AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2690-4861/840
Catholic University of Córdoba. Faculty of Health Sciences, Argentina.
*Corresponding Author: Barbara Nigro, Catholic University of Córdoba. Faculty of Health Sciences, Argentina.
Citation: Barbara Nigro, Mario Bendersky, (2025), Prevalence of Hypertension and Frequency of Patients Monitored in A Hospital Sample, International Journal of Clinical Case Reports and Reviews, 27(5); DOI:10.31579/2690-4861/840
Copyright: © 2025, Barbara Nigro. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 16 May 2025 | Accepted: 26 May 2025 | Published: 11 July 2025
Keywords: high blood pressure; cardiovascular disease; cva; infarction; sequelae; pandemic.
Hypertension remains a major public health challenge worldwide because it increases the risk of cardiovascular disease. Effective blood pressure management has been shown to reduce the incidence of stroke, heart attack and heart failure.
The current prevalence of HTA in our country is 36.3%.
In the Renata 2 study, four out of ten HTA patients are unaware of their condition.
This observation is not unrelated to what is happening globally.
In the Pure study, only 13% of hypertensive patients were controlled. 30% had optimal blood pressure and the other 30% were in prehypertension Of the 40% of patients with hypertension, 40% received treatment, but only 13% had their disease controlled.
This research work, carried out in the Cardiology Service of the National Hospital of Clinics in the city of Córdoba, aims to evaluate the prevalence of HTA and frequency of controlled patients who attend outpatient clinics. of Cardiology between the month of April 2021-February 2022.
The data will be obtained from a random sample through the use of medical records between the month of April 2021-February 2022. One year of Pandemic.
The hypothesis is to verify the insufficient control of arterial hypertension beyond what was found in the results of the aforementioned studies, in our population of the City of Córdoba, and in a totally different year, a year of Pandemic. Where access to health is limited by COVID 19.
Non-communicable diseases (NCDs) disproportionately affect people living in low- and lower-middle-income countries [1,2,3]. with almost three-quarters of all NCD deaths and 82% of premature deaths occurring within low- and middle-income countries [4].
Hypertension remains a major public health challenge in the United States because it increases the risk of cardiovascular disease. Effective blood pressure management has been shown to reduce the incidence of stroke, heart attack, and heart failure [5,6,7].
The prevalence of hypertension increased with age, from 7.5% among adults aged 18–39 years to 33.2% among those aged 40–59 years and 63.1% among those aged 60 years and older. A similar pattern was found among men and women. Men had a higher prevalence of hypertension than women among adults aged 18–39 years (9.2% vs 5.6%, respectively) and 40–59 years (37.2% vs 29.4%, respectively), but men had a lower prevalence of hypertension than women among adults aged 60 years and older (58.5% vs 66.8%, respectively) [8].
In the INTERHEART study, hypertension was found to be an independent risk factor for acute myocardial infarction among older people [9].
The estimated global prevalence of hypertension was 1.13 billion in 2015, with over 150 million in Central and Eastern Europe. The overall prevalence of hypertension in adults is around 30–45%, with an age-standardized prevalence.
globally of 24 and 20% in men and women, respectively, in 2015 [10,11].
This high prevalence of hypertension is consistent worldwide, regardless of income level—that is, in low-, middle-, and high-income countries. Hypertension becomes progressively more common with age, with a prevalence of more than 60% in people over 60 years of age.
As populations age, adopt more sedentary lifestyles, and increase their body weight, the prevalence of hypertension worldwide will continue to rise. The number of people with hypertension is estimated to increase by 15% to 20% by 2025, reaching nearly 1.5 billion.
Recent meta-analyses show significant reductions in cardiovascular events and mortality due to treatment in patients with grade 1 hypertension ]13,14,15].
These findings have been supported by the results of a subgroup analysis of the Heart Outcomes trial Prevention Evaluation (HOPE 3), showing a significant 27% reduction in major cardiovascular outcomes in patients with intermediate cardiovascular risk and baseline SBP values in grade 1 hypertensive patients [16].
Hypertension is the risk factor that most contributes to cardiovascular disease, the leading cause of death throughout Latin America [17,18].
It is estimated that up to 40% of the adult population is affected by hypertension, similar to that of developed countries. For example, the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) showed that the adjusted prevalence of hypertension was higher among Blacks (49.2%) compared to Whites (30.3%) and Mixed-race (38.2%) individuals [19].
Data from Mexico City showed a sharp increase in the prevalence of treated hypertension from middle age (26% between 35-44 years) to the elderly (59% between 75-84 years), with this increase being significantly greater in women than in men [20].
Furthermore, in a cross-sectional survey of approximately 7,500 adults from four cities in Argentina, Chile, and Uruguay, approximately 42.5% had hypertension and 32.5% had prehypertension. Of this population, approximately 63.0% were aware of their condition, 48.7% were taking prescription medications to lower blood pressure (BP), but only 21.1% of all hypertensive patients and 43.3% of treated hypertensive patients had their BP controlled 21,22,23.
The current prevalence of hypertension in our country is 36.3% [24].
This figure is in line with the latest WHO reports for the Americas. The increase in the prevalence of hypertension worldwide is attributed to population growth and aging, as well as factors such as unhealthy diet, excessive alcohol consumption, sedentary lifestyle, excess weight, and persistent exposure to stress [25].
In the RENATA-2 study, four out of 10 hypertensive patients were unaware of their condition. This observation is not unrelated to what is happening globally.
PURE (Prospective Urban Rural Epidemiology) study, which examined the prevalence, awareness, and control of hypertension in 142,042 individuals from rural and urban communities in various low-, middle-, and high-income countries; they concluded that, in the population, 46.5% of participants with hypertension were aware of their diagnosis, and 32.5% of those with blood pressure control were being treated; this suggests a substantial improvement in the diagnosis and treatment of hypertension [27] .
In this study, at a general level it was reported that among participants with hypertension, 46.5% were aware of their condition, 40.6% were receiving treatment, and 13.2% had their blood pressure controlled; when the South American region was analyzed, the degree of ignorance (42.9%) reached a proportion close to the results of the RENATA-2 study; that if 43.6% of treated hypertensive patients were controlled, when the total number of hypertensive individuals (known and unknown) was considered, only 1 in 4 was controlled with pharmacological treatment [26] .
The PURE study concluded that 18.8% of hypertensive individuals analyzed in our region were under control, as in the RENATA-2 study. Furthermore, knowledge and level of BP control were lower in men and younger individuals. [26,27]
This situation shows the importance of the commitment that physicians should assume in their daily practice, and the activity of scientific societies in training health professionals, and state agencies in communicating to the community and teaching from the beginning of schooling the risks of suffering from hypertension. Ostchega et al , in their report, infer that around 30% of hypertensive patients who are treated with monotherapy manage to achieve the BP goal, indicating that most patients will require two or more drugs [28 ].
The proportion of hypertensive patients in the national study receiving monotherapy, greater than 70%, may explain the low rate of BP control. Furthermore, our researchers observed that a fixed-dose combination regimen better controlled BP; this finding is supported by Gupta et al., since fixed-dose combinations of two or more antihypertensive active ingredients in a single tablet reduce the number of doses, promote treatment adherence, and optimize BP control .
Considering that approximately 50% of patients adhere to treatment for hypertension one year after starting it, it is understandable that poor therapeutic adherence is postulated as one of the reasons for the low control rates in society. p30, 31, 32]
In RENATA-2, where half of the treated hypertensive patients reported compliance with the antihypertensive procedure, it was demonstrated that adherence is linked to a higher rate of BP control. [26]
Using educational attainment as a surrogate marker of socioeconomic status, the PURE analysis found that, in low-income countries, BP judgment, performance, and control were lower among participants with primary or no education. These results are similar to social patterns of hypertension prevalence monitored in certain low-income regions. [27]
To determine the prevalence of hypertension and the frequency of hypertensive patients who are unaware of their disease in a sample of consecutive patients in the Cardiology Service of the National Hospital of Clinics of Córdoba during the years 2020-2021.
To determine the prevalence of hypertension and the frequency with which hypertensive patients are unaware of their disease.
To determine the prevalence of untreated or undertreated HT.
Relate the prevalence of hypertension with risk factors and cardiovascular events.
Descriptive, observational, cross-sectional study of data from medical records (secondary data source). Population/sample: Clinical data of consecutive normotensive and hypertensive patients who attended spontaneously or were referred to the Cardiology Department of the Hospital Nacional de Clínicas, between April 1, 2021, and February 28, 2022. Since these are consecutive cases and within a specific time period, the population will comprise the study sample.
Variables
1.Hereditary history of hypertension (yes/no).
2. Body mass index (BMI), calculated using the weight/height ratio 2, with individuals with a BMI >30 being considered obese.
3. Level of physical activity, including the following: a) sedentary: work with little physical activity; b) active: performs activities that require moderate physical activity; c) athletic: practices sports regularly but not professionally; d) intense athlete: practices sports professionally; e) extreme exertion: performs regular physical activity that requires significant physical effort.
4. Salt ( NaCl ) consumption: a) normal: added only when preparing food; b) abundant: added during food preparation and then over-added when consumed.
5. Types of diet: according to the quantity and quality of food, meats, fats, vegetables, dairy products, sweets, sausages: a) normal; b) deficient; c) abundant.
6. Alcohol consumption: a) does not consume; b) consumes occasionally; c) moderate consumer: during and outside of meals, up to 1 liter of wine per day; or 4 or more drinks for women and 5 or more drinks for men on one occasion. d) heavy consumer: during and outside of meals, more than 1 liter of wine per day, or 8 or more drinks for women and 15 drinks for men per week.
7. Smoking: a) does not smoke; b) smokes; c) quit smoking.
8. Economic situation: a) poor: does not cover basic needs; b) modest: covers basic needs with limitations; c) average: covers all basic needs and some comfort; d) comfortable: without major restrictions.
9. Blood pressure values: considered optimal or ideal: <120/80 mmHg ; normal: <139/89 mmHg ; high blood pressure: >140/90 mmHg .
10. Diabetes Mellitus: Defined as fasting blood glucose >126 mg/dL on two occasions separated by one week. Abnormal oral glucose tolerance test (OGTT). 200 mg/dL at 2 hours . Glycosylated hemoglobin>6.5%.
11. Dyslipidemia: Total cholesterol >200 mg/dl, Ldl >100 mg/dl, HDL <35 mg/dl in men and <40 mg/dl in women, triglycerides >150 mg/dl.
Independent Variable: High blood pressure.
Dependent Variables: risk factors, laboratory and anthropometric data.
Data sheets were collected throughout the study period and then analyzed by pairing them. An Excel®-type database was created with the collected data, which was subsequently used for statistical processing. Measures of centrality and dispersion (mean and standard deviation) were calculated for quantitative variables, and absolute and percentage distributions were calculated for categorical variables. Kruskal-Wallis or Student 's t tests were applied to compare means (after applying the Shapiro -Wilks normality test) and the chi-square test was used to correlate categorical variables. In all cases, a p-value <0.05 was considered statistically significant. InfoStat®p (v. 2016) statistical software was used for statistical processing. The results are presented in graphs or tables, depending on their best interpretation.
Ethical considerations
The work plan has been approved by the Head of Service and the Training and Teaching Committee of the National Hospital of Clínicas, FCM, UNC. The data were collected anonymously for inclusion in a computer database, protected by statistical confidentiality.
Results
Data from 849 consecutive individuals who met the inclusion criteria and who presented spontaneously or were referred to the Cardiology Department of the National Hospital of Clinics in Córdoba during the analysis period for clinical cardiology follow-up were analyzed. 63% of these patients were diagnosed with hypertension (n=535) (Figure 1).
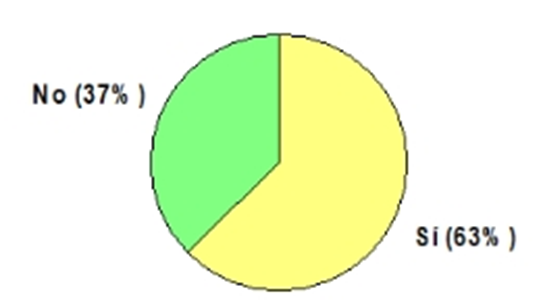
Figure 1: Distribution of the analyzed sample by hypertension diagnosis. Values are represented as percentages of cases. (n=849)
The characteristics of the cases analyzed are observed in (table 1).
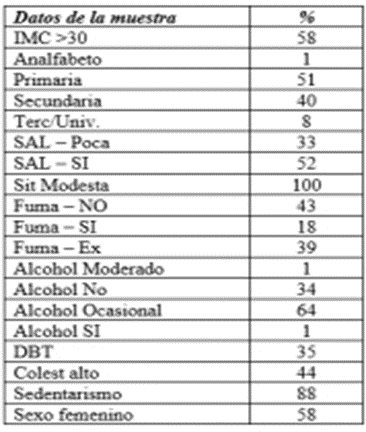
Table 1: Characteristics of the sample analyzed (n=889)
Of the total number of cases, it was determined that 133 individuals were unaware of their condition; and 172 were presumed to be hypertensive but were not (Table 2); making a total of 255 (65%) individuals unaware of their condition. It was also observed that among those aware of the condition, 30% were not hypertensive.
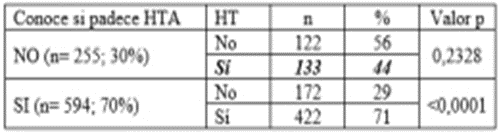
Table 2: Distribution of cases according to whether they knew whether or not they suffered from high blood pressure (n=849)
References: n: number of cases; %: percentage of cases; HT: hypertensive; NT: normotensive.
The number of HT patients who did not receive adequate or insufficient treatment was then analyzed, and it was quantified that 40.8% did not have their BP properly controlled, this value being statistically significant (Table 3).
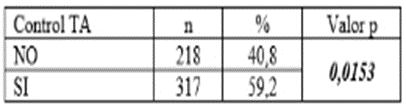
Table 3: Distribution of hypertensive patients according to whether they received treatment to control high blood pressure (n=535)
References: n: number of cases; %: percentage of cases; BP: blood pressure.
When analyzing the characteristics of the HT cases, it was determined that 58% had a body mass index> 30, 57% were smokers or ex-smokers, 64% occasional drinkers, 44% hypercholesterolemic, 35% diabetic and 88% sedentary and that 58% were female (without statistically significant differences with respect to males, 66.9 ± 13.45 vs 65.1 ± 13.62, p> 0.999 -Kruskal Wallis test-). In relation to knowing their condition and educational level achieved, in primary and secondary levels it was observed that the percentage of individuals who recognized their HTA was highly significant (78.9% and 63.9% respectively).
Salt intake was high, both for those who had their BP controlled and those who did not (54.75% and 62.14% respectively, p <0.0001).
Blood pressure (BP) is a biological characteristic that is continuously distributed in the population, and without a defined threshold beyond which the associated cardiovascular risk increases; therefore, the definition of arterial hypertension (AHT) —or systolic BP/diastolic BP
(SBP/DBP) •>140/90 mmHg - is pragmatic and conventional, guided by the objective that the expected benefit of the intervention outweighs the risk of not acting, for which there is considerable, although provisional, evidence [33].
Furthermore, BP is highly variable, as it depends on many physical and environmental characteristics in daily life; therefore, true BP is the average of many measurements. [34]
Environmentally, it is estimated that 50% of all new cases of high blood pressure in the population are attributable to excess weight; 30% to excessive salt intake (>4.5 g/day), and 16% to low physical activity [35].
However, in most cases, hypertension results from a complex interaction of multiple genetic and environmental factors.
High blood pressure is very common and the leading cause of premature death and disability worldwide, although there are significant disparities between countries at different levels of development [36].
Despite the progress made in the degree of control of hypertension in the population in the last decade, this remains relatively low [38].
High blood pressure is a very common medical condition, and its prevalence increases with age. It affects approximately 65% of individuals over 60 years of age and more than 70% of those over 85 years of age, as reported by Wiber et al. in the 1970s.
This occurs despite abundant evidence that increased control would lead to considerable individual and population benefit [33].
The decline in mortality and the increase in life expectancy are leading to a progressive aging of the population. While at the beginning of the 20th century life expectancy was 33.8 years for men and 35.7 years for women, it is currently around 74.3 and 81.5 years, respectively. According to WHO figures, 1.3% of the world's population is over 80 years old, and by 2050, it is projected that 4.4% of the world's population will be over 80 years old. This represents a scenario of great social and health impact, since the main medical consultations, both in hospitals and primary care, are carried out on the elderly population.
The prevalence of high blood pressure and the frequency of hypertensive patients who are unaware of their condition continue to be very high among patients who attended routine check-ups in the cardiology office at the National Hospital of Clinics during an extraordinary period such as the 2020-2021 COVID pandemic.
The results obtained show that 63% of patients were hypertensive, of these, 15% were unaware of their condition and 20.25% believed they were hypertensive but were not.
Regarding hypertensive individuals who had been diagnosed and treated for hypertension, 40.8% did not meet the therapeutic goal for controlling their blood pressure.
When analyzing comorbidities, it was found that 58% of individuals had a BMI>30, 57% were current or former smokers, 64% were occasional alcohol drinkers, and 58% of the study population was female.
It is notable in the population group studied that their blood pressure figures, that their educational level developed, both primary and secondary level, was highly significant in the percentage of individuals who recognized their hypertension.
Salt consumption was high, both for individuals who had their blood pressure controlled and those who did not (54.75% vs. 62.14%).