AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2578-8965/127
Department of Obstetrics & Gynecology, Faculty of Medicine, Benha University, Benha. Egypt.
*Corresponding Author: Ali A. Bendary. Department of Obstetrics & Gynecology, Faculty of Medicine, Benha University, Benha. Egypt.
Citation: Ali A. Bendary, Waleed M.Tawfik. (2022). Comparative Study between Different Methods of Laparoscopic Hysterectomies, J. Obstetrics Gynecology and Reproductive Sciences. 6(5) DOI: 10.31579/2578-8965/127.
Copyright: © 2022 Ali A. Bendary. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 02 June 2022 | Accepted: 15 June 2022 | Published: 05 July 2022
Keywords: laparoscopic-assisted vaginal hysterectomy (LAVH); total laparoscopic hysterectomy (TLH); hysterectomy
Background: Hysterectomy is the second most common major surgical procedure performed on women after caesarean section. The incidence of hysterectomy is 4-6% out of which 90% are performed for benign indications.
Aim of the work: The aim of this study was to compare intra- and post-operative morbidity associated with two types of laparoscopic hysterectomy. Laparoscopic-Assisted Vaginal Hysterectomy (LAVH) and Total Laparoscopic Hysterectomy (TLH)
Patients and methods: A total of 80 women scheduled to undergo a hysterectomy for benign disease were subdivided into 2 groups; 40 women for LAVH and 40 women for TLH, Patients were excluded from the study if they had contraindication to laparoscopy. Intra- and post-operative evaluations including the duration of the operation uterine weight, frequency of intraoperative complication, and the difference between hemoglobin level prior to surgery and one day after surgery.
Results: LAVH took the longest operating time. As regard hemoglobin deficit that occurred after 24 hours of surgery, our study showed that TLH had largest Hb deficit (1.6 gm/dl) but still the Hb deficit not significantly different. As regard transfusion of blood, one case took blood in group LAVH and one case in group TLH. As regard other complications, the bladder was injured during plunt dissection of the bladder flap in group TLH and this case was having history of one cesarean section 10 years ago.
Conclusion: laparoscopic assisted vaginal hysterectomy showed lower complication but longer operative time than total laparoscopic hysterectomy group; also (LAVH) showed shorter hospital stay and need fewer analgesics so we considered this method the best when the patient accepted total removal of the uterus. While total laparoscopic hysterectomy showed the more blood loss and complication intraoperatively and postoperatiovely, but this complication is non-significant in cases of removal of the hole uterus.
Hysterectomy is the second most common major surgical procedure performed on women after caesarean section. In India, the incidence of hysterectomy is 4-6% out of which 90% are performed for benign indications [1].
While, the incidence of hysterectomy in the Western countries is 10-20% with the highest rate in the United States and the lowest in Norway and Sweden. There are various possible approaches to hysterectomy for benign disease of uterus; Abdominal Hysterectomy (AH), Vaginal Hysterectomy (VH) and Laparoscopic Hysterectomy (LH). Laparoscopic approach may be used either to facilitate the ease of vaginal delivery of uterus as in Laparoscopy Assisted Vaginal Hysterectomy (LAVH) or it may be carried out completely till final detachment of uterus from pelvic wall i.e. Total Laparoscopic Hysterectomy (TLH). Although Laparoscopic Hysterectomy (LH) takes longer time, its proponents have emphasized several advantages over abdominal hysterectomy in terms of intraoperative blood loss, less postoperative morbidity, rapid recovery time, shorter hospital stay, fewer febrile episodes and early return to normal activities[2].
Traditionally, abdominal hysterectomy has been used for gynaecological malignancy-when other pelvic disease is present, such as endometriosis or adhesions-or if the uterus is enlarged. It remains the "fallback option" if the uterus cannot be removed by another approach [3].
Vaginal hysterectomy was originally used only for prolapse, but it is now also used for menstrual abnormalities when the uterus is of fairly normal size. Vaginal hysterectomy is regarded as less invasive than abdominal hysterectomy [4].
In 1989, Reich et al. first reported a new procedure called laparoscopically assisted vaginal hysterectomy. Since then, laparoscopic hysterectomy has gained widespread popularity and subtotal and total laparoscopic hysterectomy became a standard of care for treating benign uterine pathology in many centers worldwide [2].
Laparoscopic hysterectomy requires greater surgical experience than abdominal and vaginal methods, the proportion of hysterectomies performed laparoscopically has gradually increased in the last decades. As experience is gained during the learning curve, the operation time, complication rate and hospital stay are decreased [5].
Laparoscopic-assisted vaginal hysterectomy provide minimally invasive way to accomplish a hysterectomy with decreasing length of accomplish a hysterectomy with decreasing length of hospital stay and time of return to normal activity [6].
To compare 2 types of laparoscopic hysterectomies including Laparoscopic-Assisted Vaginal Hysterectomy (LAVH) and Total Laparoscopic Hysterectomy (TLH) as regard demographic data, indications, weight of removed uteri, operative time, intra-operative blood loss, intra- and post-operative complications, need for analgesics and hospital stay.
This was prospective randomized study carried out in Obstetrics and Gynecology Department, between March 2021 to May 2022, all patients are recruited from Gynecological Outpatient Clinic.
In this study, 80 patients were divided into 2 groups:
Group A: 40 patients underwent laparoscopically assisted vaginal hysterectomy (L.A.V.H.).
Group B: 40 patients underwent total laparoscopic hysterectomy (T.L.H.).
Patient selection:
All patients scheduled to undergo a hysterectomy for benign uterine lesion such as:
*Leiomyoma.
*Endometrial hyperplasia.
*Dysfunctional uterine bleeding un-responding to medical treatment.
*Suspected adenomyosis.
The uterine size by examination and investigation was not more than sixteen weeks like gestation size.
Excluded patients from our study:
*Any suspected or confirmed malignancy in the uterus.
*Presence of any contraindication to laparoscopy.
*Any patients with uterine size > 16 weeks like gestation uterus.
All patients were subjected to:
* Full history taking.
* Complete examination
* Ultrasonographic evaluation.
* Laboratory investigation.
* Fractional curettage and histopathological assessment.
Preoperative preparation:
It is recommended that all patients eat lightly for 24 hours and be NPO at least 12 hours prior to surgery. A Fleet enema is helpful the night before laparoscopic surgery and an oral preparation using metronidazole and neomycin 3 days before surgery an empty bowel permits better visualization during surgery, and in the event of a bowel injury, decreases the possibility of complications. It should be carefully worded to explain expected postoperative discomfort and to differentiate it from severe pain that requires her to contact the surgeon with a telephone number that is answered 24 hours a day. Patients should be discharged with all the appropriate instructions and medication or a prescription for pain relief.24 hour after the surgery hemoglobin concentration is done to all patients and the hemoglobin deficit was calculated. Also, the operation time from skin incision to last suture is calculated accurately, the uterine weight, intraoperative and postoperative complications, need to analgesia and hospital stay.
Surgical technique: routine laparoscopic equipment that is essential for performing a successful laparoscopic hysterectomy includes:
* Standard laparoscopic tower containing a high-flow CO2 insufflator, camera and a light source.
* An operating table with leg stirrups and capability of placing the patient in steep Trendelenburg position is essential
* Some kind of bleeding control instrument such as, bipolar and unipolar electricity generator Ligasure vessel sealing instrument.
* A sturdy uterine mobilizer, capable of extreme anteversion and movement of the uterus in an arc of 45° to the right and left is important.
* We prefer the disposable scissors because reusable scissors are often not sharpened adequately for the extensive cutting involved in laparoscopic hysterectomy.
* Two good laparoscopic graspers with long jaws for grasping and manipulating the uterus, adnexal structures and bowel.
* Suction irrigator is essential to clear out the smoke if unipolar or bipolar energy is used and to remove the blood and blood clots.
Step 1: Trocar placement:
We routinely place a Veress needle in the lower edge of the umbilicus. We then insufflate to 20 mmHg prior to placement of any trocars. A 10- 12 mm trocar is then placed through a vertical intraumbilical incision for insertion of the telescope. tow additional 5 mm trocars are then placed into the peritoneal cavity. this pair were placed lateral to the inferior epigastric vessels approximately two fingerbreadths above the pubis. the third one was 12 mm and put in the suprapubic region. If a patient has had prior abdominal surgery, we will often place the 5 mm trocar first and then inspect the periumbilical area with a 5 mm laparoscope to evaluate adhesion of underlying omentum and bowel to the anterior abdominal wall. Whatever method is used for trocar insertion, it is crucial to use “backstop” measures to prevent rapid, uncontrolled thrusting of the trocar through the layers of the abdominal wall and into underlying structures and adhesions.
Step 2: Identification of the ureters:
The ureters should be identified prior to securing any supporting structures to the uterus. Knowledge of pelvic anatomy and the course of the ureter are crucial. In most cases the ureters are visible through the peritoneum. As long as the ureters are clearly identified through the peritoneum, it is reasonable not to dissect them when performing procedures such as a laparoscopic assisted vaginal hysterectomy.
Ligaments:
The round ligaments can easily be desiccated by using ligasure instrument. The uterus is deviated to the left by an assistant and a grasper is used to place the round ligament on traction. The round ligament is coagulated and cut in the middle of the ligament with the coagulating instrument introduced from the ipsilateral side.
Step 4: Securing infundibulopelvic and uterine-ovarian ligaments:
For women desiring removal of the ovaries, the suspensory ligament of the ovary (infundibulopelvic ligament). For women who want to preserve their ovaries, the uterine-ovarian ligaments and Fallopian tubes were sealed and cut medial to the ovary using ligasure atlas instrument 10 mm. but if we want to remove the ovaries, we cut the infundibelopelvic ligament itself being care of the course of the ureter.
Step 5: Creation of the bladder flap:
First, identify the vesico-uterine peritoneal fold. To facilitate identification of the vesico-uterine fold, have an assistant retrovert the uterus and push it cephalad. The upper junction of the vesico-uterine peritoneal fold is distinguished as a white line. Identification of the white line is important because, cephalad to the white line, the peritoneum is attached tightly to the uterus. Below this demarcation the peritoneum is loosely attached to the cervix and can be easily dissected away.
Using a grasper, place the vesicouterine fold on traction. Make a transverse incision just below the white line and dissect the bladder away from the lower uterine segment and cervix. In the right tissue plane, the dissection should be relatively bloodless. The middle band of loose connective tissue is the vesico-cervical ligament.
This ligament does not contain blood vessels and can be easily divided. laparoscopic scissors with electroenergy can be used to coagulate any small incidental bleeders during dissection. The lateral bands of connection on both sides of the cervix are bladder pillars. The bladder pillars contain blood vessels and should be desiccated prior to ligation. Dissection of the bladder laterally helps pull the ureters away from the cervix. To achieve this, incise the bladder peritoneum to the level of the round ligament. Continue dissection in the avascular plane and push the bladder caudad over the cervix to its junction with the anterior fornix of the vagina
Step 6: Securing the uterine arteries:
The broad ligaments on both sides are opened downward and towards the cervix, skeletonizing the uterine vessels. Once the uterine vessels are skeletonized they can be sealed laterally using ligasure atlas insteroment 10 mm, if necessary, to help control bleeding and identify the ureter when dealing with a large or cumbersome uterus. With meticulous dissection, the uterine vessels can be identified at the level of the ureteric canal as it crosses above the ureter. Knowledge of the course of the ureter is essential at this point to avoid injury. the uterine vessels can be secured medially as they enter the uterine body. The suction irrigator is used to push the body of the uterus to the opposite side
In cases of group (A)(L.A.VH.) After ligation of uterine artery, the laparoscopic approach is stopped and pneumoperitoneum is reversed, then the patient position is corrected into standard lithotomy position, then the cervix is grasped using vollessulume anteriorly and posteriorly. Using cold scalble or valley lap scalpel, we cut the vaginal mucosa surrounding the cervix, then the Mackenrodit ligment is grasped using 2 force grasspers and cutting is done between the 2 grasspers, then we transligate the attached end to the pelvic wall. This is done on each side. Vagina is closed and suspended to the makenrodet ligament. ligation was done using Vicryl 0 suture. In some cases, vaginal pack is left, then we change the position of the patient and laparoscopic underwater examination is done. The patient is instructed to be followed-up one week later and then after one month.
In cases of group (B)(T.L.H.) After dealing with the uterine artery, the manipulator is used to push the uterus to the left side during grasping and cutting the Machenrodit ligament on the right and vise verse this is don using ligasure instruments.
After that, we use the Vally laparoscopic hook or unipolar hook to open the vagina, we open the vagina anteriorly against the hard "ceramic" part in the manipulator and we move the ceramic part carefully to open the cuff laterally, then posteriorly. For fear of loss of pneumoperitoneum, we use a big sponge in plastic cover to pack the vagina tightly and surround the mobilizer. Then, we remove the uterus vaginally from the opening os.
We remove all the trocar under vision. CO2 was allowed to escape gradually, then remove the last trocar under vision. Also, lastly, we close the skin using non-absorbable silk suture which removed after 7 days.
After all methods the patients were followed up carefully for 24 hours and discharged if they were will to be examined after one week then after one month. Prior to discharge, each patient was evaluated and examined for vital signs and presence of any complications.
In the postoperative period we gave all patients analgesics in the form of diclofenac sodium 100 mg which is (NSAID) but if the patients are still complaining from pain, we gave here narcotic in the form of 100 mg pethidine single dose.
After 12 hour 1 gm cefotriaxon was given and before discharge we gave here instructions to take only semisolid food in the first day, diclofenac sodium tablet 50 mg if needed.
Statistical analysis: Data were entered checked and analyzed using EpiInfo version 6 and SPP for Windows version 8.
The mean age of group (A) was 44.7 years old with standard deviation of (SD) 2.4.The mean age of group (B) was 52 years old with SD 5.4
As regard the parity each group was subdivided into two groups, the first one who delivered less than 3 children and the 2nd group who delivered more than 3 children in group (A) 60% of its patients delivered less than three children and 40 (percentage) delivered more than 3 children. In group (B) 45 (percentage) delivered less than 3 children and 55 (percentage) delivered more than 3 children. As regarding BMI, In group (A) the mean of BMI was 24.7 kg/m2 with S.D. 2.7. In group (B) the mean of BMI was 24 kg/m2 with S.D. 3.2. The P. value in all demographic data was non-significant.
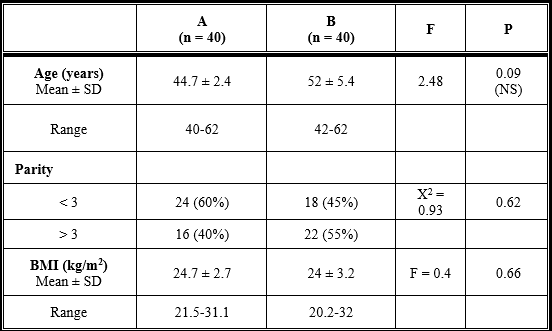
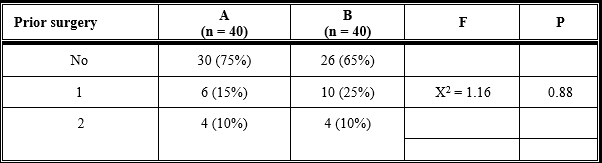
Table (2) shows percentage of previous laparotomy: In group (A) LAVH 15 cases 75% of women had no history of previous surgery, 3 only cases 15% had previous one laparotomy and 2 cases with prior history of 2 or more laparotomies. In group (B) TLH 13 cases 65% of women had no history of prior surgery, 5 (25%) of cases had prior one laparotomy and 2 10% of cases had prior 2 or more laparotomies. The data of prior surgery has no statistically significant.
The indication of laparoscopic hysterectomy in our study was only benign condition: Fibroid uterus, Endometrial hyperplasia, dysfunction uterine bleeding not responding to medical treatment and suspected adenomyosis all these indications are listed in table (3) which show: Fibroid uterus represented 35% in group (A) LAVH and 35% in group (B) TLH. Also, and hyperplasia represented 55% of cases in group (A) LAVH and 45% of cases in group (B) TLH. Dysfunction uterine bleeding (DUB) represented 10 (percentage) cases of group (B) No cases in group (A) LAVH. Suspected adenomyosis represented 10,ases in group (A) LAVH and 10,ases in group (B) TLH.
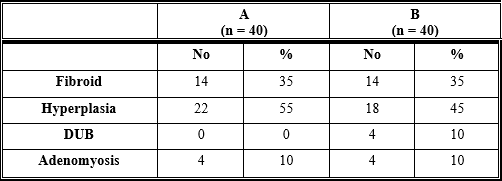
Table (4) compares the outcome measures evaluated during surgery. There was significant difference in the operating time among the 2 groups with shorter time observed in group A and longer time in group B. group (A) group (A) LAVH 104.1min S.D. 10.4. while group (B) TLH took 91.7 S.D.21.6 min. Also, this table show that the mean uterine weight in group A was 316.5 gm & S.D. 64.4. The mean uterine weight in group B was 286.79 SD 75.5. There was no statistical difference among the 2 groups.
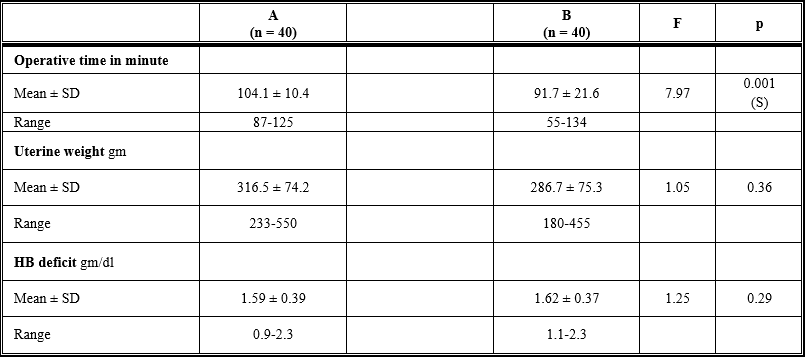
As regard hemoglobin (Hb) deficit gm/ dl.in group A and its mean was 1.59 g/dl with S.D. 0.39. In group (B) the mean of hemoglobin deficit was 1.62g/dl with SD 0.37, But not statistically difference appear between the 2 groups
Table (5) shows that blood transfusion occurs to suspected major blood loss. Conversion to laparotomy either due to uncontrolled bleeding or difficulty to manage complication. Bladder injury occurs during surgery.
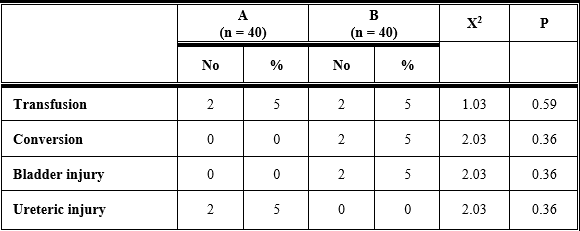
Only 4 out of 80 patients required whole blood transfusion. One patient in LAVH (group A) experienced intraoperative blood loss and one patient in the TLH (group B) for the same reason. Nevertheless, the difference among the groups were not significant. There is only 2 case of intraoperative complication which is bladder injury which occurred in group (B) (TLH) in patient which was a case of DUB and previous laparotomy was done as "cesarean section". During pushing the bladder flap downwards, the injury occurred, and immediate laparotomy was done and repairing of the bladder injury and completing hysterectomy. We asked urological surgeon to repair the bladder to avoid any injury to the ureteric orifices, this case remain in the hospital for 1 week and the catheter removed after 2 weeks. Ureteric injury noticed in the 5th day postoperatively when the patient complaint from watery discharge which is urinefarous in odor. IVP was done which discover very small ureteric fistula near the bladder wall. Consultation of urological surgeon was done and cystoureteroscopy was done to the patient with introduction of double J stent which is removed after 4 weeks, and the patient is good now this was occurred in group (A).
As shown in table (6), All patients took non-steroidal analgesic drug in the form of diclofenac sodium 100 mg (injection) and if the patient is still complaining from pain, we gave here 100 mg pethidine.
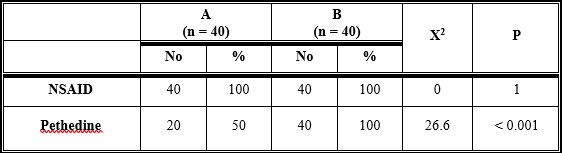
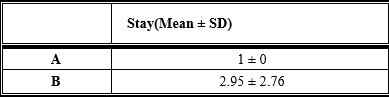
The lower mean consumption of analgesics was observed in the first group (A) and the larger consumption of analgesics observed in group B and this is statistically different. The hospital stay in all patients was only 24 hour postoperatively except in the complicated case of bladder injury where this case require hospitalization for 1 week and if we exclude this case, the time consumed postoperatively will be non-significant as shown in table (7).
Hysterectomy is the most common gynecological surgical procedure performed on women. There are three popular approaches to hysterectomy for benign disease; Abdominal Hysterectomy (AH), Vaginal Hysterectomy (VH) and Laparoscopic Hysterectomy (LH). Laparoscopic hysterectomy has three further subdivisions; Laparoscopic Assisted Vaginal Hysterectomy (LAVH) where a vaginal hysterectomy is assisted by laparoscopic procedures, Laparoscopic assisted Supracervical Hysterectomy (LASH), and Total Laparoscopic Hysterectomy (TLH) where there is no vaginal component, and the vaginal vault is sutured laparoscopically. Recently, robotic hysterectomy has also come in the field but it is not widely practiced yet [7].
Multicenter studies have shown clearly that hysterectomy is usually carried out by laparotomy, accounting for about three-quarters of all hysterectomies [8].
The primary disadvantage of abdominal hysterectomy is the prolonged recovery period mainly contributed by longer period of pain and general malaise. This may be due to the larger abdominal incision and the procedure of laparotomy itself [8].
Vaginal hysterectomy is associated with fewer complications, lower need for blood transfusion and shorter period of postoperative recovery. The progress in laparoscopic surgery made over the past few years has proved that Total Laparoscopic Hysterectomy (TLH) is a feasible technique [9].
Laparoscopic Assisted Vaginal Hysterectomy (LAVH) has been introduced as a surgical alternative to the standard methods of abdominal and non-descent vaginal hysterectomy.
Hysterectomy.
There are very few prospective randomized studies comparing various routes and types of hysterectomies. Most of the data published involves retrospective analysis of surgical technique but the Present study was a randomized prospective clinical analysis. For the operation time, our study showed that there is statistical deference among the 2 groups as the laparoscopic assisted vaginal hysterectomy (group A) showed the longest time (mean ± SD, 104 ± 10.4 minutes) due to time consuming during changing the position of the patient from trendelenburg to lithotomy position to do vaginal part of the surgery followed by reinsufflation and under water examination which took more time but TLH group (B) took about (mean ± SD, 91.7 ± 21.6 minutes).
Drahonovsky et al. (2015) did their study in Department of Gynecology and Obstetrics, 3rd Faculty of Medicine, Charles University, Czech Republic. The study was a prospective randomized study performed to a total of 125 women indicated to undergo hysterectomy for benign uterine disease were randomly assigned to three different groups (40 VH, 44 LAVH and 41 TLH). VH group showed the shortest operative time (66 minutes) and smallest drop in hemoglobin, while (TLH) group showed the longest operative time (111 minutes). (LAVH) group showed the longest amount of blood loss (306 ml) while (TLH) group showed the smallest amount of blood loss (184 ml), 3 cases out of 44 cases converted to laparotomy in (LAVH) group, 6 cases out of 41 cases converted to laparotomy in (TLH) group, one case of bladder injury in (LAVH) group out of 44 cases [10].
Our results are not in agreement with Drahonovsky et al. (2015) who showed that (LAVH) took shorter operation time than (TLH) [10].
For the hemoglobin deficit, our study stated that TLH showed the largest deficit (mean ± SD, 1.6 ± 0.37 gm/dl) and (LAVH) showed deficit of hemoglobin about (159 ± 0.39 gm/dl) and this is statistically not significant.
Mueller et al. (2019) did a study in the Department of Obstetrics and Gynecology, Erlangen University Hospital, Nuremberg, Germany was to compare Total Laparoscopic Hysterectomy (TLH) with Laparoscopically Assisted Supracervical Hysterectomy (LAVH) in women with uterine leiomyoma, 231 women underwent laparoscopic hysterectomies for the treatment of symptomatic fibroid. A total number of 113 women decided to undergo complete hysterectomy with removal of the cervix (TLH group) and 118 women wished to preserve the cervix (LAVH group). The complications occurred only in (TLH) group in the form of 2 cases of bladder injury, while no complications occurred in LASH group. The mean loss of hemoglobin in (TLH) group was 1.6 gm/dl, while in (LAVH) was 1.4 gm/dl. The hospital stay and use of analgesics were equal in both groups. He stated that (LAVH) group took shorter time than (TLH) group during the operation [11].
Mueller et al. (2019) accepted our results as they showed in their study that (LAVH) has less amount of Hb deficit (1.5 g/dl) than TLH in cases of leiomyoma which was (1.6 g/dl) in the first day post surgery.
In our prospective study, in the first group , no cases was taken blood transfusion but one case in group B was taken one unit of blood and this is due to hemorrhage from the descending cervical artery which took some time to be secured using ligasure instrument. In group B (TLH), there is 2 case was also taking blood transfusion due to bleeding from uterine artery which also was secured using ligasure instrument [11].
This transfusion rate is minimal and Drahonovsky et al. (2015) also gave blood to 2 cases in their study which was case of (LAVH).
Also, Mueller et al. (2019) had one case that was taken blood which was a case of (TLH) and this is in agreement with our study.
In our study, one case from 60 is transformed to laparotomy, this case had history of previous laparotomy which was cesarean section and during pushing bladder flab downwards, the bladder was opened and immediate laparotomy was done, the injured part is identified which was the trigon and consultant urosurgeon came immediately and close the tear after saving the ureteric orifices [10,11].
Drahonovsky et al. (2015) showed that (TLH) showed the largest conversion rate among the 3 groups as 6 cases conversed to laparotomy from 111 cases while in cases of LAVH 3 cases only converted to laparotomy from 85 cases [10].
For the hospital stay, in our study, group A the recovery was rapid, but in group B (TLH), one case took 2 days for recovery and another 4 cases took 7 days as there was urinary complication which necessitate hospital stay. So, if we exclude the 4 cases, there were no significant difference among 2 groups, but due to these 4 cases (TLH) showed the longest hospital stay duration and this is in agreement with the study of Mueller (2019) as the study showed the least hospital stay with group (LAVH) and longest stay in the group of (TLH). While Drahonovsky et al. (2015) study is not in agreement with our study as (LAVH) group showed the longest hospital stay duration and (TLH) group showed least hospital stay duration [10,11].
In our study the need for non-steroidal anti-inflammatory drugs was equal in all groups as all patients in the 2 groups were taken diclophenac sodium 100 mg injection in the early postoperative period but the need for narcotic was not needed in all patients, but the (TLH) group showed the largest number of cases who need narcotic.
Morelli et al. (2017) stated in his study that no statistically difference was found in the complication rate and postoperative recovery period between (TLH) and (LAVH).This study was done on one hundred and forty one patients who complained of symptomatic leiomyoma and abnormal uterine bleeding non-responding to medical treatment [12].
The results of Morelli et al. (2017) are not in agreement with the results of our study as we found significant difference in both postoperative stay and intraoperative complication between the (TLH) group and (LAVH) group as (TLH) took longer mean period of hospital stay, but (LAVH) took only 24 hours, but the longer duration in (TLH) group only occurred in 2 cases, one case converted to laparotomy due to bladder injury and the 2nd due to presence of drains which necessitate staying for another day and if we exclude these two cases, our results will be as the results of Morelli. For the complication rate in our study,there was no complication in group A(LAVH) while the complication rate more in (TLH) than (LAVH) but not significant, Morelli (2017) showed also that there was no significant difference between the 2 groups [12].
Long et al. (2012) in a study done on 120 patients to compare the operative and postoperative data between two groups; the first group where (LAVH) (n = 60) was done and 2nd group where (TLH) (n = 60) was done. They found that (LAVH) showed the shorter operation time than (TLH) , but they were using extracorporeal knot in ligation of the pedicles and this might be the cause of elongation of the operative time in (TLH) group. This result was not in agreement with the results of our study as we stated that (LAVH) group took the longest operation time and (TLH) group consumed shorter period during the operation and this happened with us, as we use Ligasure instrument in securing and cutting blood vessels and pedicles. Also, the time consumed during changing the position of the patient from Trendelenburg to lithotomy position during doing the vaginal part of the surgery [13].
Long et al. (2012) also stated that (LAVH) group stay for shorter period in the hospital than (TLH) group and this agreed with our results. Also, the complication rate between both groups was non-significant and this was in agreement with our results.
The study of Roy et al. (2020) showed that (TLH) took significantly longer time (105 ± 23 minutes) than (LAVH) (89 ± 21 minutes), and this results are not in agreement with our study which showed that (LAVH) group took longer operation time than (TLH) group. But if the mean blood loss was 290 ± 124 ml in (TLH) and 302 ± 130 ml in (LAVH), this means that(TLH ) group showed less blood loss than (LAVH) group and this is not in agreement with our study that stated the opposite. He also found that there were no statistically differences between (TLH) and (LAVH) groups in the postoperative stay. While our study showed that there was statistically difference in the postoperative stay where the group of (TLH) showed higher rate in the hospital stay and, in the complication, [1].
In a study done by Mousa et al. (2018) in Royal Vectoria Hospital, Montereal Canada, they stated that there were no statistically differences in the hospital stay between (LAVH) group and (TLH) group. Also, no statistical difference in the Hb deficit between the 2 group after the 1st postoperative day and this is agree with our result concerning Hb deficit only, but our result is not agreed with Mousa result's regarding hospital stay as in our result the length of hospital stay is more in group (TLH) than in (LAVH) group. Also, In the study of Mousa et al. (2018), no statistically difference between (LAVH) and (TLH) regarding major and minor complication. Also in our result, no statistically difference but there was one major complication in (TLH) group which was bladder injury which required conversion to laparotomy [14].
Jin and Jang (2018) in a study including 120 patients; 60 of them were underwent (LAVH) and 60 women underwent (TLH). There were no significant differences in patients' clinical characteristics (age and weight) and the hospital stay and this is in agreement with our result. They also found a longer operation time in (TLH) group (mean, 105 minutes) which is statistically different than (LAVH) group (86 mm), but this result is not matched with our results regarding operation time. Also, they showed that (LAVH) group has the merits of less blood loss than (TLH) group and this agreed with our result as blood loss in (LAVH) group was 1.59 gm/dl while in(TLH) was 1.62 gm/dl.
Laparoscopic assisted vaginal hysterectomy showed lower complication but longer operative time than total laparoscopic hysterectomy group; also (LAVH) showed shorter hospital stay and need fewer analgesics so we considered this method the best when the patient accepted total removal of the uterus. While total laparoscopic hysterectomy showed the more blood loss and complication intraoperatively and postoperatiovely, but this complication is non-significant in cases of removal of the hole uterus.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti
Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation. “The peer review process was efficient and constructive, and the editorial office provided excellent communication and support throughout. The journal ensures scientific rigor and high editorial standards, while also offering a smooth and timely publication process. We sincerely appreciate the work of the editorial team in facilitating the dissemination of innovative approaches such as the Bonori Method.” Best regards, Dr. Matteo Bonori.

I recommend without hesitation submitting relevant papers on medical decision making to the International Journal of Clinical Case Reports and Reviews. I am very grateful to the editorial staff. Maria Emerson was a pleasure to communicate with. The time from submission to publication was an extremely short 3 weeks. The editorial staff submitted the paper to three reviewers. Two of the reviewers commented positively on the value of publishing the paper. The editorial staff quickly recognized the third reviewer’s comments as an unjust attempt to reject the paper. I revised the paper as recommended by the first two reviewers.

Dear Maria Emerson, Editorial Coordinator, Journal of Clinical Research and Reports. Thank you for publishing our case report: "Clinical Case of Effective Fetal Stem Cells Treatment in a Patient with Autism Spectrum Disorder" within the "Journal of Clinical Research and Reports" being submitted by the team of EmCell doctors from Kyiv, Ukraine. We much appreciate a professional and transparent peer-review process from Auctores. All research Doctors are so grateful to your Editorial Office and Auctores Publishing support! I amiably wish our article publication maintained a top quality of your International Scientific Journal. My best wishes for a prosperity of the Journal of Clinical Research and Reports. Hope our scientific relationship and cooperation will remain long lasting. Thank you very much indeed. Kind regards, Dr. Andriy Sinelnyk Cell Therapy Center EmCell

Dear Editorial Team, Clinical Cardiology and Cardiovascular Interventions. It was truly a rewarding experience to work with the journal “Clinical Cardiology and Cardiovascular Interventions”. The peer review process was insightful and encouraging, helping us refine our work to a higher standard. The editorial office offered exceptional support with prompt and thoughtful communication. I highly value the journal’s role in promoting scientific advancement and am honored to be part of it. Best regards, Meng-Jou Lee, MD, Department of Anesthesiology, National Taiwan University Hospital.

Dear Editorial Team, Journal-Clinical Cardiology and Cardiovascular Interventions, “Publishing my article with Clinical Cardiology and Cardiovascular Interventions has been a highly positive experience. The peer-review process was rigorous yet supportive, offering valuable feedback that strengthened my work. The editorial team demonstrated exceptional professionalism, prompt communication, and a genuine commitment to maintaining the highest scientific standards. I am very pleased with the publication quality and proud to be associated with such a reputable journal.” Warm regards, Dr. Mahmoud Kamal Moustafa Ahmed

Dear Maria Emerson, Editorial Coordinator of ‘International Journal of Clinical Case Reports and Reviews’, I appreciate the opportunity to publish my article with your journal. The editorial office provided clear communication during the submission and review process, and I found the overall experience professional and constructive. Best regards, Elena Salvatore.

Dear Mayra Duenas, Editorial Coordinator of ‘International Journal of Clinical Case Reports and Reviews Herewith I confirm an optimal peer review process and a great support of the editorial office of the present journal
Dear Editorial Team, Clinical Cardiology and Cardiovascular Interventions. I am really grateful for the peers review; their feedback gave me the opportunity to reflect on the message and impact of my work and to ameliorate the article. The editors did a great job in addition by encouraging me to continue with the process of publishing.

Dear Cecilia Lilly, Editorial Coordinator, Endocrinology and Disorders, Thank you so much for your quick response regarding reviewing and all process till publishing our manuscript entitled: Prevalence of Pre-Diabetes and its Associated Risk Factors Among Nile College Students, Sudan. Best regards, Dr Mamoun Magzoub.

International Journal of Clinical Case Reports and Reviews is a high quality journal that has a clear and concise submission process. The peer review process was comprehensive and constructive. Support from the editorial office was excellent, since the administrative staff were responsive. The journal provides a fast and timely publication timeline.
Dear Maria Emerson, Editorial Coordinator of International Journal of Clinical Case Reports and Reviews, What distinguishes International Journal of Clinical Case Report and Review is not only the scientific rigor of its publications, but the intellectual climate in which research is evaluated. The submission process is refreshingly free of unnecessary formal barriers and bureaucratic rituals that often complicate academic publishing without adding real value. The peer-review system is demanding yet constructive, guided by genuine scientific dialogue rather than hierarchical or authoritarian attitudes. Reviewers act as collaborators in improving the manuscript, not as gatekeepers imposing arbitrary standards. This journal offers a rare balance: high methodological standards combined with a respectful, transparent, and supportive editorial approach. In an era where publishing can feel more burdensome than research itself, this platform restores the original purpose of peer review — to refine ideas, not to obstruct them Prof. Perlat Kapisyzi, FCCP PULMONOLOGIST AND THORACIC IMAGING.

Dear Grace Pierce, International Journal of Clinical Case Reports and Reviews I appreciate the opportunity to review for Auctore Journal, as the overall editorial process was smooth, transparent and professionally managed. This journal maintains high scientific standards and ensures timely communications with authors, which is truly commendable. I would like to express my special thanks to editor Grace Pierce for his constant guidance, promt responses, and supportive coordination throughout the review process. I am also greatful to Eleanor Bailey from the finance department for her clear communication and efficient handling of all administrative matters. Overall, my experience with Auctore Journal has been highly positive and rewarding. Best regards, Sabita sinha

Dear Mayra Duenas, Editorial Coordinator of the journal IJCCR, I write here a little on my experience as an author submitting to the International Journal of Clinical Case Reports and Reviews (IJCCR). This was my first submission to IJCCR and my manuscript was inherently an outsider’s effort. It attempted to broadly identify and then make some sense of life’s under-appreciated mysteries. I initially had responded to a request for possible submissions. I then contacted IJCCR with a tentative topic for a manuscript. They quickly got back with an approval for the submission, but with a particular requirement that it be medically relevant. I then put together a manuscript and submitted it. After the usual back-and-forth over forms and formality, the manuscript was sent off for reviews. Within 2 weeks I got back 4 reviews which were both helpful and also surprising. Surprising in that the topic was somewhat foreign to medical literature. My subsequent updates in response to the reviewer comments went smoothly and in short order I had a series of proofs to evaluate. All in all, the whole publication process seemed outstanding. It was both helpful in terms of the paper’s content and also in terms of its efficient and friendly communications. Thank you all very much. Sincerely, Ted Christopher, Rochester, NY.