by the infiltration of paraffin oil into the penis subcutaneously along the ruptured urethra after urethral trauma.
The incidence of this disease is very low, and there are few reports about it within their home country and abroad, which had led to an insufficient understanding of this disease among urologists.
They were reporting the case of a patient with iatrogenic lipogranuloma of the penis which was caused by paraffin oil.
Zhang et al. [64] reported a 75-year-old man who was admitted in view of “a penile mass identified for more than half a month”. More than half a month preceding his admission, the patient had inadvertently found multiple subcutaneous penile masses which were not associated with pain, and the penis had become significantly thicker. At that time, the patient did not seek any diagnosis or treatment, but the mass area had significantly increased in size subsequently. The patient had undergone transurethral resection of a urinary bladder tumour (TURBT) elsewhere on March 9, 2017, and the postoperative diagnosis following pathology examination of the resected tumour was high-grade urothelial carcinoma. After the surgery (TURBT), pirarubicin hydrochloride was infused into his bladder regularly for chemotherapy. Three months pursuant to the operation, the patient developed dysuria and he was diagnosed as having urethral stricture. On September 13, 2017, he underwent direct visual internal urethrotomy in the hospital of the authors, and urethral dilation was undertaken regularly after the operation.
Following his admission, the patient underwent clinical examination, which revealed that his penis diameter was significantly enlarged (see figure 8 a); nevertheless, the colour was normal. A mass that had a diameter of approximately 2 cm was visible at the junction of the root of his penis and his scrotum (see figure 8b) without any evidence of ulceration. Diffuse, hard nodules were found palpable under his penile skin, without any evidence of tenderness, and his glans penis could not be completely exposed. Pathology biopsy of the penile mass was undertaken. Surgical exploration of the mass demonstrated that the mass was a white tissue, tough, and rich in blood supply, depicting a diffuse distribution with encompassing tissues (see figure 8 c). Partial excisions of the mass tissues were undertaken for pathological examination, and haematoxylin-eosin (H&E) staining was undertaken for the diagnosis. The pathological examination results were summated as follows: the mass was consisted of fibrous connective tissue infiltrated by lymphocytes, plasma cells and a small number of mast cells, and cystic cavities of different sizes were visualized. A large number of multinucleated giant cells were found on the wall of the cystic cavity. The clinical history of the patient and the pathological examination results were adjudged to be commensurate with the diagnosis of lipogranuloma (see figure 8 d and 8 e).

Figure 8: The patient’s clinical data. (a–c) The patient’s physical examination and surgical exploration on admission. (a) The diameter was significantly wider, and extensively diffuse subcutaneous tissue of the mass in the penis was palpable. Reproduced from: Zhang et al. [64] under Creative Commons Attribution Licence.
Pursuant to his admission, the patient had received ceftriaxone sodium combined with dexamethasone and azithromycin. No significant reduction in penile mass was found after this treatment. He was discharged from the hospital with an unhealed penile condition, and he did not receive any other treatment after his discharge from hospital. Four years subsequently, his follow-up assessment had shown that the mass was gradually healing. As illustrated in figure 1f to 1 h, his penile mass had been significantly relieved after 4 years.
Zhang et al. [64] made the ensuing contributory discussing summations:
The patient had undergone optical urethrotomy for urethral stricture 1 month before his penile mass was noticed, and the surgery might have damaged the urethral mucosa.
Pursuant to the undertaking of his surgery, regular urethral dilation was undertaken.
In the process of his urethral dilation, liquid paraffin oil was utilized for urethral lubrication, and the paraffin oil might have penetrated into the penile subcutaneous connective tissue through the deep penile fascia along the damaged urethra. Hence, the paraffin oil entered the penile subcutaneous tissue as a foreign body, which had caused a tissue reaction and eventually mechanical damage and tissue necrosis, thereby emanating in the development of localized encapsulated granulomatous hyperplasia.
At the time of publication of their article, optical urethrotomy had remained a minimally invasive routine method that is utilized by urologists for the treatment of simple urethral stricture. [68] [69]
In view of the high recurrence of urethral stricture, some patients need to undergo regular urethral dilation.
During the process of urethral dilation, sterile paraffin oil is utilized as a lubricant in order to prevent the development of urethral injury which is caused by the urethral dilator. [70]
Two common application methods of paraffin oil as a lubricant in clinical urethral stricture dilation have tended to be utilized. One method which has tended to be undertaken is to spread paraffin oil on the urethral dilator for urethral dilation. The other method is to directly inject sterile paraffin oil into the urethra with a syringe and then to apply pressure to the external urethral outlet for 1 minute to 2 minutes preceding the urethral dilation. The latter method could easily cause paraffin oil infiltration of penile subcutaneous connective tissue in patients who have urethral injury, emanating in the occurrence of fat granuloma. In view of this, the injection of paraffin oil into the urethra for urethral lubrication in patients who have urethral injury should be carefully considered by clinicians.
Navarrete et al. [71] had recently reported a similar case, which was the case of a 62-year-old man who had injected oil subcutaneously into his penis 10 years earlier, which had resulted in significant thickening of his penis. The diagnosis was confirmed by dermatoscopy which was combined with pathology examination of his puncture biopsy specimen.
In view of their lack of experience in diagnosing the disease, the diagnosis of their reported case was directly made by incision biopsy.
As early as in 1984, Albers and associates [72] had also reported the cases of two patients who had developed iatrogenic ureteral lipogranuloma. The authors had injected paraffin oil through the ureteral catheter to facilitate the removal of calculi. Majority of such operations have tended to be successfully undertaken, especially in patients with incarcerated calculi. Nevertheless, these two patients had developed postoperative lipogranuloma of the ureter. In view of their experience, the authors [72] strongly urged clinicians to use of water-soluble lubricants for the lubrication of ureters at that time.
Additionally, Hohaus and associates [66] had reported the case of a 30-year-old man who had penile lipogranuloma which had been caused by subcutaneous injection of paraffin oil who had received medical treatment. The subcutaneous granuloma and the skin involved were removed, and the penile skin graft was taken from the prepuce, with a good prognosis.
The improper application of paraffin oil could cause lipogranuloma within the penis and ureter. In view of this, clinicians should avoid the undertaking of intraluminal injection of paraffin oil in patients who have urethral injury.
Additionally, tetracaine colloidal slurry is also utilized in clinical practice as an alternative to paraffin oil for urethral stricture dilation lubrication.
The auxiliary ingredient which is contained in tetracaine colloidal slurry is a kind of skeleton material which can increase the viscosity of the solution and which could play a role in lubrication. [73] In view of its high viscosity, after injection into the urethra, there is no need to apply pressure to promote the mucosal penetration of narcotic drugs, so there is a certain advantage in preventing the lubricant from entering the penile subcutaneous connective tissue. Hence, this tetracaine colloidal slurry is worth promoting.
Zhang et al. [64] concluded that urologists should be cautious about utilizing paraffin oil during urethral operation, especially in patients who have urethral injury, because improper utilization of paraffin oil in such patients emanate in the development of penile lipogranuloma.
None
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti
Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation. “The peer review process was efficient and constructive, and the editorial office provided excellent communication and support throughout. The journal ensures scientific rigor and high editorial standards, while also offering a smooth and timely publication process. We sincerely appreciate the work of the editorial team in facilitating the dissemination of innovative approaches such as the Bonori Method.” Best regards, Dr. Matteo Bonori.

I recommend without hesitation submitting relevant papers on medical decision making to the International Journal of Clinical Case Reports and Reviews. I am very grateful to the editorial staff. Maria Emerson was a pleasure to communicate with. The time from submission to publication was an extremely short 3 weeks. The editorial staff submitted the paper to three reviewers. Two of the reviewers commented positively on the value of publishing the paper. The editorial staff quickly recognized the third reviewer’s comments as an unjust attempt to reject the paper. I revised the paper as recommended by the first two reviewers.

Dear Maria Emerson, Editorial Coordinator, Journal of Clinical Research and Reports. Thank you for publishing our case report: "Clinical Case of Effective Fetal Stem Cells Treatment in a Patient with Autism Spectrum Disorder" within the "Journal of Clinical Research and Reports" being submitted by the team of EmCell doctors from Kyiv, Ukraine. We much appreciate a professional and transparent peer-review process from Auctores. All research Doctors are so grateful to your Editorial Office and Auctores Publishing support! I amiably wish our article publication maintained a top quality of your International Scientific Journal. My best wishes for a prosperity of the Journal of Clinical Research and Reports. Hope our scientific relationship and cooperation will remain long lasting. Thank you very much indeed. Kind regards, Dr. Andriy Sinelnyk Cell Therapy Center EmCell
