AUCTORES
Globalize your Research
Research article | DOI: https://doi.org/DOI:10.31579/2642-973X/051
1 Department of Rehabilitation Science, School of Public Health and Health Professions, State University of New York at Buffalo, Buffalo, NY, USA.
2 Jacob's School of Medicine, State University of New York at Buffalo, Buffalo, NY, USA.
*Corresponding Author: Ghazala T. Saleem, Department of Rehabilitation Science, School of Public Health and Health Professions, State University of New York at Buffalo, Buffalo, NY, USA.
Citation: Wenjie Ji, Madeleine Champagne-Shafer, Jung An, and Ghazala T. Saleem. (2023), Identifying Objective and Field Expedient Markers in Intimate Partner Violence-Related Brain Injury: A Cross-Sectional Study Protocol. J. Brain and Neurological Disorders. 6(2): DOI:10.31579/2642-973X/051
Copyright: © 2023 Ghazala T. Saleem. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 28 January 2023 | Accepted: 18 February 2023 | Published: 28 February 2023
Keywords: intimate partner violence; brain injuries; autonomic nervous system; vestibular function tests
Background: Brain injury (BI) is a serious consequence of intimate partner violence (IPV). However, evidence-based assessments are lacking to properly identify BI sequelae in IPV survivors. This pilot study focuses on identifying an objective marker of BI and physiological alteration among female IPV survivors. Materials and Methods: This cross-sectional study will compare differences in the effects of BI between two groups of female IPV survivors. A total of 52 survivors will be assigned to either a physically abused group or to an emotionally/psychologically abused group. The primary outcomes will include: 1) BI signs examined by the Buffalo Concussion Physical Examination; 2) the autonomic function assessed by the heart rate variability during an isometric handgrip test, and 3) the vestibular function evaluated through King-Devick devices. Expected Results: Female survivors with physical abuse will demonstrate more BI signs, and autonomic and vestibular dysfunctions compared to those with emotional/psychological abuse. Conclusions: The results of this trial will support the establishment of reliable objective evaluations of BI and physiological function in female survivors of IPV.
Intimate partner violence (IPV) is abuse conducted by a former or current intimate partner. IPV may cause severe physical injury, mental health concerns and may even lead to death [1]. Females are more likely to be a victim of IPV than males [2]. Behaviors regarding IPV can be divided into physical and non-physical violence (i.e., sexual violence, stalking, and psychological aggression). Victims of physical IPV are pushed, punched, kicked, and hit on the head, face and jaw, and strangled [3-5]; some of these mechanisms may place the survivors of physical violence at a higher risk of brain injury (BI) than those with non-physical violence [5, 6]. BI from IPV is referred to as “IPV-related BI”.
Previous research focusing on IPV-related BI mostly used subjective assessments (e.g., self-report) to identify BI in the IPV population [4, 7]. Recall bias exist with self-reports and some of the subjective measures may scale-up or diminish the problems based on socio-ecological factors [8]. Therefore, objective measures such as a BI physical examination are needed for accurate diagnosis and prognosis of BI as well as targeted treatment in this population [9]. The Buffalo Concussion Physical Examination (BCPE) is known to reliably differentiate athletes with acute sports-related BI from their healthy controls [10]. Thus, it will be used as the objective physical examination to identify IPV-related BI in survivors of IPV.
Assessments of physiological functions, such as cardiac autonomic and vestibular functions may serve as supplementary evaluations to the physical examination, which may identify sequalae resulted from IPV-related BI [11-17]. Cardiovascular control for homeostasis is regulated by the autonomic nervous system (ANS), which is known to be “autonomic coupling” [18-20]. The central control for the ANS is located in the brain [21, 22], thus, injury to the brain has been linked to “autonomic uncoupling” [13, 23]. Female survivors of IPV have been shown to have altered glucocorticoids (cortisol) and catecholamines concentration [24] as a consequence of potential ANS dysfunction. However, it is unknown whether this ANS alteration is linked to BI and if females with physical abuse demonstrate more autonomic impairments compared to their non-physical IPV cohort after controlling for the confounder of psychological distress [5, 25-28]. Therefore, this study will use heart rate variability (HRV), which is a commonly used marker reflecting ANS regulation [18, 29, 30] to investigate ANS function and its relationship to BI in this population. In addition to ANS deficits, impairments in vestibular function, including oculomotor and balance are often reported after traumatic BI [31-33]. Yet, to date, vestibular function has not been systematically evaluated in IPV survivors reporting physical injuries. Several oculomotor and balance assessments using the King-Devick (K-D) device have reliably evaluated vestibular function in other populations with mild traumatic BI [31-35].
This pilot study aims to 1) examine if survivors with physical IPV demonstrate more BI signs on the Buffalo Concussion Physical Exam (BCPE) compared to non-physical IPV cohort; and 2) examine if female survivors with physical abuse demonstrate worse cardiac autonomic and vestibular functions compared to those with non-physical abuse after adjusting for psychological distress.
Study Design
This cross-sectional study will assess differences in physical examination and physiological/vestibular outcomes in physically-abused (experimental) and non-physically abused (control) group of IPV survivors. The entire study visit will last about 1.5 hours. This study will be approved by the University Institutional Review Board, and all participants will provide informed consent.
Participants
This study will recruit a statistically-valid sample of 52 female survivors of IPV (26 per group). Participants will be recruited from community-based shelters or non-shelter settings around Western New York. The study team will screen survivors’ eligibility based on the following inclusion/exclusion criteria. Physically-abused cohort inclusion criteria are: 1) 18-60 years old [4, 36]; 2) reporting physical injury within the past 2 years from a current or former intimate partner [7]; and 3) proficient in English. Non-physically-abused cohort inclusion criteria are: 1) 18-60 years old [4, 36]; 2) reporting any abuse other than physical abuse within the past 2 years from a current or former intimate partner [7]; 3) not physically-injured for any reason within the past 5 years [37]; 4) no known history of BI within the past 5 years [37]; and 5) proficient in English. Exclusion criteria for both groups are: 1) pregnancy; 2) physical injury resulting in loss of consciousness > 24 hours or post-traumatic amnesia > 7 days [38] ; 3) focal neurological deficit(s) on physical exam [38]; 4) orthopedic injury producing significant balance deficits [38]. Participants’ attribution is shown in Figure. 1.

Figure 1: Flowchart of participants’ attribution to the physical- and non- physical-abuse groups
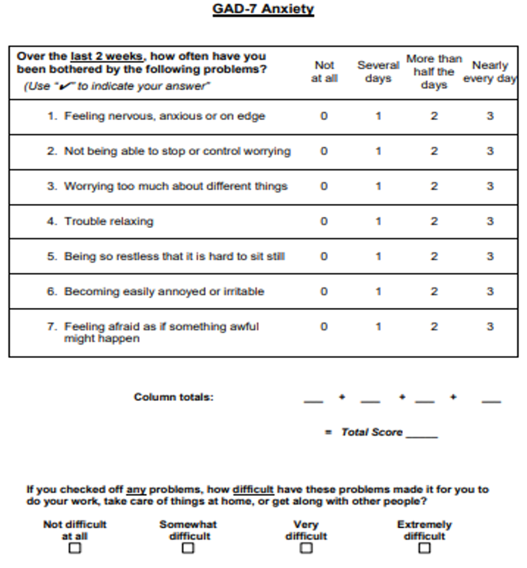
Figure 2: General Anxiety Disorder-7 Questionnaire [39]
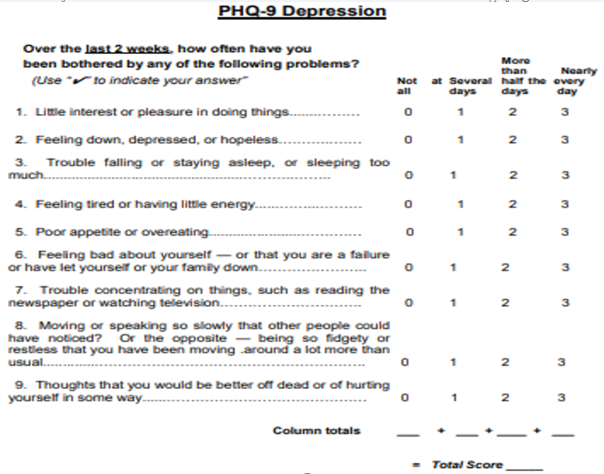
Figure 3: Patient Health Questionnaire-9 [40, 41]
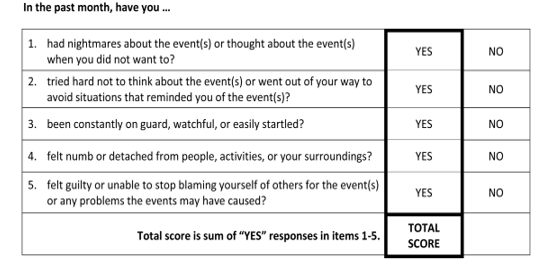
Figure 4: Example of The Primary Care PTSD Screen for Diagnostic and Statistical Manual of Mental Disorders-5 [42-44]
Outcome measures include both subjective and objective assessments: General Anxiety Disorder-7 (GAD-7). The GAD-7 was developed as a screen for generalized anxiety disorder in primary care settings [39]. It is a seven-item self-report questionnaire, and the score ranges from 0 to 21 (Fig. 2). Participants will report on the frequency of experiencing each GAD-7 symptom (e.g., being on edge or feeling nervous). Response options are “not at all,” “several days,” “more than half the days,” and “nearly every day,” scored as 0, 1, 2, and 3, respectively. A cutoff point of 10 provides a sensitivity of 89% and a specificity of 82% for the clinical diagnosis of GAD [39]. GAD-7 is known to be particularly useful in assessing symptom severity of anxiety and monitoring change across time [45]. It is widely used in studies in IPV as a standard assessment for anxiety [46-48].
Patient Health Questionnaire-9 (PHQ-9). The PHQ-9 is a 9-item depression module from the full Patient Health Questionnaire [49]. It includes questions on depression-related symptoms, such as little interest or pleasure in doing things, or feeling down. Response options are “not at all,” “several days,” “more than half the days,” and “nearly every day,” scored as 0, 1, 2, and 3, respectively. The PHQ-9 score ranges from 0 to 27. Cutoff points of 5, 10, 15, and 20 represent the thresholds for mild, moderate, moderately severe, and severe depression, respectively [40]. A cutoff point of 10 is recommended for a single screening for major depression [41]. PHQ-9 is commonly used in studies in IPV as a standard assessment for depression [46, 48, 50].
PTSD. The Primary Care PTSD Screen for Diagnostic and Statistical Manual of Mental Disorders-5 will be used to identify female survivors with probable PTSD (Fig. 4). The measure begins with a single item that assesses past exposure to traumatic events. If subjects deny any exposures, the PTSD screen is completed with a score of 0. However, if subjects indicate a trauma history – experiencing a traumatic event over the course of their life – they need to provide responses to five additional yes/no questions about the effects of trauma on their functioning, roles, and routines over the past month [44]. Preliminary results from validation studies suggest that this screen is an accurate tool for assessing PTSD [43] and a cutoff point of 3 on the PTSD screen is optimally sensitive to females with probable PTSD [42, 43].
BCPE. The BCPE is a brief (5–7 min), pertinent physical examination protocol designed for the outpatient setting, assessing subsystems commonly affected after BI (e.g., cervical, balance, and oculomotor) [51]. It was initially designed to diagnose sports-related BI [51], and has been reported to have high sensitivity (82%) and specificity (90%) for identifying symptoms following sports-related BI [10].
HRV Assessment. Heart rate will be collected using the 3-lead electrocardiogram during the 5-minute baseline, and then during an isometric grip testing followed by a 5-minute recovery. For the isometric grip testing, participants will be asked to perform 3 maximum voluntary hand grips using their preferred hand. Then, a 30% of the maximum voluntary contraction will be calculated for each individual, and participants will be asked to maintain it for one minute [52, 53]. This maneuver is to activate cardiac sympathetic activity. Raw electrocardiogram waveforms will be processed to get time- and frequency-domain HRV through the Kubios HRV premium software [54], such as root mean square of successive standard deviation of R-R interval (RMSSD), high frequency (HF), and low frequency (LF) of HRV. RMSSD and HF of HRV are known to reflect changes in parasympathetic activities [55], while LF of HRV is suggested to indicate sympathetic tone [56].
K-D Eye Tracking and Balance Tests. The K-D Eye Tracking System is a quantitative tool to assess oculomotor function after BI. The K-D test involves reading aloud a series of single-digit numbers from left to right on 3 test cards. The sum of the 3 test card time scores will constitute the summary score for the entire test, the K-D time score. Numbers of errors made in reading the test cards will also be recorded. The K-D Balance System assesses three key balance stance metrics: double stance, right tandem stance and left tandem stance. An objective balance score will be automatically derived by detecting the individual’s movements using the device’s internal accelerometer. The intra-rater reliability is good to excellent for K-D Balance testing [57].
The BCPE outcomes will be compared between the groups using a chi-squared test. Multiple ANCOVAs will be used to examine the group differences RMSSD, HF, and LF of HRV during baseline, handgrip test, and recovery while adjusting for psychological distress. Independent t-tests will be utilized to examine the group differences on the K-D Eye Tracking score and the Balance score. We will not adjust for multiple comparisons as this is a pilot study. Significance will be set at p < 0>
We expect that female survivors with physical IPV will demonstrate more atypical findings on BCPE compared to their cohort with psychological/emotional IPV. Resting RMSSD and HF of HRV are expected to be lower in survivors with physical IPV compared to those with non-physical abuse indicating increased parasympathetic dysfunction in survivors of IPV with physical abuse. During hand grip testing, survivors with physical abuse are anticipated to demonstrate lower LF of HRV versus those with non-physical abuse suggesting higher anomalies in the function of sympathetic nervous system in survivors with physical abuse. A higher time score (indicating worse performance) and more errors are expected to be seen for the K-D Eye Tracking testing in female survivors with physical IPV compared to the control cohort with non-physical abuse Survivors with physical abuse are also expected to score higher (worse) on K-D Balance System compared to those with non-physical abuse.
The findings from this study could be useful in establishing rapid, objective tools to identify IPV-related BI in female survivors. It has been recognized, although not properly quantified, that IPV survivors are at a high risk of BI [4, 6, 58]. Symptoms such as anxiety may be heightened in survivors of IPV-related BI. Hence, assessments of BI from other populations should be validated in IPV survivors [7, 59]. Previous studies reporting BI in IPV survivors used subjective measures to assess the prevalence and severity of BI [4, 9, 58, 60]. However, this subjective evaluation may not accurately identify BI as reported symptoms can be misinterpreted for other disorders [4]. For example, in one study, the HELPS questionnaire, a subjective brain injury screen, only identified 40% BI in survivors of IPV who all reported IPV-related BI history on a clinical exam performed by a clinical examiner [61]. Therefore, objective examinations to precisely identify BIs in IPV survivors are critically needed. Focused, objective examinations not only assist clinical providers in accurately identifying BIs but will also help with improving IPV survivors’ well-being as well as access to healthcare [62-64]. This study will use a physical examination (i.e., BCPE) to objectively assess BI in female participants. Notably, mild traumatic BIs can be present without any abnormal signs revealed by imaging or neurological examination. Objective measures will be valuable in identifying dysfunction and guiding treatment and prognosis in survivors of IPV.
Furthermore, as noted before, survivors with physical IPV suffer from a cascade of symptoms that may ensue from physiological impairments [7], such as autonomic [24], and vestibular [65] dysfunctions. Previous research uses steroid levels as an indirect biomarker to identify autonomic dysfunction [24, 66]. However, techniques used for measuring steroid levels can be costly and time-consuming [67]. Therefore, it is critical to establish a valid and rapid assessment for autonomic function that can be easily applied in clinical settings. This study will apply HRV, a well-established methodology for autonomic evaluation in general population [55, 68, 69], to our samples of interest, female survivors of IPV. To this end, we will establish the feasibility of using HRV as a biomarker to assess autonomic function in this underserved population. Similarly, to this date, the deficits in vestibular function have not been evaluated objectively in survivors of IPV-related BI. Though a previous study found deficits associated with vestibular function in survivors of IPV, it lacked a control group [65]. The current study will use multiple balance/gait measures, which have been validated in other populations of BI [10, 57], to provide further evidence on vestibular dysfunction in survivors sustaining physical abuse compared to survivors sustaining psychological/emotional abuse (non-physical abuse cohort).
At the completion of this study, the need will remain to systematically evaluate objective markers of function in survivors of IPV-related BI. Though, through this study, an attempt would be made to identify reliable BI markers, several limitations exist. First, this study uses a convenience sample, and it is likely that our sample may not be representative of the larger IPV population. Future studies using random selection may provide more generalizable results. However, this study is crucial in establishing the groundwork for identifying objective markers of physiological and vestibular dysfunction in survivors of IPV-related BI. Second, the two study groups would not be randomized, and therefore, a possibility of selection bias exists. Future controlled studies with larger sample sizes focusing on BI diagnostic framework in IPV survivors may further characterize BI and its sequelae in this population. Third, this study will use various measures verified in other populations (e.g., sports-related BI) [10, 70]. However, we will not be able to provide cutoff points for these measures in female survivors of IPV due to a small sample size. Future researchers conducting trials with larger samples may identify cutoff points for assessments used in this study to provide a reference point for the diagnosis of BI and/or potential physiological impairments in the IPV population. Lastly, though we will make every attempt to use the same rater to administer assessments to both groups, a possibility exists that the rater may change. We will establish inter-rater reliability to reduce the rater bias [51, 71].
Here, we have provided a detailed description of a research protocol to identify probable BI and physiological markers in female survivors with IPV. We expect the review of this protocol may be useful to other researchers planning studies that investigate IPV-related BI. In addition, a detailed protocol of the physiological assessment trial is presented primarily to provide a reference for critically evaluating the results of this study. The results of this trial will support the establishment of objective evaluations of physiological functions in female survivors of IPV. Furthermore, identifying the utility of these physiological markers in the IPV population will set the stage toward selecting reliable methods when examining the effects of interventions for the IPV-related BI.