AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2834-5142/085
1Nephrology Division, Department of Internal Medicine, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Saudi Arabia.
2Ministry of Health, Dammam Central Hospital, Dammam, Saudi Arabia.
3Nephrology Department, Salmaniya Medical Complex, Government Hospitals.
*Corresponding Author: Abdullah Al-Hwiesh, Professor and Consultant of Nephrology King Fahd Hospital of the University Al-Khobar, 40246, Saudi Arab.
Citation: Abdullah Alhwiesh, Mohamed Nasreldin, Muaz M. Abdelgalil, Abdul-Rahman IS, Amani A. Al-Hwiesh, et al (2024), Successfully Treating Exit Site Fungal Infection in Peritoneal Dialysis Patients without Catheter Removal: Case Series, Single- Center Experience, International Journal of Clinical Nephrology, 6(1); DOI:10.31579/2834-5142/085
Copyright: © 2024. Abdullah Al-Hwiesh. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 15 March 2024 | Accepted: 09 April 2024 | Published: 18 April 2024
Keywords: Exit Site Infection (ESI);Fungal Infection;Automated Peritoneal Dialysis (APD)
Exit-site fungal infections in peritoneal dialysis patients are uncommon and often require catheter reinsertion or removal. Owing to inadequate literature and absence of established guidelines, treatment options remain challenging, and most of the infected cases are shifted to hemodialysis. However, we report the successful treatment of six patients with exit site fungal infection using a combination of oral fluconazole and topical miconazole for four weeks without requiring catheter removal. This approach is rarely documented and highlights a promising alternative to hemodialysis that warrants further research
Peritoneal dialysis (PD) catheter-related infections, including exit site infections (ESIs) and tunnel infections (TIs), are major risk factors for peritonitis. Infectious complications are the most common reasons of hospital admissions, technique failure, switching from peritoneal dialysis to hemodialysis, and even death. ESI rates range from 0.06-0.42 episodes per patient-year at risk [7]. The International Society for Peritoneal Dialysis (ISPD) recommends an ESI rate below 0.40 episodes per patient-year at risk, achievable through prophylactic antibiotics, lifestyle adjustments, and daily exit-site care. [8]. The most common organisms causing exit site infections include diphtheroid (20.5%), staphylococcus aureus (13.6%), pseudomonas aeruginosa (13.6%) and fungus (9.1%) [12]. The ISPD recommends PD catheter removal for ESIs or tunnel infections progressing to peritonitis or simultaneously occurring with peritonitis (with the same organism) or ESIs refractory to antibiotics [8]. Exit-site fungal infections represent a minority of cases, with candida parapsilosis as the predominant causative organism [13]. Risk factors include diabetes mellitus, immunosuppressive therapy, and recent antibiotic use [14].
There are no strong guidelines concerning the treatment options for fungal exit site infections and whether to remove the PD catheter. The lack of established guidelines presents a dilemma among clinicians. However, we report the successful treatment of six peritoneal dialysis patients with exit site fungal infection using a combination of oral fluconazole and daily topical miconazole cream for four weeks, preserving their catheters. To the best of our knowledge, this approach is rarely reported in the literature and offers a potential alternativeto the customary practice of catheter removal.
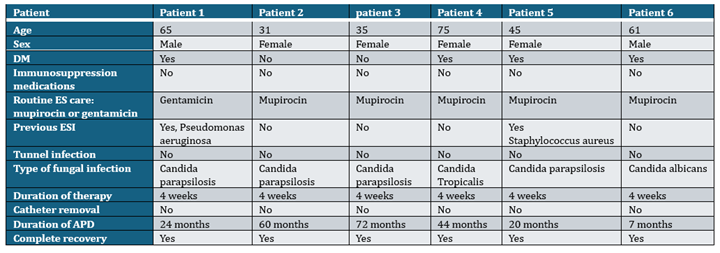
Table I: The Characteristics of the Six Patients with Exit Site Fungal Infection. DM: Diabetic Mellitus, ES: exit site, ESI: exit site infection, APD: Automated Peritoneal Dialysis
Case 1:
A 65-year-old Saudi gentleman is a known case of end-stage renal disease (ESRD) secondary to diabetic nephropathy, hypertension, and coronary artery disease status post coronary artery bypass graft (CABG) was started on incremental Automated Peritoneal Dialysis (APD) three times per week as he had good residual kidney function with routine exit site care with mupirocin. The patient developed ESI secondary to pseudomonas aeruginosa. Therefore, he was treated with topical gentamicin ointment daily and intraperitoneal Ceftazidime for three weeks with complete recovery of ESI. Six months later, he presented with erythema and brownish discharge from the exit site. Swab culture from the exit site revealed Candida Parapsilosis, while the tunnel ultrasound showed no fluid collection around the catheter or the cuff. He was treated with oral fluconazole 200 mg daily combined with miconazole cream daily for four weeks. After two weeks of treatment, the exit site culture became negative, and the subsequent monthly cultures for six months were also negative with no signs of infection.
Cases 2 to 6:
Cases (2, 3, and 5) represent female patients aged 31, 35, and 45 on APD who developed exit site fungal infections (ESFIs) with the same organism. They were treated with a similar regimen (oral fluconazole and topical miconazole cream) with complete recovery. The fourth patient was a 75-year-old male who developed ESRD secondary to diabetic nephropathy and had ESFI three years after starting APD. The exit site culture was consistent with Candida Tropicalis and was treated similarly to the previous cases. The last patient developed ESFI four months after commencing APD, and the exit-site infection culture revealed Candida Albicans. He was also treated with the same regimen (daily oral fluconazole 200 mg and topical miconazole cream). All our patients had tunnel ultrasound, which did not detect any signs of tunnel infection, and none of our patients had exit -site bacterial infections after the local application of miconazole cream.
Peritoneal dialysis (PD) is a vital treatment option for patients with end-stage kidney disease (ESKD) worldwide. PD constitutes about 10% of the dialysis population in the Kingdom of Saudi Arabia [1]. However, catheter-related infections, particularly exit-site infections (ESIs) and peritonitis present significant challenges that can lead to treatment failure and the necessity to switch to hemodialysis (HD) (2-3). Infections caused
by staphylococcus aureus and gram-negative organisms are usually difficult to eradicate and often need prolonged antibiotic therapy, frequent hospitalization, and catheter removal. Prophylactic antifungal medications in all patients with bacterial peritonitis significantly decreases the frequency of subsequent fungal infection [19]. ESI is usually defined as the presence of purulent discharge with or without skin erythema, while tunnel infection involves erythema, induration, or tenderness over the subcutaneous tract, which may be difficult to detect clinically and require ultrasound confirmation [5]. Exit-site infections caused by staphylococcus aureus or pseudomonas aeruginosa frequently coexist with tunnel infections (6).
As per the ISPD recommendations in 2017, each center needs to report exit site and tunnel infection regularly as part of continuous quality improvement. Further, the ISPD committee suggested reporting catheter-related infections as the number of episodes per patient per year. The overall incidence of ESI varies from 0.06 to 0.42 episodes per patient year [7]. The latest ISPD guideline in 2023 suggested that the ESI rate should not exceed 0.4 episodes per patient-years at risk, and PD catheter insertion-related catheter infection should be less than 5% within 30 days of catheter insertion [7-8]. At our center, the prevalence of exit site infection is 0.008% episode per year at risk, which is considered very low compared to other reported centers.
Bernardini et al. has shown that using gentamicin ointment increases the risk of developing exit site fungal infections (ESFI)by 20% in comparison to mupirocin cream, though the use of gentamicin ointment significantly reduces the ESI for both gram-positive and gram-negative bacteria [16]. Notably, only one patient in our series used gentamicin. Overall, the incidence of exit site fungal infections varies from 1%-6.5% [13-15]. Fungal exit site and tunnel infections in Automated Peritoneal Dialysis (APD) are rarely being reported in the literature. Data regarding treatment course, duration, and time of catheter removal and reinsertion is scarce. ESFI can progress to fungal peritonitis, leading to devastating complications such as frequent hospitalizations, catheter loss, technique failure and much more mortality in comparison to bacterial peritonitis [9-10,18]. Consequently, many clinicians opt for catheter removal as a preventive measure [11-12]
Candida parapsilosis is a common skin colonizer, particularly in subangular areas, and can thrive in glucose-containing solutions and adhere to synthetic foreign body materials [17]. However, it is highly susceptible to most antifungal agents [13]. According to the Infectious Diseases Society of America, the core treatment for mucocutaneous candidiasis rests fundamentally on antifungal therapy with topical or systemic azole [12,13]. Our results of treating ESFI align with a retrospective observational study by Sofia Coelho et al., who treated 30 ESFI episodes in 26 CAPD patients (caused by candida parapsilosis). The patients were treated with fluconazole or itraconazole for 64.4 (±33.9) days with a success rate of 80%, and only six episodes required catheter removal [13]. Similarly, four of our patients with ESFI had candida parapsilosis, and we successfully used only a four-week regimen combining topical and systemic azoles.
Multiple Candida species, including albicans, glabrata, krusei, parapsilosis, and tropicalis, can cause infections [14]. Common risk factors for fungal infections include diabetes mellitus, prolonged antibiotic use or previous use of antibiotics, recurrent peritonitis, malnutrition, and immunocompromised patients [14]. While clear guidelines for exit-site care and antibiotic use in PD are lacking, our center and many others employ daily mupirocin cream or gentamicin ointment for gram-negative ESIs. However, prolonged antibiotic use might contribute to fungal ESIs at our center. We believe that the high success rate in our case series is primarily due to a reduced frequency of antibiotics and the intensified use of local antifungal with miconazole cream combined with oral fluconazole for at least four weeks.
In conclusion, while most ESFI cases had shown favorable clinical response with medical treatment, catheter removal or exchange remains an option for those unresponsive to extended antifungal therapy. Further research is required to establish optimal treatment protocols, including duration, and to guide decisions regarding catheter removal and reinsertion.
This is a retrospective, observational study with limited number of patients and absence of comparable control group.
The authors would like to express their sincere gratitude and appreciation to the dedicated team of peritoneal dialysis nurses at King Fahad University Hospital in Al Khobar. Their unwavering support and meticulous patient follow-up were instrumental in achieving these excellent outcomes.
Dr. Moaz Abdulgalil, Prof. Ibrahiem Saeed Abdul-Rahman, and Dr. were responsible for collecting the cases and drafting the case presentation. Prof. Alhwiesh and Dr. Khadija Alshehabi performed the literature review and drafted the discussion. Prof. Alhwiesh, Dr. Mohammed Nasr El-Din, Dr. Amani A. Al-Hwiesh, Dr. Nadia Al-Audah, Dr. Hatem H Althubaini, Dr. Khadija Alshehabi, and Dr. Marium AlDossari contributed to writing and reviewing the manuscript.
The authors declare no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Ethical approval was obtained from Imam Abdulrahman bin Faisal University Review Board of Medical Center. All participating patients provided written consent.
The authors received no financial support for the research, authorship, and/or publication of this article.