AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2692-9562/056
1 University of Health Sciences Gazi Yasargil Training and Research Hospital, Department of Otorhinolaryngology, Diyarbakır,21100 Turkey.
2 Dicle University, Department of Otorhinolaryngology, Diyarbakır,21100 Turkey.
*Corresponding Author: Serkan Dedeoğlu, University of Health Sciences Gazi Yasargil Training and Research Hospital, Department of Otorhinolaryngology, Diyarbakır,21100 Turkey.
Citation: Serkan Dedeoğlu, Muhammed Ayral, Serdar Ferit Toprak, (2023). Evaluation of Patients with Malignant otitis external Treated in Our Clinic. Journal of Clinical Otorhinolaryngology 5(2); DOI: 10.31579/2692-9562/056
Copyright: © 2023 Serkan Dedeoğlu, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Received: 02 January 2023 | Accepted: 11 January 2023 | Published: 29 January 2023
Keywords: malignant otitis externa; otalgia; pseudomonas aeruginosa; external otitis; necrotizing otitis externa
Background
Malignant otitis is a disease that occurs after an external ear canal infection and spreads towards the skull base. It is a complex condition to treat because it shows clinical differences between patients and different responses to treatment. Malignant otitis We investigated the epidemiology and treatment management of patients hospitalized with external diagnoses.
Material and Methods
This study was carried out between January 2014 and May 2020 in Dicle University ENT Clinic, which was treated and treated with malignancy. Otitis was designed as a retrospective study that analyzed 22 patients diagnosed with externa.
Results
All patients in the study had diabetes. He had diabetes mellitus. Pseudomonas aeruginosa was grown in the culture of 17 of the patients. Although otalgia was the most common symptom, discharge from the external ear canal and development of edema and obstruction were also observed. Two of our patients were hospitalized again as a result of recurrence.
Conclusion
Malignant disease in the practice of otolaryngology otitis It is a complex disease to treat due to the lack of a standard treatment protocol for externa. Therefore, early diagnosis and early initiation of treatment reduce the patients' hospital stay. Early diagnosis and treatment are the most critical factors in reducing mortality and morbidity.
Necrotizing otitis externa, also known as malignant otitis externa (MOE), is an aggressive disease of the external auditory canal that can spread to the mastoid region and skull base [1]. The first reported patient was fatal temporal bone osteomyelitis due to infection originating from the [2]. For the first time, Chandler et al . by ' Malignant otitis externa ' named it[3]. Severe otalgia and purulent discharge from the ear are common symptoms. Otoscopic examination, otitis While an appearance similar to an externa is formed, edema formation in the bone-cartilage region and granulation appearance are malignant. otitis in favor of the [4]. With temporal bone involvement, cranial nerve paralysis (most commonly facial nerve, then other cranial nerves IX, X, XII) may cause meningoencephalitis and brain abscess [5]. The most common pathogen is pseudomonas aeruginosa, but staphylococcus aureus, aspergillus, and candida are [6]. The incidence of MOE in the community is very low. Diabetes with MOE in older people and a low immune system is more common in Mellitus (DM) patients. Approximately 90% of MOE patients appear to have DM disease. The primary protocol in the treatment is antipseudomonal drugs. It was previously reported that mortality was close to 50%, and recurrence rates were very high in systemic medications. With the discovery of fluoroquinolones, the cure rate has increased to 90%. Generally, treatment can take 6-8 weeks [7]. In cases where some patients do not respond to this treatment, MOE due to [8]. Our study aimed to evaluate the clinical symptoms and response to therapy of MOE patients who applied to our clinic.
This study was carried out retrospectively according to the ethical standards stated in the 1964 Declaration of Helsinki, and publication ethics were followed. The Dicle University Faculty approved our study of the Medicine Ethics Committee. Ethics committee decision no. 311 dated 06.05.2021 was approved. This study was carried out between January 2014 and May 2020 in Dicle University ENT Clinic, which was treated and treated with malignancy. Otitis retrospective analysis of 22 patients diagnosed with externa was done by scanning the patient files and obtaining permission from the hospital management. The diagnosis of MOE was made by supporting the findings originating from the external ear canal towards the skull base with computed tomography (CT). The patients' demographics, co-morbidities, clinical symptoms, length of hospital stay, culture results, imaging methods, treatment, and surgical intervention were evaluated. Ceftriaxone 1g was started in our hospitalized patients, and other antibiotics were added according to the ear culture results. The patients were discharged after the decrease in otalgia and the cessation of ear discharge. Oral antibiotics and antibiotic ear drops were given to these patients. One week later, he was called for control. It was treated until the symptoms disappeared. These results were compared in the literature.
Of the 22 patients in the study, 14 were male, and eight were female. The mean age was 58 (34-82). All patients had DM. The number of patients whose right ear was affected was 13. The patient whose left ear was affected was 9. It was observed that two of our patients were treated for the hematological disease. Despite the topical treatment for otalgia and otorrhea, CT scans were performed because no improvement was observed in all patients. The diagnosis of MOE was left by combining clinical findings and examinations. Ear cultures were taken from all patients. Pseudomonas in 16 aeruginosa, staphylococcus in 2 aurei, and four did not reproduce. All patients had otalgia and ear discharge. Hearing loss was seen in 19 (86%) patients. Edema (91%) and granulation tissue (27%) occurred in the external ear canal. Facial paralysis was observed in one patient, and it was observed that he completely recovered after the treatment. In the anamnesis of two of our patients, we determined that they were treated for hematological diseases. Two of our patients are non-Hodgkin and received treatment for lymphoma. In Table I, we presented the clinical findings of the patients.
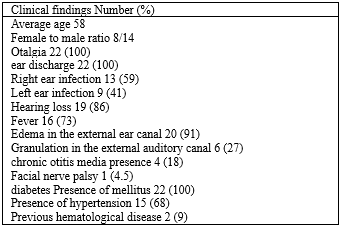
Table I. Clinical findings of MOE patients
Sedimentation rate (81%) and elevated C-reactive protein (68%) were present in many of our patients. The number of patients with Hba1c levels higher than ten was heightened. The mean length of hospital stay was 14 ±2.3. Systemic and topical antibiotic therapy was used in all patients. The mean duration of treatment was 12 ±3.6 weeks. In two of our patients, recurrence was observed one week after discharge, and after two weeks of treatment, complete recovery was achieved. Bone destruction was observed on CT of five patients. Laboratory, radiological, microbiological, and treatment conditions of MOE patients are shown in Table II

Table II. Laboratory , radiological, microbiological, treatment status information of MOE patients
MOE is a complicated disease to treat. Its treatment may be long-term, and it is necessary to follow this treatment closely. Undiagnosed or under-treated MOE may spread to the skull base, resulting in meningitis, lateral sinus thrombosis, or jugular vein may cause significant complications such as [9]. The most common clinical manifestation of many cases is ear pain. This pain may also be associated with temporal and occipital headaches. Edema, granulation formation, and discharge in the external ear canal are seen in all MOE cases [10]. Ear pain was observed in all of our patients in our study. Many of our patients present edema, granulation tissue, and discharge in the external ear canal. There is no difference between the right ear and the left ear in terms of MOE formation. There is no relationship between [11]. Our study observed that facial paralysis developed in one of our patients and wholly recovered after treatment.
In many studies in the literature, it is more common for patients with MOE to be elderly, have DM, chronic renal failure, and immunodeficiency diseases [12]. Twelve of our patients had high Hba1c levels and had uncontrolled DM, which is consistent with our literature search. MOE development in diabetic patients is related to [7]. Fifteen of our patients had hypertension (HT) with DM, and two patients had non-Hodgkin's disease. We saw that he had been treated for lymphoma.
We found that in 18 of our patients, the ESR rate was 40 mm/hr higher. We determined that clinical symptoms decreased as the ESR rate returned to normal. Thus, we thought that the ESR rate could be a parameter we could use to respond to treatment. Studies in the literature showed a relationship between ESR rate and regression in clinical symptoms [13]. Likewise, we found that the CRP value was above 10 mg/L in 15 patients. We thought that the decrease in CRP could be used to evaluate the response to MOE treatment. As the symptoms in our patients decreased, CRP decreased to normal levels. When CRP is considered together with clinical and radiological findings, it may show a response to treatment [14].
P.aeruginosa was the most common pathogen in our study with 16 patients. In many publications, it is stated that [15]. Staphylococcus in two patients' aureus and the other four patients showed no growth in the culture. CT scan was performed on all our patients. Bone destruction was observed on CT of five patients. One of our patients had facial nerve palsy and wholly recovered after treatment. Studies have shown that facial nerve palsy does not affect the [16]. Systemic antibiotic therapy with ciprofloxacin or ceftazidime and gentamicin, or Pseudomonas aeruginosa effective semisynthetic penicillin and aminoglycoside combination is recommended until the disease is brought under control [11]. Hyperbaric oxygen therapy can be an adjunctive method in patients resistant to antibiotic therapy [17]. Systemic and topical antibiotic therapy was started in all our patients. Regular ear lavage and treatment for diabetes control were provided. Drops with ciprofloxacin were used in topical treatment. Ciprofloxacin was used in systemic therapy. Oral ciprofloxacin was given after discharge. The mean duration of treatment ±was found to be 12 3.6 weeks. We had two patients with recurrence in the first week after release, and they were hospitalized again, and systemic antibiotic therapy was started. No reproduction was observed afterward.
MOE remains a complex disease to manage due to the lack of a standardized treatment protocol. In our study, Severe otalgia, edema, otorrhea in the external auditory canal, and facial nerve palsy were seen in MOE patients. They were primarily elderly patients, and all patients had diabetes and were immunocompromised. When MOE is diagnosed, systemic antibiotics are preferred for treatment. CT and magnetic resonance (MR) has an essential role in the diagnosis and follow-up of patients with MOE . has its place. CT scans may not reveal soft tissue changes early in MOE. If clinical suspicion of MOE persists, MRI is required. To correctly manage and eradicate MOE, clinicians should evaluate clinical symptoms and signs and assess radiological imaging results and assays for inflammatory markers.
This research complied with all relevant national regulations, institutional policies, and the principles of the Declaration of Helsinki and was approved by the Dicle University Faculty of Medicine Ethics Committee (approval number: 06.05.2021 / 311).