AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2768-2757/082
Department of Surgery ward 02, Jinnah Postgraduates Medical Centre Karachi.
*Corresponding Author: Anas Ahmed, Department of Surgery ward 02, Jinnah Postgraduates Medical Centre Karachi.
Citation: Anas Ahmed, Dileep Kumar, Shamim Qureshi, (2023), Jejuno-Jejunal Intussusception in An Adult-An Unusual Presentation of Malignant Melanoma: A Case Report. Journal of Clinical Surgery and Research, 4(4); DOI:10.31579/2768-2757/082
Copyright: © 2023, Anas Ahmed. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 29 May 2023 | Accepted: 06 June 2023 | Published: 13 June 2023
Keywords: jejuno-jejunal; intestinal obstruction; intussusception; malignant melanoma
Background: Small bowel intussusception is common presentation in children and rare in adults but malignant melanoma as primary cause is once in a blue moon event. It accounts for 1% of all bowel obstructions. Jejuno-Jejunal intussusception is a rare mode of metastatic malignant melanoma presentation. It may be metastatic and rarely primary cause of this type of presentation. In literature no such case s reported from our country before and perhaps seventh case of malignant melanoma as primary cause of jejuno-jejunal intussusception in literature.
Case Presentation: Here we report a case of a 40 years old male who presented to us with features of intestinal obstruction. On exploration, Jejuno-Jejunal intussusception was found secondary to some mass in jejunum. Resection anastomosis of Jejunum was performed. Histopathological examination of mass revealed metastatic malignant melanoma. On further work up, CT scan abdomen showed multiple enlarged mesenteric lymph nodes and few enlarged bilateral inguinal lymph nodes. Patient post-operative recovery was uneventful and discharged.
Conclusion: One should suspect metastatic melanoma as a lead point in cases of jejuno-jejunal intussusception in adults presenting with intestinal obstruction.
Intussusception is invagination of one portion of gut into an immediately adjacent segment. More common in children than adult. In adult population intussusception account for 1% of total cases and diagnosis is challenging because of nonspecific symptoms i.e., abdominal pain, vomiting and constipation. Although the gastrointestinal (GI) tract is an uncommon site for metastasis, melanoma is one of the most common tumours to metastasize to the GI tract. Only 2 to 4% of patients with melanoma will be diagnosed with GI metastases during course of disease [1, 2].
It is unusual for a cutaneous melanoma to metastasise to the intestine, but it is even rarer for that metastatic nodule to act as a lead point and result in intussusception. Numerous cases of ileo-ileal intussusception have been reported in the English medical literature, but only six cases of jejuno-jejunal intussusception due to malignant melanoma are documented. (3) In literature not a single case was reported of this type from our country. So, patients with such metastatic lesions can present with features of intestinal obstruction and that too with intussusception or bleeding. One should keep this thing in mind while treating jejuno-jejunal intussusception. The rarity of this presentation in adults is the prime reason for reporting this case.
A 40 years old male presented in Emergency department with severe Central abdominal pain and vomiting since 06 days, History of weight loss was present. He was operated for some scrotal skin surgery in 2014 but no documentation was available. On Examination Patient was vitally stable, Conscious well oriented, looking pale. Abdomen was not distended. Scar mark was seen on scrotum. 4x11cm enlarged left inguinal lymph node. Haematological labs were unremarkable, X-RAY Abdomen Erect was Unremarkable. Ultra-sound Abdomen showed large segment of Jejuno-Jejunal intussusception approximately measuring 8.0cm noted in left lumbar region. Few enlarged adjacent mesenteric lymph nodes are also seen. Active resuscitation measures including Nasogastric tube, Foley’s catheter and Intravenous fluid administered. Diagnostic laparoscopy was done which showed jejuno-jejunal intussusception which converted operation to mini–Exploratory Laparotomy. Resection anastomosis of Jejunum was performed and mass was sent for biopsy.
Histopathology report revealed Tumor of about 4.5x3cm size and Malignant Melanoma TNM Stage: T3 NO MO, Single focality, Melan-A positive, HMB-45 positive, S100 positive, CKAE1/AE3 positive. Lymphovascular invasion was not identified.
CT Scan Abdomen and Pelvis shows Multiple enlarged mesenteric lymph node. Largest one on left side measures approximately 2.7x2.2cm. Few enlarged bilateral inguinal lymph node Largest one on left side measures approximately 6.2x4.2Cm (Figure.3)

Figure 1
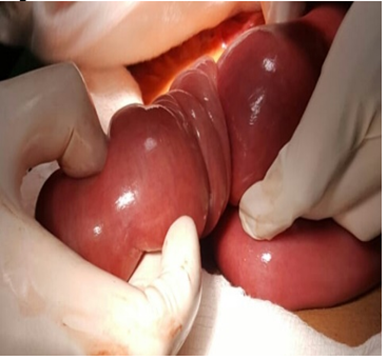
Figure 2

Figure 3
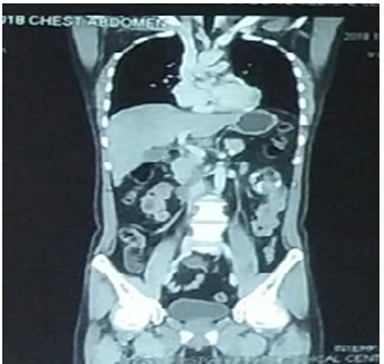
Figure 4
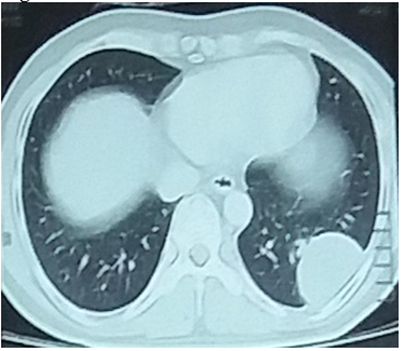
Figure 5
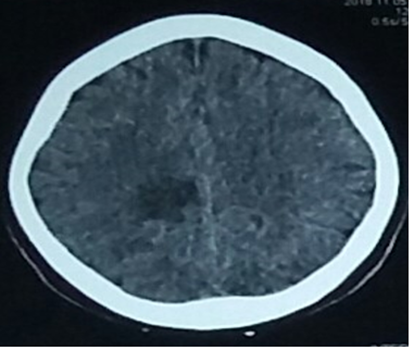
Figure 6
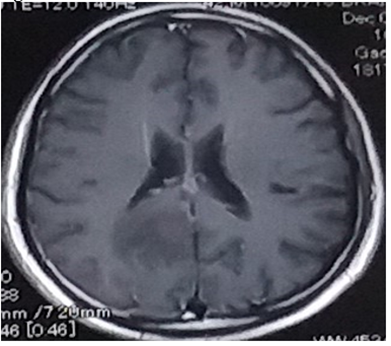
Figure 7
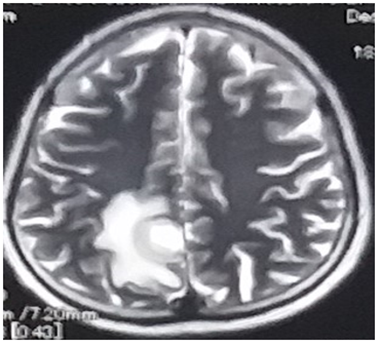
Figure 8
CT Scan chest shows few soft tissue density nodules identified in lungs (Fig.5). Largest one measures 4.2cm x 3.2cm in the left lower lobe in subpleural in location abutting chest wall with no bony destruction. Other two lesions seen in upper lobe. CT Spine shows well defined lucent lesion seen in L3 and L4 vertebral bodies.
CT scan Brain and MRI Brain with Contrast shows metastatic lesions in right high parital lobe along with parasagittal location (Figure.6,7,8)
Small bowel intussusception presents commonly in children. Though being idiopathic in aetiology, it is a rare entity in adults accounting 1% of population and is usually neoplastic. The Gastro-Intestinal tract (GI) is the third most common site for distant metastasis where small intestine is most commonly affected. Gastro-intestinal metastases have been observed in 5-6% patients of malignant melanoma, whereas 60% of them remain undiagnosed during their life time. Malignant melanoma is highly aggressive and has high metastatic potential associated with a worse prognosis [4-6].
Though malignant melanoma is the most common cause of the extra-abdominal source of intestinal metastasis, it is rare to find them presenting as jejuno-jejunal intussusception [7]. To date in the English medical literature, only six cases of jejuno-jejunal intussusception with melanoma as the lead point have been documented [3].
Rare reports of primary gastrointestinal melanoma have been documented. It occurs due to the malignant transformation of locally migrated primordial skin megaloblastic cells during foetal development [8]. Most cases of gastrointestinal involvement in melanoma stem from metastasis from primary cutaneous melanoma. Gastrointestinal metastasis is very rare and is seen in three to five per cent of cases and is classified as stage four terminal disease with an average life span of two months to 15 years following diagnosis [7].
Most melanoma patients present early with the sudden appearance of a growing hyper pigmented patch on their skin. The delayed presentation is seen mainly in developing countries because of poverty, lack of medical knowledge, neglect, and lack of proper management. The presentation of a patient with a primary gastrointestinal melanoma is usually late, not occurring until he or she develops features of obstruction or may present with non-specific symptoms like vomiting, nausea, abdominal pain, and bleeding [7].
Excision biopsy is the preferred method of investigation to diagnose cutaneous melanoma. In our case, the patient initially presented with features of intestinal obstruction, which were investigated by ultrasonography and CECT scan. So, it is very rare to present like this.
A study by Karmiris et al. showed that CT scan have a sensitivity of 70 per cent in diagnosing such lesions [9]
Treatment in metastatic melanotic intussusceptions with obstruction is palliative and involves resection and anastomosis of the involved segment of the gut. It relieves obstruction and also helps in the control of blood loss. Reduction should not be attempted if malignancy is suspected [10].
To conclude this, we can say that despite being a rarer entity, one should suspect metastatic melanoma as a lead point in cases of jejuno-jejunal intussusception in patients presenting with intestinal obstruction.
The authors declared no conflict of interest.
AA: Concept, design, definition and intellectual content
DK: Data acquisition, Literature search, data analysis, manuscript preparation and editing.
SQ: Design, definition and manuscript preparation