AUCTORES
Globalize your Research
Review Article | DOI: https://doi.org/10.31579/2692-9759/056
1 Cardiology Department, Faculty of Medicine, Zagazig University, Zagazig City 44519, Egypt.
2 College of Biotechnology, Misr University for Science and Technology (MUST), 6th October City 12566, Egypt.
3 Anatomy and Embryology Department, Faculty of Medicine, Zagazig University, Zagazig City 44519, Egypt.
*Corresponding Author: Abdelmonem Awad Hegazy, Anatomy and Embryology Department, Faculty of Medicine, Zagazig University, Zagazig City 44519, Egypt.
Citation: Hegazy MA; Kamal S Mansour KS; Alzyat AM; Mohammad MA, Hegazy AA. (2022). Myocardial Infarction: Risk Factors, Pathophysiology, Classification, Assessment and Management. Cardiology Research and Reports. 4(5); DOI: 10.31579/2692-9759/056
Copyright: © 2022, Abdelmonem Awad Hegazy. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 15 March 2022 | Accepted: 28 March 2022 | Published: 30 May 2022
Keywords: myocardial ischemia; cardiac enzymes; risk factors; management
Myocardial infarction is a serious health problem affecting populations worldwide. Proper and prompt diagnosis and management is critical to achieving good prognosis and avoiding or reducing morbidity and mortality. It is essential for clinicians to be aware of the risks, diagnosis and treatment. In this review we aim to update and discuss knowledge of myocardial infarction with respect to risk factors, pathophysiology, types or classification, clinical manifestations, diagnosis and treatment in a concise and simplified manner in order to define a simple comprehensive guide for clinicians. The available literature has been searched, reviewed, studied, analyzed, written in a simple understanding method, discussed and concluded. For prophylaxis, it has been found that moderate muscular exercise, regular consumption of fresh vegetables and fruits, avoidance of smoking and stress, and low consumption of fat are associated with reduced risk of coronary heart disease in populations of all age groups worldwide. The diagnosis of myocardial infarction is based primarily on evaluations of clinical features, typical abnormalities in ST-segment and T wave of ECG findings and rise in cardiac enzymes or biomarkers such as plasma troponin. At the same time, the key to treatment is reperfusion of the myocardium and restoration of coronary blood flow.
Myocardial infarction (MI) is sudden ischemia of the heart muscle tissue due to lack or obstruction of coronary blood flow, which leads to its damage (Frangogiannis, 2015). The heart muscle is anatomically fed by two major coronary arteries, the "right and left". Each one terminates by small branches supplying the myocardium from the epicardial side. The left circumflex and left anterior descending “anterior interventricular” arteries form the main two terminal branches of left coronary artery. Although there is anastomosis between the small terminal branches of the coronary arteries, this anastomosis is insufficient if one of them is occluded (Hegazy, 2018). Obstruction or stenosis of any of them leads to a decrease in coronary blood flow and thus the development of MI. The MI is a leading cause of death in developed countries and has become a growing health problem in developing countries other than infectious diseases. The ST-segment elevation myocardial infarction (STEMI) is defined by a characteristic clinical picture of myocardial ischemia associated with electrocardiographic (ECG) ST-segment elevation suggestive of coronary occlusion (Gaziano et al, 2010; Kushner and Bates, 2013). Although this is difficult to be fully ascertained, it is estimated that approximately 500,000 patients in the United States are affected by ST-elevation myocardial infarction annually (Antman et al, 2004). Coronary artery disease (CAD) mortality in the United States was approximately 17% of all deaths in 2007 (Roger et al, 2011).
In 2001, there were about 7.3 million deaths from coronary heart disease (CHD). About three-quarters are encountered in low- and middle-income countries. This represents an increasing health burden on the economies of these countries. The escalating increase is attributed to changes in lifestyle and increased life span with acquisition of more relevant risk factors (Gaziano et al, 2010). It was noted that the mortality rate among males is higher than among females at young ages. However, it often converges with age (Bots et al, 2017).
Since the damage from myocardial infarction is irreversible, it is essential to properly diagnose and resuscitate the heart as soon as possible when expected in patients. The sooner treatment takes place less than 6 hours after symptoms appear, the better the prognosis (Mechanic et al, 2021). Therefore, the aim of the current review is to update knowledge of myocardial infarction regarding risk causes, clinical manifestations, diagnosis and treatment in a concise and simplified manner in order to be a simple guide for clinicians in the accurate and rapid management of myocardial infarction.
Risk factors
The onset of acute myocardial infarction (AMI) is strongly associated with some risk factors (RFs). Such RFs are defined as clinical or laboratory elements associated with the likelihood of disease onset and progression in a time period. Identification of RFs is important for approaches to preventing most premature MI (Yusuf et al, 2004). The RFs include smoking five or more cigarettes per day, diabetes with a blood glucose level of ≥126 mg/dL, hypertension, central obesity, and low-density lipoprotein cholesterol from 100 to 120 mg/dL (Piegas et al, 2003). However, there are other factors called non-modifiable RFs including age above 45 years for males and above 55 years for females, African American race and previous family history of early CAD (Harrington et al, 2018).
Smoking
Smoking is the main independent risk factor for AMI morbidity and mortality. There is a direct relationship between CAD and the duration and amount of tobacco consumed (Prescott et al, 1998). Smoking is responsible for about 10% of deaths which is expected to increase to about 17% by 2030 (Piegas et al, 2003). Its mechanism on coronary circulation appears to be complex and multifactorial. Tobacco smoking can exert its effect by increasing blood pressure and heart rate resulting in an increase in metabolic oxygen (O2) demand by the heart muscle. At the same time, it leads to vasoconstriction, which leads to a reduction in the dimensions of the coronary arteries and thus the flow of blood through them. These adverse effects with respect to myocardial O2 supply and requirements can be exacerbated by concomitant use of cocaine with cigarette smoking (Moliterno et al, 1994).
Alemu et al (2011) found that cigarette smoking may worsen right coronary circulation and thus inferior wall AMI more than left coronary artery and anterior wall infarction. However, they added that the mechanism of this difference is not clear.
Hypertension
Hypertension is an important risk factor for CAD and AMI. There is a direct association between high blood pressure values and morbidity and mortality of CAD. Furthermore, proper management of hypertension may reduce the burden of AMI in morbidity and mortality (Kaplan et al, 1999). With high blood pressure, the risk of developing AMI has been found to increase to more than twofold (Piegas et al, 2003).
Diabetes mellitus
Diabetes mellitus (DM) is a well-documented risk factor for CAD and AMI. Myocardial infarction (MI) is more common in diabetic patients than in non-diabetic people. Moreover, DM and hyperglycemia are high-RFs for mortality in cases of MI (Stevens et al, 2004). The pathophysiology of DM in causing MI is the long-term insulin resistance associated with hyperglycemia; hence compensatory hyperinsulinemia occurs. Insulin resistance, hyperglycemia and excess fatty acids lead to increased systemic oxidative stress and inflammation as well as production of advanced glycation product. All of these factors contribute to the emergence and development of coronary atherosclerosis and microvascular impairment (Severino et al, 2019).
Anthropometric measures
Although body weight appears to predict obesity, its values do not differentiate between body fat and muscle mass. Moreover, central fat has more to do with the development of atherosclerosis than peripheral obesity (Siavash et al, 2008). Therefore, other anthropometric measures such as waist circumference (WC), waist/hip ratio (WHR), and waist/thigh ratio (WTR) are suggested to be more indicative of CAD risk (Zhang et al, 2008).
Body mass index (BMI), waist/hip ratio (WHR) and waist/thigh ratio (WTR) are considered independent RFs for CAD and AMI. Presence of both BMI and WHR is a great predictor for routine investigation of people at risk for CAD (Oshaug et al, 1995; Borné et al, 2014; Baghbani-Oskouei and Gholampourdehaki, 2020). Central obesity is greater indicator in CAD risk than generalized obesity. It has been observed that elevated WC is associated with significant increase in CVD mortality even in people of normal weight (Zhang et al, 2008).
Blood lipids
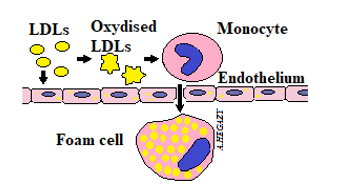
The low-density lipoprotein (LDL)-cholesterol is associated with development of atherosclerosis, endothelial dysfunction and arterial plaques that represent the potential cause of CAD and stroke (Linton et al, 2019). The role of oxidized LDL (oxLDL) in atherosclerosis pathogenesis in endothelial injury and dysfunction is attributed to activation of lectin-like oxLDL receptor-1 (LOX-1) (Szmitko et al, 2003) (Fig. 1). Such LOX-1 represents the major receptor of endothelial cells for oxLDL. It could be expressed in the invading smooth muscle cells (SMCs) and macrophages (Yoshida et al, 1998; Aoyama et al, 2000).
Only LDL-cholesterol seems to be independent risk factor. It has been noticed that LDL-cholesterol, and triglyceride were increased in cases of CAD, while high-density lipoprotein (HDL)-cholesterol was elevated in control groups (Piegas et al, 2003).
Inflammation
There are accumulating data that the inflammation is considered a major risk factor for atherosclerosis development perhaps exceeding the role of LDL (Libby et al, 2002; Smit et al, 2019). Increased levels of highly sensitive C-reactive protein (CRP) could be an indicator of CHD risk in healthy individuals irrespective of LDL values. Moreover, it is believed that the statins’ role in protection against CAD is attributed to its role in reducing the inflammation. This is evident through decreasing the levels of inflammation markers including CRP (Diamantis et al, 2017).
Alcohol intake
The effect of excessive drinking doubles the risk of developing AMI compared to not drinking alcohol. However, some authors suggest that low consumption may have a beneficial effect on myocardial infarction (Ilic et al, 2018). Such benefit is thought to be achieved by increasing HDL-cholesterol, rather than effecting platelets and fibrinolysis (Suh et al, 1992; Piegas et al, 2003). Despite the suggested benefit of reduced alcohol consumption, it is not recommended due to the known harmful effect of excessive alcohol intake (Suh et al, 1992).
Socioeconomic status
Socioeconomic status is associated with CAD and AMI risks. There is an inverse relationship between the education level and AMI; individuals with elementary school education are most affected, regardless of social class (González-Zobl et al, 2010). Moreover, individuals with low incomes and material deprivation are exposed to excessive psychosocial stress that is detrimental to overall health including the cardiovascular system. This may also happen by adopting unhealthy behavior such as smoking which can exacerbate the risks (Piegas et al, 2003).
Family history
Family history especially for the first-degree relatives is considered to be an independent risk factor for AMI. However, family history is not a simple factor, but it results from interactions among many other factors such as environmental factors and genetic susceptibility (Ranthe et al, 2015).
It has been claimed that about 40% to 60% of coronary heart disease is inherited (Roberts and Stewart, 2012). Previous reports have suggested the involvement of more than 40 common genetic variants in the risk of CAD (Roberts and Stewart, 2012; Deloukas et al, 2013). Therefore, taking a detailed family history may be necessary especially in patients between 35 and 55 years of age for appropriate assessment of AMI risk (Ranthe et al, 2015).
It has been found that moderate muscle exercise, regular consumption of fresh vegetables and fruits, avoidance of smoking and stress, and low consumption of fat are associated with reduced risk of coronary heart disease in populations of all age groups worldwide (Yusuf et al, 2004).
Pathophysiology of myocardial infarction
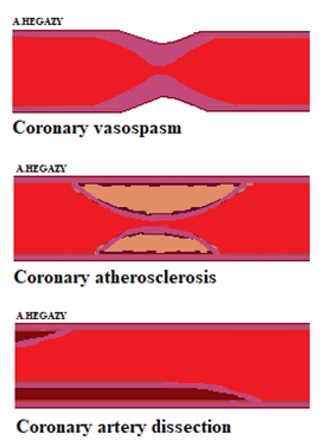
Myocardial infarction (MI) results from a severe and prolonged imbalance between the myocardial O2 supply and its requirements. In most cases, this occurs as a result of occlusive coronary atherosclerosis superimposed with luminal thrombus (Christia and Frangogiannis, 2013). The atherosclerosis is a dynamic, progressive process. Its effects are attributed to a combination of inflammation and endothelial dysfunction (Szmitko et al, 2003). In about 10% of cases, myocardial infarction may occur without detection of coronary artery obstruction. The prognosis and management in such cases are different from coronary artery occlusion (Niccoli and Camici, 2020). The exact mechanism in non-obstructive cases has not yet been clearly established. However, some potential causes such as coronary artery spasm, plaque disruption, spontaneous coronary artery dissection, in-situ thrombosis and microvascular dysfunction have been suggested (Tamis-Holland et al, 2019; Hegazy et al, 2022). In these cases, it is important to rule out other causes of elevated troponin such as myocarditis, Takotsubo cardiomyopathy and pulmonary embolism (Li et al, 2020).
The central mechanism of the pathophysiology is the same regardless of the etiological factors that may only modify the outcome. For example, hypertension is a main risk factor involved in strokes while smoking increases the incidence of MI (Bentzon et al, 2014).
The pathophysiology process can be summarized in the following steps:
Endothelial dysfunction
Coronary endothelial dysfunction precedes the lesion formation and increases with progression of CAD. It results from endothelial injury that occurs in response to oxidized LDL, increased levels of blood glucose, hypertension and increased free radicals derived from oxygen. There is usually a decrease in release of endothelial nitric oxide (NO) that affects vasomotion; thus, an increase in platelet and monocyte adhesions occurs with increased smooth muscle cell proliferation (Lüscher et al, 2009). The NO inhibits atherogenesis by promoting vasodilation and reducing the platelets’ adhesions to the vascular endothelium (de Graaf et al, 1992).
Plaque and necrotic core formation
Atherosclerosis is the main cause of plaque formation by causing internal inflammation, fibrosis, necrosis and calcification. The direct mechanism is through accumulation of LDLs in the arterial endothelium with an intrinsic adaptive thickening (Bentzon et al, 2014). Then, LDLs become modified by oxidation as well as aggregation. The modified LDLs produce chronic stimulation of innate and adaptive immunity resulting in differentiation of monocytes to phagocytes (Fig. 1). These phagocytes engulf lipid particles forming so-called foam cells that are the hallmark of atherosclerotic plaques (Libby et al, 2011). The endothelium is then becoming leaky (Bentzon et al, 2014).
Matrix metallopeptidase 9 (MMP-9), also known as gelatinase B, 92-kDa type IV collagenase, has been produced by SMCs and macrophages in response to oxLDL, reactive oxygen specious (ROS) and tumor necrosis factor (TNF)- α (Galis and Khatri, 2002). The level of MMP-9 is increased in cases of unstable angina and MI. Overexpression of MMP-9 enhances the process of atherosclerosis and fibrous cap degradation of plaques and intravascular thrombosis (Belaaouaj et al, 2000; Morishige et al, 2003).
Inflammation contributes to foam cell death and muscle fibers’ migration. This could result in formation of necrotic core within the plaque. Therefore, a mature atheromatous plaque is composed of a lipid-rich necrotic core surrounded by collagen rich capsule (Smit et al, 2019).
Plaque angiogenesis and intervening hemorrhage
New vessels originate from the vasa vasorum within the vessel adventitia and give another route for monocytes and immune cells to reach the base of atheromatous plaque (Kumamoto et al, 1995). These vessels are fragile resulting in bleeding and extravasation leakage to erythrocytes and plasma proteins. Such bleeding expands the plaque and promotes occurrence of more inflammation. Moreover, rupture of fibrous cap of plaque is another cause for bleeding (Bentzon et al, 2014).
Fibrous cap rupture and thrombosis
Plaque rupture occurs through the thin fibrous cap. Rupture of vulnerable plaque could be preceded by severe exertion. The increase in amount of free cholesterol and phagocytes’ infiltration in the plaque cap as well as the decrease in its thickness are factors involved in rupture mechanism (Burke et al, 1999). Plaque rupture might occur spontaneously; however, in other cases it could be triggered by psychological, physical or sexual stress, infections or substance abuse (Mittleman and Mostofsky, 2011). The triggered pathways’ mechanism might be hastened through the increase in the blood pressure and heart rate leading to plaque rupture or via increasing the coagulability and thrombosis of platelets superimposed on already vulnerable plaque (Martin et al, 2012; Bentzon et al, 2014).
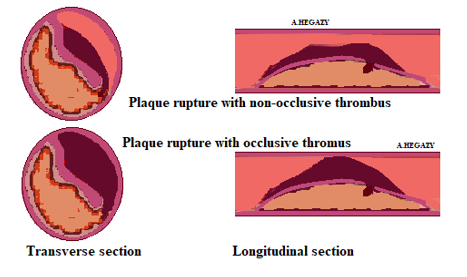
Plaque rupture leads to exposure of blood with the necrotic core that is rich with erythrocytes and highly thrombogenic material leading to clot formation. Plaque rupture represents the most common cause for occurrence of thrombosis (Bentzon et al, 2014). This might be associated with acute coronary syndromes and myocardial infarction. The occlusive and sustained thrombosis often accompanies cases of ESTMI; however, in non- ESTMI, the thrombus is often dynamic and does not clog the vessel or is even absent (Davies, 2000).
Classification of Myocardial Infarction
There are generally two MI categories; MI with elevation or non-elevation of ST-segment in electrocardiogram (ECG) known as STEMI and STEMI respectively. This classification is usually adopted for patients with chest ischemic manifestations in order to sake immediate management including reperfusion therapy. However, there is another classification made according to international consensus into 5 categories (Thygesen et al, 2018). These include the followings:
Type 1 “spontaneous MI”
This type MI is associated with atherosclerotic plaque disruption such as rupture, erosion, fissuring or dissection (Fig. 2). It may be complicated by intraluminal thrombosis and distal emboli. There may also be intraplaque hemorrhage through surface disruption of plaque cap (Falk et al, 2013; Bentzon et al, 2014).
Type 2 “ischemic-related MI”
This myocardial infarction is associated with myocardial ischemia. It is caused by an imbalance between supply and demand for O2 to the heart muscle (Chapman et al, 2017). Cases of decreased blood supply include shock, defined by hypotension below 90 mm Hg associated with organ dysfunctions’ signs. They also include anemia with hemoglobin less than 5.0 mmol/L, respiratory failure, bradycardia, arrhythmia and coronary artery spasm, dissection or atherosclerosis. On the other hand, increased demands occur in conditions such as tachycardia of twenty minutes or more, and hypertension of systolic pressure over 160 mm Hg associated with ventricular hypertrophy (Fig. 3) (Saaby et al, 2013; DeFilippis et al, 2019).
Type 3 “sudden unexpected cardiac death without cardiac biomarkers’ evidence”
In this type, sudden, unexpected death occurs before an elevation of cardiac biomarkers or when evidence is lacking even though the signs and symptoms are suggestive of a myocardial infarction. (Thygesen et al, 2018).
Type 4 “percutaneous coronary procedure-related MI”
This MI is associated with medical interference including 2 types: Type 4a resulting from percutaneous coronary intervention (PCI) or type 4b that might follow coronary stent placement (Chapman et al, 2017). It may occur periprocedural or later on reflecting a complication for the stent or device like stent thrombosis or restenosis. It may be discovered by angiography or postmortem at autopsy (Rahimi et al, 2009; Thygesen et al, 2018).
Type 5 “cardiac surgery-related MI”
In this case, MI is associated with coronary artery bypass grafting (CABG). It has been reported that CABG has a higher mortality rate than percutaneous coronary intervention (PCI). Furthermore, there is no further benefit to CABG over PCI (Head et al, 2018).
Type | Name | Main Characters |
1 | Spontaneous MI |
|
2 | Ischemic-related MI |
|
3 | MI with sudden unexpected cardiac death |
|
4 | Percutaneous coronary procedure-related MI |
|
5 | Cardiac surgery-related MI |
|
Table 1: Main types of myocardial infarction (MI)
Diagnosis of MI
Evaluation of myocardial infarction is based on evaluations for the presence of risk factors, clinical features, typical abnormalities in ST-segment and T wave of ECG findings and rise in cardiac enzymes or biomarkers such as plasma troponin (Sharma et al, 2004; Barstow et al, 2017).
Clinical manifestations
A prompt and focused patient history taking and a complete physical examination is essential to exclude or identify any risk factor that could be mitigated or managed (Nellen et al, 1973; Wasalwar and Wasnik, 2020). The most common symptom in MI is the chest pain (Barstow et al, 2017). Although there is atypical chest pain, the usual presentation is a "heavy chest pressure" or burning sensation, associated with difficulty breathing and extending to the left side of the jaw, neck, shoulder, or upper arm (Malik et al, 2013). There are other non-cardiac causes of chest pain. Therefore, it is necessary not to rely on the initial evaluation, but it is necessary to be motivated to embark on further investigations. Chest pain represents an ischemic damage caused by coronary artery occlusion or reduction in O2 supply to fulfil demands of myocardium (Barstow et al, 2017).
Cardiac biomarkers
Cardiac biomarkers have been essential tools in cardiology clinics since their use for the past 50 years. Their discovery, in particular troponin, represents a new era for improving the management of patients with heart disease (Mair et al, 2015).
The MI has been defined by WHO “World Health Organization” in 1970s by having at least two of following characteristics: 1) Chest pain characteristic of cardiac ischemia, 2) development of Q waves in ECG and 3) increased blood enzymes including total creatine kinase (CK), CK-myocardial band, lactate dehydrogenase and aspartate aminotransferase. Then, in 1999, cardiac troponins (cTn) have been introduced as the gold standard for diagnosing MI (Alpert et al, 2000; Mythili and Malathi, 2015).
Troponin may be the only biomarker recommended in the diagnosis of myocardial infarction. Its accuracy in diagnosis has been greatly improved through the use of more sensitive assays that allow detection of its concentration even in healthy people and thus the development of a more accurate reference range for MI (Apple et al, 2012; Chapman et al, 2017). The use of cardiac troponin has developed significantly in clinical practice for its use not only in the detection of patients with myocardial infarction but also as an ongoing measure of risk (Shah et al, 2015; Chapman et al, 2017).
Troponins (T or I) have more specificity and sensitivity than that of cardiac enzymes. They are cardiac proteins, regulating myocardial contraction by controlling interactions mediated by calcium between actin and myosin. Although traces of troponin T might be expressed in skeletal muscles, both regulatory proteins “troponins T and I” are theoretically specific to myocardium (Sharma et al, 2004). Troponin levels that are very low in healthy individuals are significantly increased in case of myocardial injury. Elevated cardiac troponin levels are accepted as the standard diagnosis of signs of MI (Braunwald et al, 2000). Myocardial injury is diagnosed when the level reaches more than 99th of upper reference level (URL) of ≥0.045 ng/ml (Acosta et al, 2020).
Other authors suggested the high-sensitivity C-reactive protein as cardiac biomarker used for prediction of heart failure (HF) that might occur as a complication of MI (Mair et al, 2015; Al Aseri et al, 2019). This has been attributed to the important independent role of inflammatory process in development of HF following MI.
Lactate dehydrogenase (LDH) represents another biomarker for diagnosis of myocardial ischemia. It rises in blood within 6-12 hours after AMI. It peaks after 1-3 days and remains high for 1-2 weeks after which it returns to normal (Patibandla et al, 2021). The presence of elevated LDH values for up to 2 weeks makes it a late biomarker for AMI (Dasgupta and Wahed A, 2014). LDH is no longer used in the diagnosis of AMI. However, the only use of LDH can be to assess AMI to distinguish it from subacute conditions in those with elevated troponin values, normal creatine kinase (CK) and myocardial creatine kinase (CK-MB) band levels (Yun and Alpert, 1997).
Glycogen phosphorylase BB is a biomarker found in high concentration in the heart muscle and brain. It is released into circulation two to four hours after the onset of myocardial ischemia and returns to baseline normal levels 1-2 days after AMI, so it is an early biomarker (Dasgupta and Wahed A, 2014).
Myoglobin (MYO) is an oxygen-binding protein located in the cytoplasm of skeletal and cardiac muscles. It is released early in the serum, about 1 hour after the onset of myocardial ischemia, peaks at 4-12 hours and immediately returns to baseline levels. Its disadvantage is attirbuted to the lack of specificity of the heart muscle due to its presence in the skeletal muscles. Therefore, it can be used to rule out the presence of AMI; not to diagnose (Mythili and Malathi, 2015).
Other laboratory investigations
Laboratory tests in cases of AMI include a complete blood count (CBC), kidney function tests, a lipid profile, and a metabolic panel. B-type natriuretic peptide (BNP) should not be considered as a marker of AMI; Alternatively, it can be used to determine the prognosis of risk, especially in cases of heart failure. Hemoglobin level is important to rule out anemia as a cause of hypoxia. Moreover, the platelet count is determined before anticoagulant drugs are administered. Creatinine level is required before administration of an angiotensin-converting enzyme (ACE) inhibitor. The lipid profile is examined at the time of stroke as its level changes 12-24 hours after the acute phase. Furthermore, identification of C-reactive protein and other markers indicative of inflammation is of great interest in laboratory investigations (Gupta, 2009).
Diagnostic testing
1- Electrocardiogram (ECG)
An electrocardiogram (ECG) is available as a non-invasive method used to diagnose myocardial infarction. Prompt ECG prediction associated with infarction as soon as it is suspected can facilitate management and avoid complications (Mamun et al, 2017). This must be done within 10 minutes of medical referral (Thygesen et al, 2018). One of the well-established ECG manifestations in acute infarction is the changes in ST-segment. The elevation magnitude of ST-segment is considered an indicator of the degree of infarction (Guo et al, 2000). Criteria for ECG changes that occur in AMI patients who may benefit from early reperfusion include: ST-segment elevation (STSE) in at least two contiguous leads and new left bundle branch block. Moreover, ST-segment depression in right leads “V1-V3” indicating posterior AMI associated with posterior lead STSE could be another ECG indication for urgent reperfusion therapy such as thrombolytic agents. Coronary angioplasty is also beneficial if it is applied as soon as possible (Brady and Morris, 2000). Perfusion is usually accompanied with a rapid and marked reduction in STSE (Thygesen et al, 2018).
The ST-segment shifts or T wave inversions including multiple leads are usually good evidence of myocardial ischemia. Association of ST-segment depression ≥ 1 mm in 6 leads and STSE in leads aVR or lead V1 indicates multivessel lesion or left main disease. Presence of pathologic Q waves increases the risk of prognosis. ECG is not a sufficient tool for diagnosis of AMI. This is because ST-segment deviation might be present in other disorders such as left ventricle hypertrophy, left bundle branch block or acute pericarditis (Thygesen et al, 2018).
2- Echocardiography
Echocardiography might be the non-invasive method option for visual assessment of myocardial functions. It represents a facilitation method for estimating impairment of blood flow to myocardium (Alizadehasl et al, 2017). Contrast echocardiography using intravenous administration of microbubble contrast agents has improved the visualization. It can be used clinically to detect and evaluate suspected or known CAD, as well as identify areas of the myocardium at risk and evaluate reperfusion therapies in cases of AMI (Trindade et al, 2013).
Differential diagnosis
All cases of AMI should be differentially diagnosed from other causes of abnormalities of ST-segment such as acute pericarditis, myocarditis, pulmonary embolism, intracranial processes, hypothermia and electrolyte abnormalities (Thygesen et al, 2018). Also, differential diagnosis of AMI includes other causes of chest pain such as musculoskeletal elements, cholecystitis, acute pancreatitis, peptic ulcer, acid gastroesophageal reflux and esophageal spasm (Gupta, 2009; McConaghy and Oza, 2013). They can be categorized into associated pathological ischemia, ST-section elevation but without ischemia, and chest pain associated with ischemia (Table 2) (Griffin et al, 2000).
| Condition | Causes |
1 | Comorbid ischemia | Aortic dissection |
Aortic stenosis | ||
Systemic arterial embolism | ||
Hypertensive crisis | ||
Arteritis | ||
Cocaine abuse | ||
2 | ST-segment elevation without ischemia | Early repolarization |
Left bundle branch block | ||
Left ventricular hypertrophy | ||
Hyperkalemia | ||
Burgada syndrome | ||
3 | Chest pain with ischemia | Aortic dissection |
Myopericarditis | ||
Pulmonary embolism | ||
Pleuritis | ||
Costochondritis | ||
Gastrointestinal disorders |
Table 2: Differential diagnosis of myocardial infarction
Therapy
Prior to reperfusion
1- Aspirin
Immediate aspirin intake is a significant benefit unless contraindicated due to a clear history of allergy. Dosage can be around 325mg, preferably chewable for quick absorption. If the oral route is not available, it can be given as rectal suppositories. If the patient is allergic to aspirin, clopidogrel monotherapy is an alternative (Griffin et al, 2013). It is suggested that the combination of aspirin and clopidogrel be as safe as using aspirin alone in reducing ischemic stroke (Rahman et al, 2019). However, other authors agree that the combination has a lower risk but is associated with a higher likelihood of bleeding than those using aspirin alone over a 90-day period (Johnston et al, 2018).
2- Oxygen therapy
Oxygen (O2) should be given for all suspected cases of AMI. It can be given with a face mask or through an endotracheal tube (Griffin et al, 2013). O2 is indicated to cases of AMI depending on fact that the ischemic heart diseases are caused by interruption of O2 supply of myocardium for a sustained period. Therefore, O2 supplementation could improve the myocardial oxygenation, reduce the associated pain, minimize the size of infarction and consequently reduce mortality. However, some authors thought that O2 might be biologically harmful. They attribute their proposal to its paradoxical effect in reducing coronary blood flow and strengthening coronary vascular resistance. (McNulty et al, 2007; Cabello et al, 2016). On the same line, Abuzaid et al (2018) confirmed that O2 therapy has no benefit in cases of AMI associated with normal O2 saturation levels. However, it could be of great value in cases with cardiogenic shock or severe pulmonary edema (Griffin et al, 2013).
3- Analgesia
Morphine
Morphine is recommended and commonly used to relieve chest pain secondary to myocardial tissue damage and to reduce the associated sympathetic activation that occurs with AMI. Such sympathetic activation can lead to an overload of the myocardium as well as vasoconstriction (Ibanez et al, 2018). In preclinical study, the authors have concluded that morphine could have a protective role against rat AMI through increasing plasma calcitonin gene-related peptide level, decreasing endothelin-1 level, and decreasing size of myocardial infarction (Zhang et al, 2004). Also, Bonin et al (2018) and Eitel et al (2020) stated that morphine is effective and safe in cases of STEMI. However, some authors raised the possibility of harmful opioid effects that may lead to high mortality (Yan et al, 2020). Morphine might reduce the effects of antiplatelet agents used in acute stage (Koh et al, 2019). Many strategies have been adopted to overcome this undesirable effect that occurs through interaction between morphine and P2Y12 receptor inhibitors. These include using crushed ticagrelor tablets or morphine replacement with administration of short-acting alfentanil. Otherwise, it is recommended to be co-administered with an antiplatelet agent after clinical evaluation of the patient (Moore et al, 2021).
Pethidine
Pethidine is another analgesic that can be used for AMI. It is a synthetic opioid known as meperidine. Its dose of 75–100 mg roughly corresponds to about 10 mg of morphine; and its analgesic effect becomes obvious within 15 minutes of intramuscular injection (Yan et al, 2020).
4- Nitroglycerin
Nitroglycerin or glyceryl trinitrate (GN) since its discovery over 150 years ago has become the most common drug used in the treatment of angina and AMI (Ferreira and Mochly-Rosen, 2012). Its effect occurs by promoting vasodilation and thus increasing coronary blood flow (Abrams, 1985). GN is effective in restoring oxygenation of the ischemic part of myocardium. However, there is a tolerance with sustained administration resulting in pro-oxidant effects, with increase of sensitivity to vasoconstrictors (Kosugi et al, 2011). It could be administered as sublingual tablets (0.4 mg NG). It might be used to determine whether ST-section elevation is due to a spasm during preparation for reperfusion therapy (Griffin et al, 2013).
5- Platelet P2Y12 receptor antagonists
Platelet P2Y12 receptor plays the crucial role for platelets’ functions including hemostasis and thrombosis. It represents chemoreceptor for the adenosine diphosphate (ADP) (Cattaneo, 2015; Mechanic et al, 2021). Platelet P2Y12 receptor antagonists are used currently for all cases of STSMI. The drugs called antiplatelet agents recommended in this context include prasugrel, clopidogrel and ticagrelor; the first and second are irreversible inhibitors of the receptors while the third one is a reversible inhibitor (Kushner et al, 2009; Siller-Matula et al, 2011). The clopidogrel is the most widely P2Y12 receptor antagonist used in clinical sitting (Cattaneo, 2015). A loading dose of 600 mg clopidogrel is recommended before or during percutaneous coronary intervention (PCI) (Siller-Matula et al, 2011). Other newer drugs, including prasugrel and ticagrelor, have been shown to be more effective at preventing major heart events than those with clopidogrel (Cattaneo, 2015).
6- Anticoagulants
Antithrombotic therapy should be given to all patients with STEMI unless contraindicated. Unfractionated heparin (UFH) is traditionally used 60 U/kg as one bolus with a maximum of 4,000 U, followed by an infusion of 12 U/kg/h with a maximum of 1,000 U/h. This aims to achieve partial thromboplastin time (PTT) value of 45 to 65 seconds. Low molecular-weight heparin (LMWH) is considered an alternative to UFH; however, it is preferred in cases undergoing fibrinolysis. It has advantages over UFH including more bioavailability, more fixed dosing, increased thrombin inhibition, decreased heparin-induced thrombocytopenia and more cost effective as no need for serial monitoring of Activated Partial Thromboplastin Time (aPTT). Other anticoagulants are mostly targeting the prevention of recurrence rather than use in initial phase of disease. They include direct thrombin inhibitor dabigatran and anti-Xa therapies (rivaroxaban, apixaban and otamixaban) (Onwordi, 2018).
Reperfusion therapy
Reperfusion therapy is a medical management aiming to restore the coronary blood flow after AMI either through the blocked vessel or passing around it. It includes medication and surgery. Medications include fibrinolytics; while surgery include minimal invasive procedures called PCI and other more invasive surgery comprising coronary bypass around the blocked part of the vessel (McCoy et al, 2013).
Reperfusion therapy should be reinstituted as soon as possible. Proper timing of reperfusion interference could reduce myocardial damage and thus the size of infarction and minimize the morbidity and mortality (Bagai et al, 2014). Perfusion could be performed via fibrinolysis or PCI. The PCI is preferred if facilities of angiography and PCI are available within 90 minutes of medical contact; they might be done immediately. Otherwise, fibrinolysis could be done. However, the last therapeutics of fibrinolysis should not be prescribed for patients of non-STEMI (Keeley et al, 2003). In this case, antifibrinolytics should be administered unless contraindicated within the first 30 minutes of medical contact. However, if they are contraindicated, arrangement for doing PCI could be taken. Fibrinolytics include alteplase, streptokinase, reteplase, and tenecteplase. Such medications should be used in conjunction with heparin therapy (Griffin et al, 2013). In all cases, antiplatelet therapy as well as parenteral anticoagulants are recommended. Prior to hospital discharge, patients with AMI may be given aspirin, beta-blockers, high-dose statins and/or an ACE inhibitor (Mechanic et al, 2021).
Prognosis and Prevention
Acute myocardial infarction still carries high risk of death. About 5-10% of patients undergoing AMI die within the first year after the incidence of the events. Moreover, about 50% are needed to be re-hospitalized in the same year. The overall outcome depends on many factors including degree of the myocardial infarction, timing of medical intervention and management as well as presence of precipitating risk factors. The complications of AMI include early development of cardiac arrythmias and fibrillation that may cause congestive heart failure, papillary muscle damage with development of newly-emerged atrioventricular regurgitation and late complications represented by myocardial aneurism and interventricular septal rupture (Mechanic et al, 2021).
The commonly adopted strategy for primary prevention of AMI relies on two main components. The first component is conducted by healthcare systems and includes a healthy environment and appropriate lifestyles. The second personal factor is to be taken from the individuals themselves by staying away from potential risk factors including abstaining from smoking and excessive drinking, avoiding obesity, adopting a new good dietary pattern and treating underlying causes such as diabetes and hypertension (Perna, 2020).
The MI is a great health challenge worldwide in both developed and developing countries. Identification of risk factors and therefore their avoidance as much as possible is the cornerstone of prevention of myocardial infarction and also helps in the treatment of patients. Prompt and proper diagnosis and treatment are essential to save patients or at least minimize complications. The diagnosis of myocardial infarction is based primarily on evaluations of clinical features, typical abnormalities in ST-segment and T wave of ECG findings and rise in cardiac enzymes or biomarkers such as plasma troponin. At the same time, the key to treatment is reperfusion of the myocardium and restoration of coronary blood flow.
None.
None.
All authors share in all steps of the article. All figures in the paper were drawn by the fifth author “AAH”.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti
Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation. “The peer review process was efficient and constructive, and the editorial office provided excellent communication and support throughout. The journal ensures scientific rigor and high editorial standards, while also offering a smooth and timely publication process. We sincerely appreciate the work of the editorial team in facilitating the dissemination of innovative approaches such as the Bonori Method.” Best regards, Dr. Matteo Bonori.

I recommend without hesitation submitting relevant papers on medical decision making to the International Journal of Clinical Case Reports and Reviews. I am very grateful to the editorial staff. Maria Emerson was a pleasure to communicate with. The time from submission to publication was an extremely short 3 weeks. The editorial staff submitted the paper to three reviewers. Two of the reviewers commented positively on the value of publishing the paper. The editorial staff quickly recognized the third reviewer’s comments as an unjust attempt to reject the paper. I revised the paper as recommended by the first two reviewers.

Dear Maria Emerson, Editorial Coordinator, Journal of Clinical Research and Reports. Thank you for publishing our case report: "Clinical Case of Effective Fetal Stem Cells Treatment in a Patient with Autism Spectrum Disorder" within the "Journal of Clinical Research and Reports" being submitted by the team of EmCell doctors from Kyiv, Ukraine. We much appreciate a professional and transparent peer-review process from Auctores. All research Doctors are so grateful to your Editorial Office and Auctores Publishing support! I amiably wish our article publication maintained a top quality of your International Scientific Journal. My best wishes for a prosperity of the Journal of Clinical Research and Reports. Hope our scientific relationship and cooperation will remain long lasting. Thank you very much indeed. Kind regards, Dr. Andriy Sinelnyk Cell Therapy Center EmCell

Dear Editorial Team, Clinical Cardiology and Cardiovascular Interventions. It was truly a rewarding experience to work with the journal “Clinical Cardiology and Cardiovascular Interventions”. The peer review process was insightful and encouraging, helping us refine our work to a higher standard. The editorial office offered exceptional support with prompt and thoughtful communication. I highly value the journal’s role in promoting scientific advancement and am honored to be part of it. Best regards, Meng-Jou Lee, MD, Department of Anesthesiology, National Taiwan University Hospital.
