AUCTORES
Globalize your Research
Re-print Article | DOI: https://doi.org/10.31579/2694-0248/058
Orthopedics Department, Spanish Hospital. Av. Mexican National Army 613, Granada, Miguel Hidalgo, 11520 Mexico City, CDMX, Mexico.
*Corresponding Author: Gómez Mont Landerreche Juan Gabino, Orthopedics Department, Spanish Hospital. Av. Mexican National Army 613, Granada, Miguel Hidalgo, 11520 Mexico City, CDMX, Mexico.
Citation: Rodriguez M V, Gómez Mont L J Gabino, Castañeda G Jossue, Jarquin G F de Jesus, and Palafox C. Ignacio, (2023), Re-print: Restoring Horizontal Stability in III-V Acromioclavicular Dislocations by Anatomic Reconstruction of the Coracoclavicular and Acromioclavicular Ligaments; Surgical Technique, J. Clinical Orthopedics and Trauma Care, 5(2); DOI:10.31579/2694-0248/058
Copyright: © 2023, Gómez Mont Landerreche Juan Gabino. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 11 April 2023 | Accepted: 25 April 2023 | Published: 15 May 2023
Keywords: acromioclavicular; dislocations; anatomic technique; horizontal stability; coracoclavicular and acromioclavicular ligaments; vicryl 2.0
Dislocation of the acromioclavicular (AC) joint is a common injury seen in young adults. The objective is to describe a surgical technique that can restore the horizontal and vertical stability of the AC joint. This is a surgical technique with anatomical and biological reconstruction of the CC and AC ligaments, using an allograft. Two bone tunnels are made in the clavicle, passing the lateral end of the graft below the acromion; then the two ends are fixed with 2 bio-absorbable screws, restoring vertical and horizontal stability. This procedure allows to restore the vertical and horizontal stability of the AC joint. Follow up studies are required to report functional and radiological results, in order to ensure advantages compared to existing techniques.
Injuries to the acromioclavicular (AC) joint are common in male athletes following acute shoulder trauma [1]. They are mostly mild sprains and occur more frequently in men than in women (5:1), with a higher incidence in the 20-30 age group. They represent ~12%, and can reach 21% in some cases of all shoulder injuries [1-3].
The AC joint is a flat diarthroid joint that serves as the main connection between the axial skeleton and the upper extremity [3]. Its complex ligamentous structure is essential for the normal function of the shoulder girdle. It is made up of dynamic and static stabilizers, providing anterior, posterior, superior and inferior stability. The Acromioclavicular (AC) and Coracoclavicular (CC) ligaments are the static stabilizers, while the deltoid and trapezius muscles are the dynamic stabilizers [3]. The AC joint is normally capable of displacement of 4 to 6 mm in the anterior, posterior and superior planes under loads of 70N. It also allows rotational movement of 5° to 8° during scapulothoracic movement and 40° to 45° of shoulder abduction and elevation [4, 12].
The treatment of an AC dislocation depends on its degree of injury according to the Rockwood classification and the functional demand of the patient [5]. The most common mechanisms of AC joint injury include a fall onto an outstretched arm or a direct axial-loading contusion to the lateral aspect of the shoulder with the arm adducted [6]. Patients report upper shoulder pain during upper extremity elevation attempts; with tenderness in the AC joint [7].
The Rockwood classification system is used as a guide for treatment [3]. Type I is an AC ligamentsprain; the AC and CC ligaments are intact. Type II is a partial tear of the AC ligament, but not the CC ligament; with lessthan 25 percentage clavicle displacement. Type III is a rupture of the AC and CC ligaments, with 25% to 100% displacement of the clavicle compared to the contralateral side [5].
Type IV the AC and CC ligaments are torn and present a posterior displacement of the distal clavicle Type V the AC and CC ligaments have >100% displacement of the clavicle. Type VI is the result of inferior displacement of the distal clavicle to the subcoracoid position [7,8].
There are many treatment options depending on the patterns of low or high energy trauma. Type I and type II injuries are the result of low energy forces which are treated conservatively with shoulder immobilization [9]. Type IV, V and VI injuries are the result of high energy forces and are usually treated with surgery [3]. Type III injuries are a subject of debate, depending on the functional demand of the patient and decision of the surgeon [8,9]. Each case must be treated individually, remembering that 50% of patients with grade II to V injuries have some glenohumeral intra-articular injury [10].
The AC fixation allows recovery of the CC ligaments by restoring distance between the clavicle and coracoid [11]. Different open surgical techniques are currently performed, but they are associated with complications such as infection, fixation failure or implant failure. There are arthroscopic techniques that reduce complications and allow the identification of associated pathologies in the glenohumeral joint [7,12, 13]. Proper management requires reconstruction of the AC ligament as well as the superior joint capsule. Currently the development of techniques for the management of these injuries continues [14].
The objective of our surgical technique is to restore both vertical and horizontal stability of the acromioclavicular (AC) joint.
Surgical Technique
All surgeries were performed by the same surgeon, in a period less than 3 days after the patient's injury after the diagnosis(FIG 1).
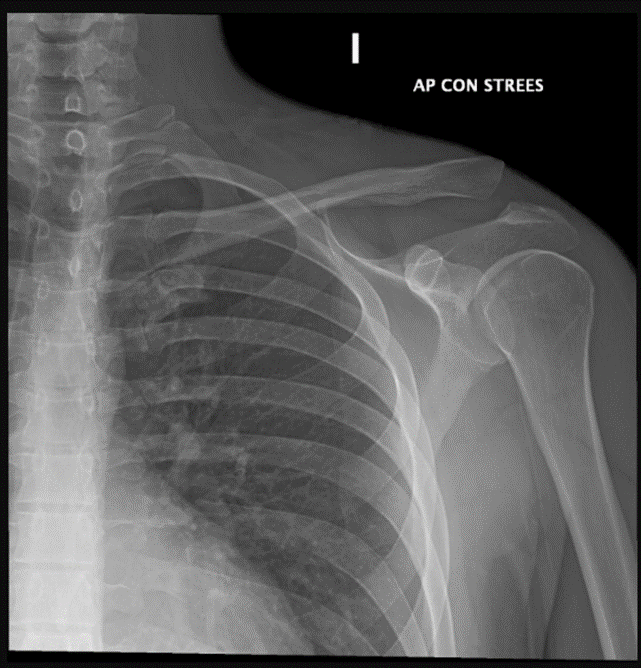
Figure 1: Anteroposterior X-ray of the left shoulder with stress. Observed the loss of acromioclavicular joint congruence, with caudal elevation of the distal third of the clavicle
With the patient under general anesthesia and prior antibiotic prophylaxis, the patient is placed in a beach chair position at 60° flexion. First the anatomical landmarks are identified using surface anatomy; the coracoid process, acromion, and the AC joint are marked (FIG 2).

Figure 2: Patient in beach chair position. Upper view of a right shoulder. Marking anatomical structures is observed for the approach that begins 3.5 cm medial to the acromioclavicular joint, with extension to the coracoid.
The anterior border of the clavicle is incised 5 cm lateral to the AC joint and extended toward the coracoid process following Langer´s lines. It is dissected by planes, performing hemostasis with electrocautery until the deltoid muscle is identified in the anterior part of the clavicle and the insertion of the trapezius in its posterior surface. A blunt dissection is performed on the deltoid fascicle towards the coracoid process until the base of the coracoid process is located and sterile gauze is passed as a reference. Complete exposure of the clavicle and AC joint is performed; as well as its soft tissues that prevent joint reduction (FIG 3). Then resect 3 mm of the distal edge of the clavicle and soft tissues (remaining AC ligaments and articular disc) are excised (FIG 4) [17].

Figure 3: Exposure of the clavicle and acromioclavicular joint is observed. Observed the gauze that is a reference of the base of the coracoid

Figure 4: Upper view of a right shoulder. It is noted resection of the distal edge of the clavicle and soft tissues that prevent reduction of the AC joint.
The CC ligament debris (trapezoid and conoid) are identified, guides are placed to make 2 bone tunnels (posteromedial and anterolateral) usually 5.0 mm (depending on allograft diameter), in the clavicle according to the native anatomical locations of the CC ligaments. A minimum distance of 20 to 25 mm between the tunnels was maintained where possible, with the trapezoidal tunnel placed at least 15 mm medial from the distal end of the clavicle (FIGURE 5) [17].

Figure 5: Superior view of the clavicle in the right shoulder. Bone tunnel perforations are observed in the anatomical site of the coracoclavicular ligaments
Through a lateral incision 2cm distal the lateral border of the acromion a nitinol guidewire is passed under the acromion. Manual traction of the AC joint is performed, while an assistant performs graft fixation in the clavicular orifices with two 5 mm x 15 mm bio-tenodesis screws, observing adequate graft fixation and establishing vertical stability (FIG 7). Subsequently the debris of the distal end of the graft is passed under the acromion, with the help of a nitinol guide in the lateral incision, and is sutured with its proximal end on the upper edge of the clavicle with a non-absorbable suture (FIGURE 8, 9) [17].

Figure 7: Superior view of the clavicle in the right shoulder. Reduction if the AC joint and graft fixation with 2 bio-absorbable screws are observed. The distal end of the graft passes under the acromion and the graft is fixed with non-absorbable suture in the lateral hole.
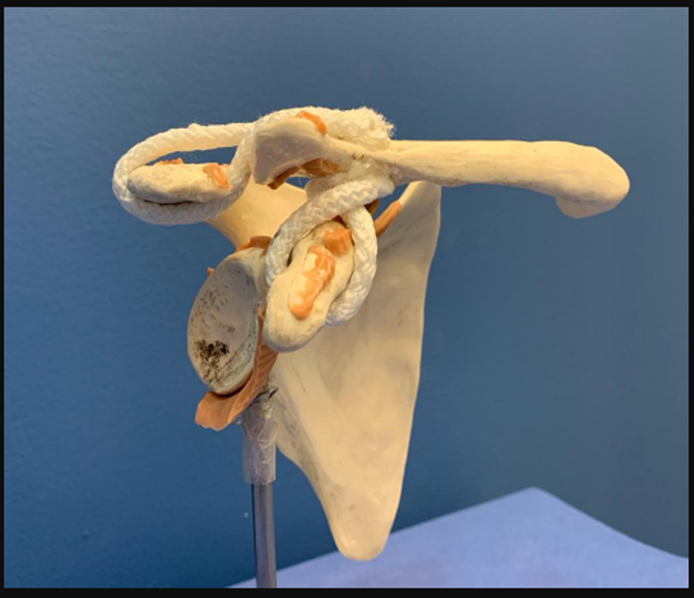
Figure 8: Representation of the anatomical reconstruction of the AC joint with autologous graft in its Anteroposterior projection.
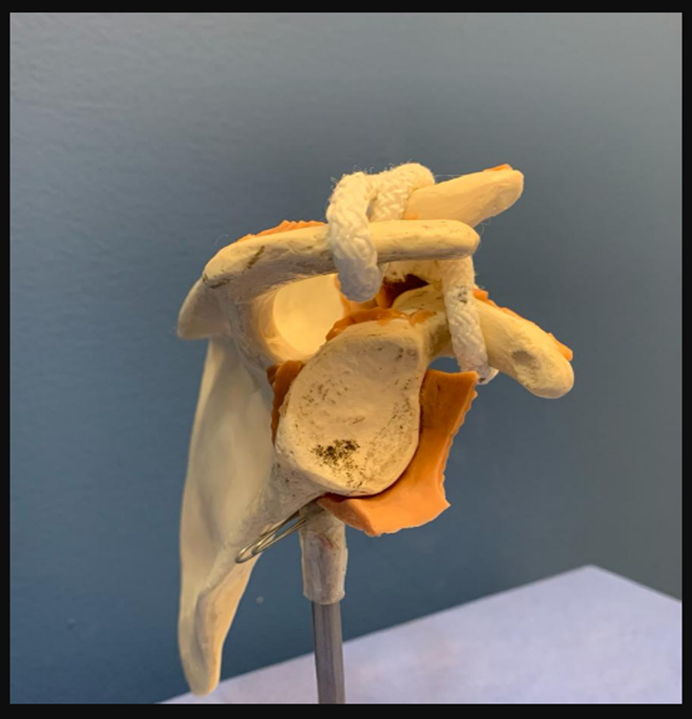
Figure 9: Representation of the anatomical reconstruction of the AC joint with autologous graft in its axial projection.
The graft in addition to serving for the reconstruction of the CC ligaments; its interposition in the AC space Works as a spacer, replacing the function of the articular disc of said joint. With the fluoroscope an anteroposterior view is taken, confirming adequate reduction of the AC joint (FIG 10) [17].
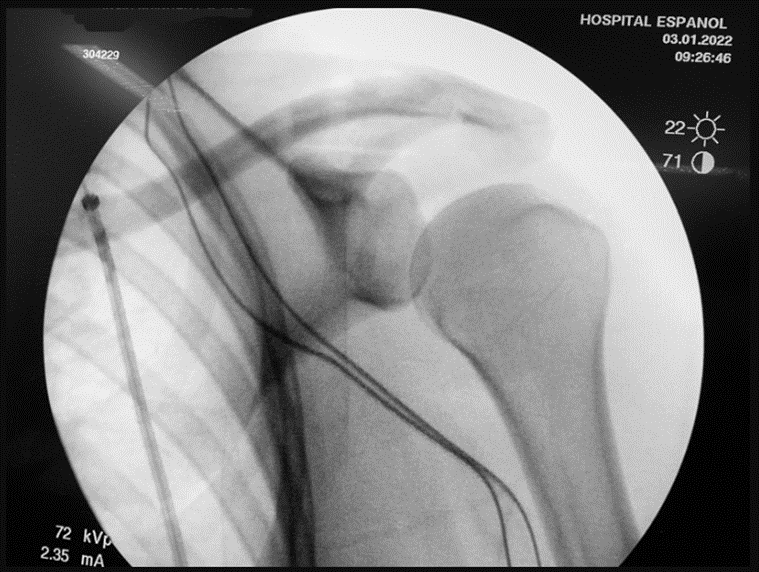
Figure 10: Anteroposterior shoulder fluoroscope control showing reduction of AC joint.
The surgical wound is irrigated with saline solution. Deltotrapezial fascia is carefully closed with interrupted stitches with absorbable sutures (Vicryl 2.0) and subsequently by planes: subcutaneous cellular tissue with Vicryl2.0 suture with inverted “U” stitches and skin with a barbed absorbable suture 3-0 with subdermal continuous stitch. The thoracic limb is immobilized with a shoulder immobilizer and an adductor band [17].
The AC joint injuries represent a diagnostic and therapeutic challenge that require accurate clinical evaluation with a detailed physical examination to assess scapular motion [1]. We described a surgical technique that managed to restore both vertical and horizontal stability, with an anatomical reconstruction of the AC and CC joint.
Neurovascular structures need to be assessed. The indication for surgery is clear in type IV, V and VI injuries [5, 6]. The treatment of acute type III dislocation depends mainly on the functional demand and expectations of the patient; however recent studies have shown better functional results with surgical treatment [7, 15].
Surgical treatment should focus on reduction and fixation of the AC joint, repair of the deltoid- trapezius fascia, and repair or reconstruction of the CC ligaments [3].
There is still no optimal surgical technique described for the treatment of these injuries; clinical and anatomical studies are in favor of anatomical reconstructions. The original technique of Weaver-Dunn (1972) in recent biomechanical studies has shown that anatomic reconstruction with free grafts provides better stability compared to the other ligament transfer procedures [6, 9, 14].
Primary reconstruction using tension bands and Kirschner wires applied through the AC joint or extra-articular Bosworth screws to hold the clavicle in a reduced position; they are simple techniques that are based on the primary repair of the CC ligaments [3, 5]. However, all are rigid fixation methods that can lead to implant failure and are considered biomechanically insufficient [4,14]. The hook plate fixation presents some complications, like osteolysis, acromial fracture, osteoarthritis of the AC joint, subacromial impingement and rotator cuff tears; as well as the need for a second surgery to remove the implant that can also fracture the distal clavicle [2, 4].
The arthroscopic techniques obtain better functional results, better aesthetics and allow an earlier return to activities of daily living [5]. They focus on ligament healing or ligament reconstruction [4, 5]. In our technique, the AC repair is complemented with previous shoulder arthroscopy to identify associated pathologies in the shoulder joint. In case of existing pathology, they were repaired in the same surgical time.
The repair procedure can be performed using an arthroscopy-assisted mini open technique or a fully arthroscopic technique. Among these techniques is the Tight Rope, which is a double metal button with four high strength sutures threads [9]. The results are satisfactory with good functional results, especially in type III and type IV acute injuries; although it can be considered not as profitable as open methods [5,16].
The arthroscopy-assisted restoration of the CC ligament with the use of a double-bundle free tendon graft (autograft or allograft) and a suture-lace device is called the coracoid cerclage technique. In this procedure a conoid and a trapezoid tunnel are drilled into the clavicle, the tendon graft is placed in an eight-cross pattern. Loss of reduction is common with this approach, as the native components (trapezoid and conoid) of the original CC ligaments are not restored [14].
The importance of restoring joint structure in both the horizontal and vertical planes is an important parameter to recover the native anatomy of the AC joint. 4 The advantage of our surgical technique is that it restores the anatomy of the CC ligaments and restores the horizontal stability of the AC joint with the application of an allograft and tenodesis fixation with two screws. The use of allograft to replicate native CC ligaments was shown to provide better vertical and horizontal stability compared to other non-anatomic techniques [2].
Another advantage is that our technique uses the allograft for the reconstruction of the CC ligaments, it can provide better biomechanical stability and a possible permanent biological reconstruction, with a failure rate equivalent to that of native CC ligaments [1-3]. The graft in addition to serving for the reconstruction of the CC ligaments; its interposition in the AC space Works as a spacer, replacing the function of the articular disc of said joint.
The previously described surgical technique is one more surgical treatment option for the management of acromioclavicular dislocations. It allows to recover adequate stability and restore the anatomical properties of the acromioclavicular joint, recovering both vertical and horizontal stability. It is a reproducible technique that requires a larger number of patients and follow-up studies to assess functional results compared to other therapeutic options.