AUCTORES
Globalize your Research
case Report | DOI: https://doi.org/10.31579/2690-4861/617
1 Department of orthopedic Surgery, Beijing united family hospital, Beijing China.
2 Departments of Orthopaedics and Pathology, Beijing United Family Hospital, No 2 Jiangtai Road, Chaoyang District, Beijing, 10016, China.
*Corresponding Author: Jike Lu, Department of orthopedic Surgery, Beijing united family hospital, Beijing China.
Citation: Niu Jing, Qiao Xu Bai and Jike Lu, (2024), Post Traumatic Synovial Chondromatosis of the Elbow Joint - A Case Report, International Journal of Clinical Case Reports and Reviews, 20(4); DOI:10.31579/2690-4861/617
Copyright: © 2024, Jike Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 17 November 2024 | Accepted: 27 November 2024 | Published: 09 December 2024
Keywords: synovial chondromatosis; mechanical symptoms; elbow; arthroscopy; synovectomy
Synovial chondromatosis is most commonly occurs in knee joints, and rarely occur in elbow joint. Patient usually complaints of pain, swelling and restrictions of movements at the affected joint. Diagnosis is made through thorough clinical examination and imaging studies. We reported a 44-year-old female with complaints of pain and reduced range of movement (ROM), and catching locking symptoms in right elbow that was worsening on movements. She had a history of trauma in elbow joint two years ago. The patient was diagnosed with synovial chondromatosis after radiological investigations and confirmed with histology study. Arthroscopically assisted synovectomy, removal of the synovial chondral bodies was performed and post operatively timely physiotherapy was initiated at the involved elbow. After 6, 12 months of follow-up, the patient improved clinically and functionally.
There are two forms of synovial chondromatosis which is primary and a benign condition, and characterized with multiple intra-articular bodies with chondroid metaplasia in the synovium. Joint effusion, crepitus and restriction of range of motion of the joint can be seen. The secondary synovial chondromatosis is usually associated with trauma, degenerative joint disease, inflammatory arthropathies and neurological diseases, which are the cause of chondral loose bodies and joint abnormalities [1-2]. Usually it occurs in the large joints of the body such as hip and knee. The elbow is a very rare site for the disease and this location was firstly reported by Henderson M.S. in 1918 [3]. Clinical symptoms include pain, swelling and decrease in the range of motion, locking, articular crepitus and instability [2,4]. Sudden onset of severe loss of elbow extension and flexion range of motion can occur as caused by mechanical block from deposition of chondral fragments in the olecranon and coronoid fossae, respectively and this is always associated with severe pain [9].
A 44year-old woman presented with limitation of right elbow motion and progressively worsening with pain associated elbow movements. The pain was present when the patient was at rest, and aggravated when the elbow in motions. She did not describe any swelling but with catching, locking symptoms. The pain was started six-years ago after fell over accidently on an outstretched hand. After the accident she visited at emergency department and radiological imaging did not revealed any abnormalities in her elbow. For pain and swelling, elevation and cold-pad applied and then she was discharged home with pain medications. Her pain was relieved a few weeks post injury, however two years ago she was presenting in outpatient clinic, complained right elbow pain associated with weight lifting and pushing up from chairs. Initially her pain was managed as lateral epicondylitis but not effective. On clinical examination, varus stress, elbow Pivert shift tests were positive indicating lateral ulnar collateral ligament (LUCL) laxity (probably from old injury). Radiographs showed a few bony ossicles over lateral epicondyle and lateral radio-capitalum joint, however no bony abnormalities in anterior and posterior elbow joint space (Fig 1). CT scans showed that calcified fragments over lateral elbow joint and a tiny calcification lesion at the olecranon fossa (Figure 2 and 3).
After a few weeks’ physiotherapy, physical therapies her pain was not relieving, subsequently surgery was performed for debridement of the bony fragments and repairs of the LUCL. After surgery, her pain was completely relieved, elbow was stable and radiographs showed all extra articular ossification ossicles were removed except a tiny bony ossicle inside lateral collateral ligament (Figure 4).

Figure 1. Six years ago, the patient had right elbow injuries, but presented in clinic complained with lateral elbow pain which was managed as lateral epicondylitis. After a few weeks’ physiotherapy & physical therapies her pain was not relieving, Radiographs showed a few bony ossicles over lateral epicondyle and lateral radiocapitalum joint (A), however no bony abnormalities in anterior and posterior elbow (B).
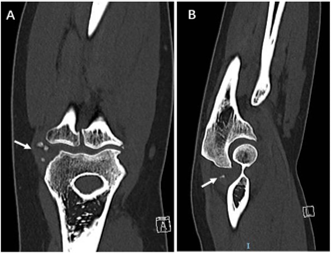
Figure 2: CT scans showed that calcified fragaments for ossicles over lateral elbow joint (arrow) and a tiny calcification lesion at the olecranon fossa.
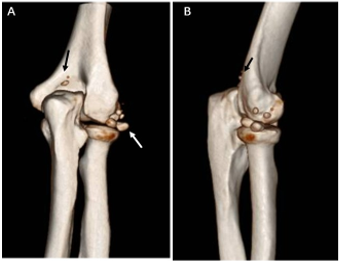
Figure 3: Three-D CT reconstruction images of the right elbow showed that multiple bony ossicles at lateral elbow (x5) (a white arrow) and olecranon fossa (x2) (black arrows)
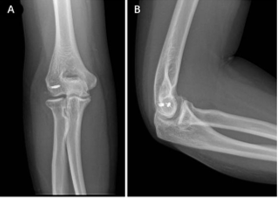
Figure 4. Because of her lateral elbow instability and pain, surgical excision ossicles and LUCL repair was performed with two bone anchors (an arrow). After surgery, her pain was completely relieved with full ROM elbow at the follow ups. Radiographs showed no loose bodies or osteochondral lesions
However, on clinical examination, she has laxity lateral elbow joint with collateral ligament stress test positive and chair pushing up test+ and elbow pivert shift test + indicating LUCL chronic instability. Two years after index surgery, she has complained the elbow pain and progressively worsening on ROM; joint with flex up to 90 degrees and extension blocking in 30 degrees to full extension (FFD 30 degrees). The lateral and the A-P radiographs of the elbow showed numerous chondral calcifications (Figure 5). CT scans showed osteochondral lesions at anterior and posterior parts of the elbow (Figure 6). Sagittal view of CT scans showed that posterior capitalum bony defect indicating previous intra articularly osteochondral injuries (traumatic OCD lesion) (Figure 7). Prior to second surgery, CT angiogram scans showed the humerus artery at least 10 mm anterior to anterior elbow osteochondral lesion, relatively safe for arthroscopically assisted surgery (Figure 8).

Figure 5. Two years after index surgery, she has elbow pain and progressively worsening on ROM of the elbow with flexion up to 90 degrees and extension blocking in 30 degrees to full extension (FFD 30 degrees). Radiographs showed osteochondral calcification in front of the coronoid process and olecranon fossa (arrows)
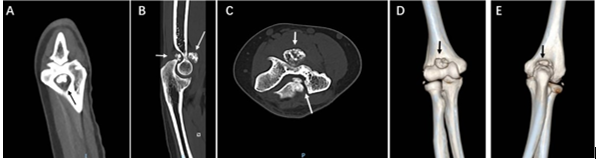
Figure 6: Two years after index surgery, CT scans showed anterior and posterior elbow osteochondral lesions (arrows).
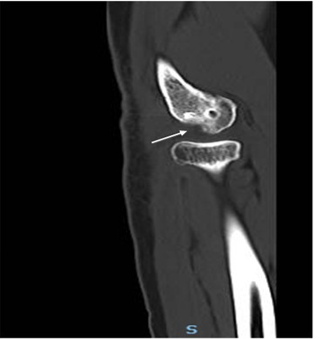
Figure 7: Sagittal view of CT scans showed that posterior capitalum bony defect indicating previous intra articularly osteochondral injuries (traumatic OCD lesion)
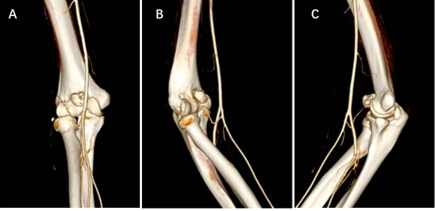
Figure 8. Two years after index surgery, CT angiogram scans showed the humerus artery at least 10 mm anterior to anterior elbow osteochondral lesion (arrows in B and C), relatively safe to do arthroscopically surgery
Under the general anesthesia, the patient was in the prone position, posterior compartment arthroscopy was performed with the posterolateral portal as the viewing portal and the posterior central portal as the working portal. The loose bodies were removed and synovectomy was performed. This was followed by lateral compartment arthroscopy with the posterolateral portal as the viewing portal and the soft spot portal as the working portal. Loose bodies were removed and synovectomy was performed with special focus on the synovial recess deep to the annular ligament. Finally, anterior compartment arthroscopy was performed via the proximal medial and anterolateral portals. With the anterolateral portal as the viewing portal and the proximal medial portal as the working portal, the adherent chondral synovium body is cut into two pieces and then removed. Gross synovium chondromatosis lesions (cut in two pieces) displayed pedicles attached on synovium tissues and covered with membrane of synovium tissues (Figure 9). Arthroscopically a synovium chondromatosis lesion sitting between medial and lateral humoral condyles was impinged on coronoid process (10 A). In B, an arrow indicated the bed of the synovium chondromatosis lesion after removal, clearly showed synovium tissue adhering on it (Figure 10). Synovectomy of the medial half of the anterior compartment was performed. With the proximal medial portal as the viewing portal and the anterolateral portal as the working portal, a large osteochondral mass at the center part of the anterior compartment were removed. Synovectomy of the lateral half of the anterior compartment was performed.
A month post 2nd surgery, radiographs showed no osteochondral lesions in anterior and posterior elbow joint (a little calcification dot was present inside lateral collateral ligament rather than intra articularly (Figure 11).

Figure 9. Gross synovium chondromatosis lesions (cut in two pieces) displayed pedicles attached on synovium tissues and covered with membrane of synovium tissues (arrows).
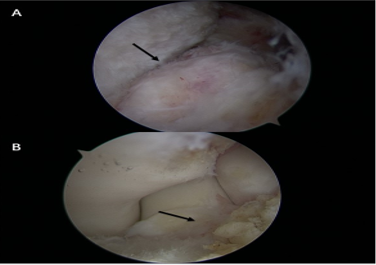
Figure 10: Arthroscopically a synovium chondromatosis lesion sitting between medial and lateral humoral condyles was impinged on the coronoid process (an arrow in A); In B, an arrow indicated the bed of the synovium chondromatosis lesion after removal, clearly showed synovium tissue adhering on it.
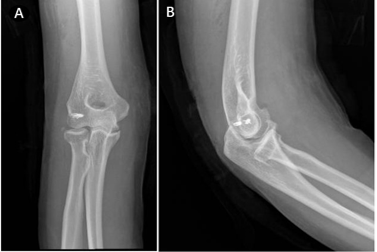
Figure 11. A month post 2nd surgery, radiographs showed no osteochondral lesions in anterior and posterior elbow joint (arrows) (lateral little ossicle was present inside lateral collateral ligament rather than intra articularly).
Pathology study confirmed our preoperative diagnosis of synovium osteochondromatosis that comprise areas of the mature hyaline cartilage, a cluster of chondrocytes in various stages of calcification (Fig 12)
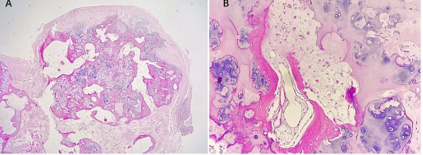
Figure 12. A hyaline cartilage nodule surrounded by a thin synovial membrane (an arrow) is seen in various stages of calcification and ossification chondrocytes, mild atypia, binucleate cells, and occasional mitoses (low power view x10x2) (A). The cartilage nodule with ossification and some chondrocytes with mild atypia (an arrow in B) (high power view x10x40).
The patient was started on a gentle ROM exercises and she had an elbow flexion of 130˚ and full pronation-supination, and extension of the elbow at her a year follow up postoperatively.
Synovial chondromatosis should be kept in the differential diagnosis of painful limitation of range of motion of the joints. The symptoms and signs are not specific, hence, several differential diagnosis should be kept in mind [5]. The calcified nodules in the joint should be suspected synovial originated chondromatosis as the possible source of symptoms related with joint like pain, effusion and locking [2].
Radiographic manifestations are usually pathognomonic for the diagnosis. Multiple calcified loose bodies can be seen in the joint in radiographs. Computed tomography (CT) optimally depicts the calcified intraarticular fragments and extrinsic bone erosion. However, because the radio-opacity cannot be detected in 1/3 of the cases diagnosis become difficult [2]. In our case, initial x-rays and CT scan did not show any intra articular synovium osteochondral calcifications at the initial presentation (Figure 1).
Milgram has reported that multiple loose bodies can be found without any synovial metaplasia and divide the disease into three separate phases; stage one is synovial chondromatoplasia but no loose bodies, stage two is the active synovial disease and formation of loose bodies, stage three is the late stage with loose bodies but no synovial disease [6]. Our patient’s lesions were corresponding to stage one of Milgram on initial presentation. It regresses to stage two in two years’ time and although it is very rare, malignant transformation of synovial chondromatosis can occur [7]. It should be suspected in chronic cases where acute exacerbation of symptoms of pain (night pain) and swelling occur.
Treatment modalities include arthroscopic or open extraction of the synovium loose bodies and arthroplasty in the presence of late stage of osteoarthritis due to long-term insults from chondromatosis lesions for articular cartilages.
The synovial chondromatosis, that is chondroid metaplasia in the synovium, should be kept in the differential diagnosis of the chronic monoarticular pain and painful limitations of the range of motions of the joints. Most common differential diagnoses include other conditions in which inflammation of the synovial membrane and loose body formation occur (secondary synovial chondromatosis), e.g., osteoarthritis, trauma, and osteochondritis dissecans. [8]
Symptoms of synovial chondromatosis can be grouped as inflammatory, mechanical, and due to pressure effects. [8] Sudden onset of severe loss of elbow extension and flexion in range of motion can occur as caused by mechanical blockage from interposition of chondral fragments in the olecranon and coronoid fossa, respectively and this is always associated with severe pain [9]. The pressure effects of an increasing volume of synovium together with the development of synovium loose bodies can by itself cause intrusive pain [8]. Neurologic symptoms also may develop due to the pressure effects on adjacent nerves, particularly the ulnar nerve, although lesions of the posterior interosseous and median nerves have been reported [8].
Secondary synovial chondromatosis is a rare condition characterized by the growth of particles separated from the articular cartilage or osteophytes in joint diseases [10]. Pain relief can be achieved by nonsurgical therapy in phase I (nonsteroidal anti-inflammatory medications and corticosteroid injection). Surgical treatment has been recommended as the first choice of therapy in stages II and III. Both arthroscopic and open synovectomy for removal of loose bodies could give a satisfactory result, but the arthroscopic approach has many advantages, including a shorter rehabilitation period and greater patient satisfaction [10], and less soft-tissue trauma, better cosmetic result, and fewer wound complications. The potential risks of this technique include nerve injury (ulnar, median or radial nerves), incomplete synovectomy and recurrence of the disease, residual loose bodies, compartment syndrome of forearm due to excessive extravasation, triceps tendon injury, and damage of the articular cartilage.
In conclusion, Synovial chondromatosis of the elbow is not a common condition that presents as multiple hyaline cartilage nodules within sub synovial connective tissue which is different from loose bodies. Arthroscopically assisted excision of synovium is an alternative way to prevent the recurrence and late stage osteoarthritis development. Compared with open procedures, the arthroscopic approach has many advantages, including a shorter rehabilitation duration and higher patient satisfaction.