AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2690-8808/149
Department of Medical Gastroenterology, PGIMS, Rohtak & SHKM, Nalhar, Mewat &ADGHS, NVHCP, Panchkula, Haryana, India.
*Corresponding Author: Parveen Malhotra. Department of Medical Gastroenterology, PGIMS, Rohtak & SHKM, Nalhar, Mewat &ADGHS, NVHCP, Panchkula, Haryana, India.
Citation: Parveen Malhotra, Usha Gupta, Yogesh Sanwariya, Mahima Vohra, Sugam, Shobhit Singh. (2023). Missing Links in History Leads to Diagnostic Dilemma. J, Clinical Case Reports and Studies, 4(3); DOI:10.31579/2690-8808/149.
Copyright: © 2023 Parveen Malhotra, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 27 December 2022 | Accepted: 20 January 2023 | Published: 02 March 2023
Keywords: costal cartilage disruption; diaphragmatic hernia; trauma; thoracoabdominal hernia
Costal Cartilage disruption after forceful coughing in obese males is an uncommon occurrence. Rarely it is associated with diaphragmatic disruptions leading to herniation of the abdominal contents into the chest. A successful outcome requires correcting both elements, namely, repairing the diaphragmatic defect along with the reduction of hernia and repairing the costal cartilage fracture. In this manuscript, we present a case where the diaphragmatic hernia was repaired, but the costal cartilage disruption was missed resulting in a reoccurrence of the diaphragmatic hernia.
Good history taking is an essential part of a comprehensive assessment of everyone including older adult [1]. The advancement in technology is continually redefining the practice of medicine, with sophisticated diagnostic machines, investigative procedures, and medical tests now widely available for medical diagnosis. Indeed, new discoveries, devices, and the internet have positively influenced the way physicians diagnose, treat, and palliate diseases. However, unlike in many high-income settings, where advancements in medical technology have, in most cases, been complementary to understanding disease pathogenesis and acquisition of core clinical skills, emerging evidence from many low- and middle-income countries, point to the contrary [2,3]. There are widespread concerns about doctors’ declining attitude in bedside skills and clinical aptitude [4]. While it is a requisite that medical students and doctors-in-training must demonstrate competence in history-taking and physical examination, there are reports that doctors fail to maintain and improve on these skills over their professional practice owing to over-reliance on results of medical tests [4]. In developing countries like India due to resource-constrained settings, where majority can hardly afford simple medical tests, the essence of detailed history taking and physical examination cannot be overemphasized.
A thirty eight year old male, non smoker, non alcoholic, government servant, married and was having no previous history of Diabetes mellitus, Hypertension, Thyroid disorder or Koch's presented with one year history of Polyuria which was characteristically occurring in morning hours after
waking up and use to settle by afternoon. There was no history of burning in urine, hesitancy, hematuria, post maturation dribbling, fever, weight loss. His clinical examination including general and systemic including Chest, Respiratory, Cardiovascular, Central Nervous System were essentially normal. He had been seen by multiple specialists like Urologist, Endocrinologist and General Physicians but for no relief. All his investigations like Complete Haemogram, Liver & Renal function test, Thyroid & Lipid profile, Viral screen, Urine complete & Culture, Chest X-ray, Ultrasonogram abdomen, Computed tomography scan of abdomen including pelvis were essentially normal. There was no leading point except increased amount of urine that too only in morning. Then again it decided to start fresh with the case and again history was recorded and for the first time patient shared that he has started consuming around three liters of water after waking up in the morning for last one year and after that his increased urine passage problem in the morning started. He has started this habit of increased water intake in morning on advice of his friends, so as to improve digestion and avoid gastritis problem in future. On asking why he has not shared it before to all the doctors he consulted, then he replied it being a routine phenomenon followed by many and thus never attributed any importance to same. The patient was adviced to restrict his morning intake from three liters to half liter and this solved all the problem. Thus a patient who has been seen by many specialists and was over investigated and remained diagnostic dilemma was solved in single sitting with the patient and repeat recording of history.
A Seventy eight year old male, smoker, non alcoholic and not a known case of Diabetes mellitus, Hypertension, Thyroid disorder or Koch's presented with three days history of dysphagia and for last one day he was not able to swallow anything. He was being treated by local private practitioner on lines of dyspepsia but for no relief. The family members and treating doctor thought then thought it may be transfer dysphagia due to nerve weakness supplying throat and this weakness may have developed slowly and now must have aggravated and thus patient appreciated the same at this stage. But patient was adamant that his this complaint of inability to eat has developed only for last three days. Thus he persisted to be shown to some specialist. Thus patient was taken up from village to our centre. His clinical examination including general and systemic including Chest, Respiratory, Cardiovascular, Central Nervous System were essentially normal. The history was recorded point wise and in detail and patient at that point of time told that he ate Indian Blackberries before developing complaint of dysphagia and he admitted that same thing he has told to his family members and local private practitioner who treated him initially but they attributed no importance of it for causing dysphagia and neglected it. But they forgot that patient may have unknowingly swallowed the whole Indian blackberry with seeds which is very hard and can easily get stucked up in esophagus. Thus keeping that in mind, patient was subjected to upper gastrointestinal endoscopy which as expected showed stucked up seed of Indian blackberry in mid-esophagus which was removed by foreign body basket.
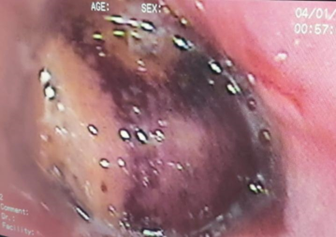
Figure 1: Endoscopy Showing Stucked up Indian Blackberry in Esophagus

Figure 2: Showing Indian Blackberry Removed By Foreign Body Forceps
The patient got immediate relief and started eating well and was discharged after observation for twenty four hours. The patient had no complaints after discharge. Thus it clearly emphasizes the need of believing the complaints and version of patient. In this case also patient persisted to be shown to specialist and hinted about foreign boy ingestion which was neglected by family members and local practitioner who initially treated the patient.
A forty two year old female, non smoker, non alcoholic, house wife, married and having two children born by normal delivery in government hospital. She was suffering from diabetes mellitus and was being treated with Glimiperide and Metformin combination. She had no history of Hypertension, Thyroid disorder , Dyslipidemia or Koch's. She presented to us with three months history of increased frequency of stools, urge to pass stool after every meal but there was no history of blood or pus with stools, nocturnal frequency, dyspepsia, weight loss, fever or significant pain abdomen. The clinical examination including general and systemic including Chest, Respiratory, Cardiovascular, Central Nervous System were essentially normal. She was on regular follow up of Endocrinologist for control of Diabetes Mellitus. All her investigations like Complete Haemogram, Liver & Renal function test, Thyroid & Lipid profile, Viral screen, Urine complete & Culture, Chest X-ray, Ultrasonogram abdomen, Computed tomography scan of abdomen including pelvis, Serum IgAttg antibody for wheat allergy were essentially normal. The patient was treated on lines of Irritable bowel syndrome in view of history of diabetes mellitus and clinical presentation but even after three weeks of treatment there was improvement in symptoms. The dose of drugs being used for I.B.S. were increased and some new drugs were added but even this did not work and symptoms persisted. It was very surprising that almost all patients of I.B.S respond at least partially to these drugs but this patient despite being on full dose of I.B.S. drugs with diabetes mellitus under control and strict dietary advices like avoiding of milk, juices, high sugar, oily & spicy diet, no improvement was occurring. Hence, it was decided to restart from starting and again all history, dietary intake and drug intake was recorded and now patient revealed that three months back, a new oral hypoglycemic drug Voglibose and Metformin combination was added to previous drugs and after that symptoms of I.B.S started. The patient was totally correct as this drug is known to cause I.B.S symptoms and as soon as this drug was stopped, patient got absolute relief. Thus there was missing of history of this drug intake both on part of patient as well doctor, thus once its intake was noticed, despite stopping of all I.B.S medication, all symptoms settled. The fact is it was not I.B.S but side effect of oral hypoglycemic drug.
It is always said to make correct diagnosis, the journey transverse the path of History, clinical features and investigations. The wise physician on basis of good history makes probable differential diagnosis and to confirm the same gets limited specific tests. An ideal doctor is who can diagnose patient correctly with limited tests and successfully treat patient with minimal drugs, so as to save from adverse reactions and decrease financial burden on society. For this proper knowledge and its application in right direction is mandatory, thus it reemphasizes the need of detailed history with recording of every small detail because that can prove to be turning point in correct diagnosis and treatment of patient.
The authors declare that they have no conflict of interests.
The authors declare that no financial support was taken for above study.