AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2690-8808/019
1* Works in Sacramento, CA and specializes in Other Specialty.
*Corresponding Author: Louis DeVoe, Works in Sacramento, CA and specializes in Other Specialty.
Citation: Louis D Voe, Farid A, Lam M, David T Barba, Venugopal S, (2020) Of Equestrians and Endocarditis. J Clinical Case Reports and Studies, 1(4): Doi: 10.31579/2690-8808/019
Copyright: © 2020. Louis DeVoe. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 21 July 2020 | Accepted: 30 October 2020 | Published: 10 August 2020
Keywords: streptococcus zooepidemicus; endocarditis; encephalitis; immunocompromised host; group-B streptococcus
an 80-year old female was transferred from an outside hospital for concerns of a mitral valve vegetation and sepsis. Her past medical history included untreated chronic lymphocytic leukemia (CLL) and atrial fibrillation on warfarin therapy. The patient was otherwise very active and enjoyed daily rides on her horses. She initially presented with altered mental status and was found to be in septic shock with respiratory failure requiring intubation. Initial head CT showed an ischemic stroke in the bilateral frontal lobes. Echocardiogram showed a large mitral valve vegetation. A repeat CT of her head obtained for clinical decline revealed hemorrhagic conversion of her ischemic stroke. She began to have seizure activity that was treated with Keppra. Blood cultures grew Streptococcus zooepidemicus, and she was subsequently transferred to our tertiary medical center for increased level of care.
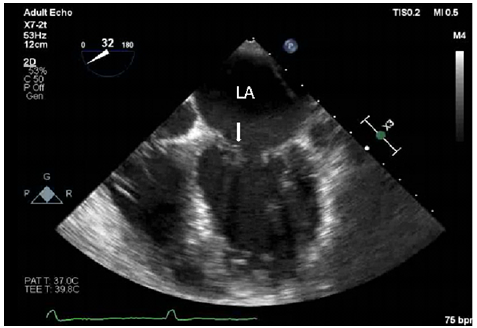
An 80-year old female was transferred from an outside hospital for concerns of a mitral valve vegetation and sepsis. Her past medical history included untreated chronic lymphocytic leukemia (CLL) and atrial fibrillation on warfarin therapy. The patient was otherwise very active and enjoyed daily rides on her horses. She initially presented with altered mental status and was found to be in septic shock with respiratory failure requiring intubation. Initial head CT showed an ischemic stroke in the bilateral frontal lobes. Echocardiogram showed a large mitral valve vegetation. A repeat CT of her head obtained for clinical decline revealed hemorrhagic conversion of her ischemic stroke. She began to have seizure activity that was treated with Keppra. Blood cultures grew Streptococcus zooepidemicus, and she was subsequently transferred to our tertiary medical center for increased level of care.
The patient arrived at the cardiac care unit intubated, afebrile, with blood pressure 165/94 mm Hg, pulse of 105 beats per minute, respiratory rate of 16 breaths per minute, and oxygen saturation of 98% on minimal ventilator settings. She had a Glasgow Coma Scale score of 3T without sedation. There was no noticeable jugular venous distention. Lungs were clear to auscultation bilaterally with associated ventilator sounds. Cardiac point of maximal impulse was non-displaced. The neurologic examination was notable for intact brainstem reflexes, but the patient was otherwise obtunded. When a sternal rub was performed, the patient had no response. There was no localization to the pain, no grimacing, and no posturing.
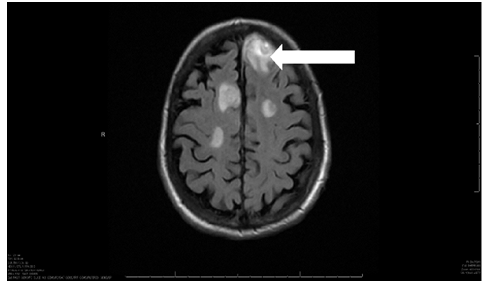
The electrocardiogram (ECG) showed atrial fibrillation with incomplete right bundle branch block. Laboratory data was notable for elevated white blood cell count (WBC) to 101.3 K/MM^3, elevated troponin 2219ng/L, and creatinine 2.24mg/dL. The previously noted mitral valve vegetation was not seen on repeat transthoracic echocardiogram. A 0.4cm mobile mass on the anterior mitral valve was confirmed on transesophageal echocardiogram. Lumbar puncture revealed elevated protein and lymphocytes consistent with partially treated bacterial encephalitis. Repeat MRI/MRA confirmed a conversion of her ischemic stroke and concerns for evolving abscess formation, which was also consistent with the lumbar puncture results. EEG was obtained after consulting Neurology, which was concerning for non-convulsive status epilepticus despite patient being on seizure prophylaxis. Her anticonvulsants were escalated, and eventually she required a midazolam drip to break the non-convulsive status epilepticus.
The diagnosis of mitral valve endocarditis having been made, the patient was treated with vancomycin and ceftriaxone. Infectious disease was consulted regarding further management of the patient’s endocarditis and encephalitis. Ceftriaxone was continued based on sensitivities. The anti-seizure regimen was also narrowed to Keppra (levetiracetam) and Vimpat (lacosamide). Patient improved clinically and was eventually extubated. While she remained minimally responsive to questions, she was able to verbalize yes/no and answer questions appropriately. Physical therapy and occupational therapy were instituted. On hospital day 30, she was transferred back to the referring hospital for continued rehabilitation with the plan to continue her antibiotics for a 4-week course and her seizure prophylaxis for 3-6 months with follow-up brain MRI. The patient continued to improve clinically and eventually discharged home. She was seen in the infectious disease clinic two months following her initially presentation and noted to have made full neurologic recovery.
we present this case, a rare cause of endocarditis complicated by encephalitis, as a clinical dilemma because of the scarcity of literature concerning the infection by Streptococcus zooepidemicus in humans. To our knowledge, we present the first case of S. zooepidemicus, endocarditis that progressed to encephalitis. (1) (2) (3). This is also the first case of S. zooepidemicus endocarditis with radiologic imaging presented in the literature. Upon review of the literature, we encountered one case presented in 1979 of a patient who presented with endocarditis that resulted in seizures and altered mental status; however, the exact species of the Group C streptococcus was never specified. (4) A similar case was presented in 2013 where a patient developed S. zooepidemicus meningitis that progressed to endocarditis. (5)
While an established pathogen in equine medicine, Streptococcus zooepidemicus is not commonly seen in humans. It has a wide variety of clinical manifestations. Transmission from horses to humans has been established.8 Infection with S. zooepidemicus is also associated with drinking raw milk, and outbreaks in the past can be linked back to raw milk sources. (6) (7). This bacterial species is not localized to the United States and has been see throughout Europe, the Americas, Asia, as well as Australia. (8). Clinical manifestations can vary, from endocarditis and meningitis as seen in our patient to nephritis and post-streptococcal glomerulonephritis. While its treatment is straight forward, the clinical effect of this lesser known organism and the response of bacteria to appropriate antibiotics should not be ignored. (6)
The complexity of our patient presentation made the clinical course somewhat unclear. Initial neurologic symptoms were attributed to the patient’s ischemic to hemorrhagic conversion and underlying status epilepticus, less to her endocarditis. This case highlights the importance of coordinating care amongst the subspecialties of neurology and infectious disease as it was initially unclear as to how the endocarditis could result in her neurological manifestations, as they did not appear consistent with septic emboli. The coordination resulted in timely initiation of therapy to treat the endocarditis and encephalitis. Given the severity of the infection on presentation, it is important to note the responsiveness of this bacteria to antibiotics. Continuation of antibiotics was initially in question as it was unclear as to whether the patient’s clinical status was due to the bilateral frontal lobe stroke or due to her infection. The consultation with neurology provided us with a source of the altered mental status and infectious disease was able to advice on appropriate antibiotic treatment for the patient. In the end, the coordination of the Cardiac Care Team, Neurology, and Infectious Disease was able to navigate the winding path of this patients care.
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
All authors had access to the data and participated in writing the manuscript.
All authors declare that we have no conflicts of interest.