AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2690-4861/609
1Department of Obstetrics and Gynecology, Amrita Institute of Medical Sciences and Research Centre, Amrita Vishwavidyapeetham, Kochi 682041, India.
2Department of Pediatrics Amrita Institute of Medical Sciences and Research Centre, Amrita Vishwavidyapeetham, Kochi 682041, India.
3Health Science Research. Amrita Institute of Medical Sciences and Research Centre, Amrita Vishwavidyapeetham, Kochi 682041, India.
*Corresponding Author: Cherupally Krishnan Nair, Health Science Research. Amrita Institute of Medical Sciences and Research Centre, Amrita Vishwavidyapeetham, Kochi 682041, India.
Citation: Vinita Murali, Sheena P. Kochumon, Pragalya Loganathan, Radhamany K and Cherupally K. Nair, (2025), Comparative Analysis Of Preoperative And Postoperative Findings In Patients With Endometrial Hyperplasia: A Clinical Study, International Journal of Clinical Case Reports and Reviews, 25(2); DOI:10.31579/2690-4861/609
Copyright: © 2025, Cherupally Krishnan Nair. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 07 January 2025 | Accepted: 17 March 2025 | Published: 14 April 2025
Keywords: abnormal uterine bleeding; endometrial hyperplasia; hormone replacement therapy
Aim and Objective: The objective of this study is to compare preoperative and postoperative findings in patients diagnosed with endometrial hyperplasia, focusing on clinical symptoms, histopathological features, co-morbidities, surgical outcomes, and recurrence rates. This analysis aims to identify significant differences between hyperplasia with and without atypia, contributing to improved management strategies and clinical decision-making in patients undergoing treatment for endometrial hyperplasia.
Methodology: This observational study was conducted at Amrita Institute of Medical Sciences in Kochi, Kerala, over two years (July 2019 to July 2021) and approved by the institutional ethical committee. It included 68 women diagnosed with endometrial hyperplasia via endometrial biopsy who were planned for hysterectomy, and excluding those on tamoxifen or hormone replacement therapy. Data on age, menopausal status, time between biopsy and hysterectomy, and histopathological findings were collected and reviewed by a single pathologist, using WHO criteria for classification.
Result: In this study of preoperative and postoperative findings in endometrial hyperplasia, the mean age of patients with hyperplasia with atypia was 49.20 years (n=41) compared to 50.95 years for those without atypia (n=27), with no significant difference in mean endometrial thickness (12.5 mm vs. 11.05 mm, p=0.547). Cystic spaces were more prevalent in the without atypia group (48.1% vs. 24.4%, p=0.063). Postoperatively, complications were low and comparable across groups, with infection rates of 7.3% in atypia and 7.4% in without atypia. The recurrence rates were similar at 12.2% for hyperplasia with atypia and 11.1% for without atypia (p=0.857), indicating that atypia did not adversely affect long-term outcomes. Follow-up symptoms showed a low prevalence of ongoing heavy menstrual bleeding (10.0% for atypia vs. 7.4% for without atypia) and other irregularities, suggesting effective symptom management through surgical intervention.
Conclusion: In conclusion, the study indicates that preoperative and postoperative findings in endometrial hyperplasia, whether atypical or non-atypical, show no significant differences in clinical profiles or outcomes. Both groups exhibited similar mean ages, endometrial thickness, and low rates of postoperative complications. The recurrence rates were also comparable, with 12.2% in the atypical group and 11.1% in the non-atypical group, suggesting that the presence of atypia does not negatively affect long-term outcomes. Overall, these results highlight the effectiveness of surgical intervention for endometrial hyperplasia.
Endometrial hyperplasia is characterized by the thickening of the endometrium, marked by the proliferation of irregularly sized and shaped glands and an increased gland-to-stroma ratio. This condition is a direct precursor to invasive disease and can progress to malignancy if left untreated. It primarily arises due to an imbalance in hormonal regulation, where excess estrogen stimulates endometrial proliferation, while progesterone normally acts to limit this growth. Without proper hormonal balance, the endometrium undergoes a series of architectural and cytological changes, leading to conditions ranging from hyperplasia without atypia to more severe forms like endometrial intraepithelial neoplasia and ultimately, endometrial cancer [1, 2]. A significant incidence rate of 133 per 100,000 per year is observed, particularly post-menopause, highlighting the condition's relevance in gynaecological health [3].
While atypical hyperplasia is more frequently diagnosed in women aged 60 to 64, the true incidence of endometrial hyperplasia may be underreported due to individuals often seeking medical attention only after symptoms have subsided [4]. This condition shares common risk factors with endometrial cancer and is considered a direct precursor in many instances. The rising incidence of endometrial cancer is attributed to factors such as an aging population and increasing obesity rates, despite low public awareness [5, 6, 7]. Currently, there are no routine screening procedures for endometrial hyperplasia or its lesions, making diagnosis reliant on evaluations of abnormal uterine bleeding [8]. The American Cancer Society has concluded that evidence is insufficient to support routine screening in both premenopausal and postmenopausal women, even those at high risk [9].
The primary risk factors for endometrial hyperplasia include elevated estrogen levels and conditions leading to reduced progesterone effects. Non-modifiable factors, such as age, significantly influence the risk, with hyperplasia being most commonly diagnosed in women aged 50 to 54 [10]. Menstrual history also plays a crucial role, with postmenopausal women, those with early menarche or late menopause, and nulliparous women being at higher risk [11]. Obesity is particularly impactful as it correlates with an increased risk of endometrial hyperplasia and cancer; higher body mass index (BMI) is associated with elevated estradiol levels due to increased conversion of androgens to estrogens in adipose tissue ]12, 13]. Other factors, including type II diabetes, chronic low-grade inflammation, and conditions like polycystic ovarian syndrome (PCOS), also contribute to the risk through mechanisms promoting prolonged estrogen exposure and cellular proliferation (14, 15).
Hereditary conditions such as Lynch syndrome and Cowden syndrome further illustrate the genetic underpinnings of endometrial hyperplasia and cancer. Lynch syndrome, associated with mutations in mismatch repair (MMR) genes, presents a lifetime risk of 25-60% for endometrial cancer [16]. Endometrial hyperplasia in Lynch syndrome patients exhibits molecular similarities with endometrial and ovarian carcinomas, reinforcing the notion of early convergence in tumorigenesis [17]. Similarly, Cowden syndrome, linked to germline mutations in the PTEN gene, is characterized by multiple hamartomas and an elevated risk for several cancers, including endometrial cancer [18, 19]. The loss of PTEN function leads to unchecked cellular growth, with early loss of PTEN activity in endometrial hyperplasia being associated with malignancy progression [20]. Understanding these conditions emphasizes the critical need for vigilant monitoring and potential prophylactic measures in at-risk populations [21, 22].
Study Design and Setting
This observational study was conducted at Amrita Institute of Medical Sciences, Kochi, Kerala, India, a tertiary care referral center. The study was approved by the institutional ethical committee and spanned a period of two years, from July 2019 to July 2021. A total of 68 women who reported to the gynaecological outpatient department (OPD) and were diagnosed with endometrial hyperplasia during the evaluation for abnormal uterine bleeding were enrolled in the study.
Inclusion and Exclusion Criteria
The study included women who were diagnosed with endometrial hyperplasia based on endometrial biopsy and were subsequently planned for hysterectomy. All histopathological analyses on endometrial biopsy and hysterectomy were conducted at our institute. Exclusion criteria included women who were planned for hysterectomy based on an endometrial biopsy diagnosis from outside our institute and those who were on tamoxifen or hormone replacement therapy (HRT).
Data collection process: Patients included in the study had reported to the Department of Obstetrics and Gynaecology during the study period and underwent endometrial sampling to evaluate abnormal uterine bleeding. The histopathological diagnosis of endometrial hyperplasia was reviewed and classified according to the World Health Organization (WHO) criteria, which distinguishes endometrial hyperplasia into two categories: with atypia and without atypia.
Data collected for the study included patient age, menopausal status, time interval between endometrial biopsy and hysterectomy, type of endometrial hyperplasia identified in curettage specimens, and the pathological diagnosis in hysterectomy specimens. All preoperative and postoperative pathological specimens were reviewed by a single pathologist. The histopathological findings from the endometrial biopsy were compared and correlated with those from the hysterectomy specimens. The consistency rate was determined by dividing the number of patients with consistent diagnoses on both specimens by the total number of patients included in the study.
Sample Size
The sample size was calculated based on the consistency rate of 45
A total of 68 study participants included in this study. The mean age of patients with hyperplasia with atypia (49.20 years) and without atypia (50.95 years). The endometrial thickness is similar across both groups (12.5 mm vs. 11.05 mm), with no significant difference (p=0.547). The presence of cystic spaces is more common in patients without atypia (48.1%) compared to those with atypia (24.4%). Heavy menstrual bleeding is the most common presenting complaint, particularly in those with atypia (61.8%), indicating that more severe symptoms may correlate with atypical changes. (Table 1)
| Parameter | Hyperplasia with Atypia (n=41) | Hyperplasia without Atypia (n=27) | P Value |
|---|---|---|---|
| Mean Age (years) | 49.20 ± 5.4 | 50.95 ± 6.8 | 0.265 |
| Mean Endometrial Thickness (mm) | 12.5 ± 4.6 | 11.05 ± 5.06 | 0.547 |
| Cystic Spaces Present (%) | 10 (24.4) | 13 (48.1) | 0.063 |
| Presenting Complaints (%) | |||
| - Heavy Menstrual Bleeding | 21 (61.8) | 13 (38.2) | |
| - Postmenopausal Bleeding | 8 (53.3) | 7 (46.7) | |
| - Irregular Cycles | 6 (54.5) | 5 (45.5) | |
| - Amenorrhea | 6 (75) | 2 (25) |
Table 1: Preoperative Findings in Endometrial Hyperplasia
The analysis of co-morbidities, ultrasound findings, and endometrial sampling techniques in relation to the consistency rate revealed no statistically significant associations. Among patients with co-morbidities, 29.7% were in the consistent group, while 41.9% were in the inconsistent group (p=0.294), indicating no significant relationship. Similarly, ultrasound findings such as adenomyosis, fibroids, and their combination did not show any significant differences between the consistent and inconsistent groups, with the combination being slightly more frequent in the consistent group (39.4% vs. 23.1%), but still not significant (p=0.632). Endometrial sampling techniques, including endometrial aspiration and Pipelle biopsy, also showed no significant difference in consistency rates (p=0.423), with 52.8% consistency for aspiration and 60% for Pipelle biopsy. These findings suggest that none of these variables significantly influenced the consistency rate. (Table 2)
| Variable | Consistent (%) | Inconsistent (%) | P Value |
|---|---|---|---|
| Co-Morbidities | 0.294 | ||
| Yes | 11 (29.7%) | 13 (41.9%) | |
| No | 26 (70.3%) | 18 (58.1%) | |
| Ultrasound Findings | 0.632 | ||
| Adenomyosis | 9 (27.3%) | 9 (34.6%) | |
| Fibroid | 9 (27.3%) | 9 (34.6%) | |
| Fibroid + Adenomyosis | 13 (39.4%) | 6 (23.1%) | |
| Ovarian Cyst | 2 (6.1%) | 2 (7.7%) | |
| Endometrial Sampling Techniques | 0.423 | ||
| Endometrial Aspiration (n=53) | 28 (52.8%) | 25 (47.2%) | |
| Pipelle Biopsy (n=15) | 9 (60%) | 6 (40%) |
Table: 2: Co-Morbidities, Ultrasound Findings, and Endometrial Sampling Techniques with Consistency Rate
The rates of postoperative complications are generally low in both groups, indicating that surgical intervention for endometrial hyperplasia is relatively safe. The incidence of infection is similar (7.3% vs. 7.4%), which suggests that the presence of atypia does not influence the likelihood of infection post-surgery. Haemorrhage rates are also comparable, with no significant difference between groups, indicating effective management in both cohorts.The overall low complication rates may reflect careful surgical techniques and patient management in both groups.(Table 3)
| Parameter | Hyperplasia with Atypia (n=41) | Hyperplasia without Atypia (n=27) | P Value |
|---|---|---|---|
| Postoperative Complications (%) | |||
| - Infection | 3 (7.3) | 2 (7.4) | |
| - Hemorrhage | 1 (2.4) | 1 (3.7) | |
| - Other Complications | 2 (4.9) |
|
Table 3: Postoperative Findings in Endometrial Hyperplasia
The recurrence rate for endometrial hyperplasia is similar between groups (12.2% vs. 11.1%), with a p-value of 0.857 indicating no significant difference, suggesting that the presence of atypia does not adversely affect long-term outcomes.Follow-up symptoms reveal that a small percentage
of patients in both groups continue to experience heavy menstrual bleeding and other menstrual irregularities. The low rates of continued symptoms at follow-up indicate that surgical intervention may effectively alleviate the clinical manifestations of endometrial hyperplasia. (Figure1)
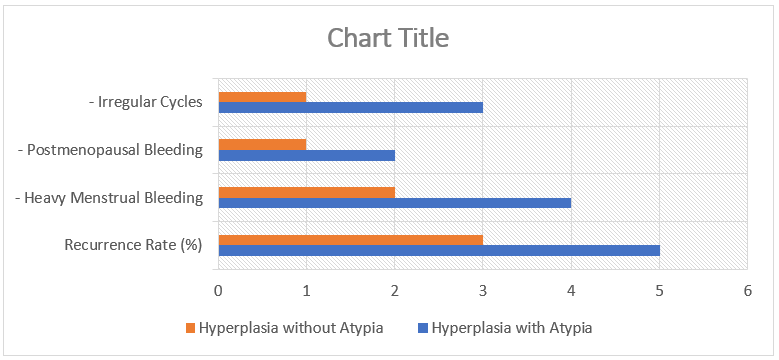
Figure 1: Follow-Up Findings
The primary objective of this study was to compare preoperative and postoperative histopathological findings in patients diagnosed with endometrial hyperplasia, focusing on clinical symptoms, co-morbidities, ultrasound findings, sampling techniques, surgical outcomes, and recurrence rates. The results of this analysis provide valuable insights into the diagnostic reliability of endometrial hyperplasia and its progression, with implications for clinical decision-making and patient management.
Our study found that preoperative clinical symptoms, such as heavy menstrual bleeding and postmenopausal bleeding, were common in both hyperplasia with atypia and without atypia, with heavy menstrual bleeding being more frequent in patients with atypia (61.8%). These findings align with previous studies, such as the work by consistency rates ranging from 41.3% to 79.5%, depending on the presence of atypia. We observed higher consistency in patients with atypia (63.7%) than in those without atypia (40.7%), suggesting that atypical hyperplasia may be more reliably diagnosed through preoperative biopsy. The variability in consistency rates across studies highlights the challenges of achieving diagnostic uniformity, potentially due to differences in sampling techniques, interobserver variability, and the nature of the lesions themselves.
Endometrial sampling techniques, including Pipelle biopsy and endometrial aspiration, did not show statistically significant differences in diagnostic accuracy (p=0.423). However, consistency rates for Pipelle biopsy were slightly higher (60%) than for aspiration (52.8%). This finding contrasts with studies such as Navakumar et al., [24] who reported higher consistency rates for both techniques, suggesting that further refinement and standardization in sampling protocols may improve diagnostic accuracy.
Postoperative complications were low across both groups, with no significant difference between hyperplasia with and without atypia. These findings suggest that surgical intervention for endometrial hyperplasia is relatively safe, and that the presence of atypia does not increase the risk of postoperative complications. Our recurrence rates were also similar between groups (12.2% vs. 11.1%, p=0.857), indicating that atypia may not necessarily predict higher recurrence rates.
The study's results also highlight the role of co-morbidities, such as diabetes mellitus and hypertension, in endometrial hyperplasia. While these conditions were prevalent among our patients, they did not significantly impact the consistency rates of preoperative and postoperative histopathological findings. This suggests that factors such as the quality of biopsy samples and pathologist interpretation may play a more significant role in diagnostic accuracy than co-morbid conditions.
In conclusion, this study underscores the importance of reliable preoperative histopathological evaluation in patients diagnosed with endometrial hyperplasia. While consistency rates between preoperative biopsy and postoperative findings were moderate, particularly in cases with atypia, there remains a risk of diagnostic variability. The presence of atypia appears to be associated with more severe clinical symptoms but does not significantly affect surgical outcomes or recurrence rates. Ongoing efforts to standardize diagnostic criteria, improve sampling techniques, and enhance preoperative assessment are essential for optimizing patient management. Future research should focus on larger, multicenter studies to validate these findings and provide clearer guidelines for the diagnosis and treatment of endometrial hyperplasia.
Not applicable.
none.
No conflict of interest for this study.
None.
All authors contributed equally