AUCTORES
Globalize your Research
Review Article | DOI: https://doi.org/DOI:10.31579/2692-9406/121
1 Department of Neurosurgery, University of Florida, Gainesville.
*Corresponding Author: Brandon Lucke-Wold, Department of Neurosurgery, University of Florida, Gainesville.
Citation: Michelot Michel, Noelle Lucke-Wold, Mohammad Reza Hosseini, Eric Panther, Ramya Reddy and Brandon Lucke-Wold, (2022) CNS Lymphoma: Clinical Pearls and Management Considerations. J. Biomedical Research and Clinical Reviews. 7(2); DOI:10.31579/2692-9406/121
Copyright: © 2022 Brandon Lucke-Wold, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 19 May 2022 | Accepted: 06 June 2022 | Published: 27 June 2022
Keywords: CNS Lymphoma; management considerations; diagnosis; treatment
Primary CNS lymphoma presents unique challenges for the clinician. New evidence has emerged regarding the appropriate workup, management considerations, and treatment. In this paper, we highlight the clinical presentations, disease prognosis, and management considerations. We place specific emphasis on the decision tree for immunocompetent and immunocompromised. The key imaging characteristics are discussed. Once biopsy prove lymphoma, important management considerations are addressed. We highlight need for follow up and role for surgery verse radiation. Finally, we present emerging treatment options and pre-clinical work that will be making its way through the pipeline. This up-to-date review will serve as a key learning tool for clinicians and researchers
Primary CNS lymphoma (PCNSL) represents a rare subset of non-Hodgkin lymphoma that is confined to the CNS without systemic involvement. PCNSL accounts for approximately 4% of newly diagnosed CNS tumors [1,2]. In the US, approximately 1500 patients are newly diagnosed each year [3]. PCNSL can arise in both immunocompetent and immunosuppressed patients, such as those with HIV/AIDS, post-transplant patients, and those on other immunosuppressive medications [3,4]. Although it is relatively rare in the immunocompetent population, the incidence rate has increased in recent years, with a predilection for patients over the age of 60 [5].
Clinical Presentations
PCNSL is classically isolated to the brain. Within the brain, it is often found in the periventricular white matter, basal ganglia, and corpus callosum [6]. To a lesser extent it can also arise from the spinal cord, cerebrospinal fluid, leptomeninges, and eyes [7,8]. The location of the lesion is the main driver of symptom presentation with up to 80% of patients presenting with focal neurological deficits [9,10]. Other presentations include neuropsychiatric symptoms and signs of elevated intracranial pressure [11]. Compared to other primary CNS lesions, seizures are relatively uncommon [11].
Disease Prognosis
Median overall survival (OS) for patients with untreated PCNSL is approximately 1.5 months [12]. OS rates at 5-years have been reported to be 29.3% [13]. Treatment of PCNSL has traditionally consisted of brain radiation and high-dose methotrexate (HDMTX), with many patients achieving a curative response. Although aggressive treatment and other favorable prognostic factors often lead to a cure, nearly 36% of patients relapse within 2 years of remission [14]. The prognosis of PCNSL relapse after primary radiation and chemotherapy is poor with a previously reported median survival of 2-4 months [15].
Diagnostic Workup
When suspicion arises for primary CNS lymphoma, diagnostic workup (Figure 1) includes imaging, biopsy, serological and cerebrospinal fluid (CSF) analysis, ophthalmologic examination, and evaluation for systemic involvement. We discuss some of the key principles of workup below.
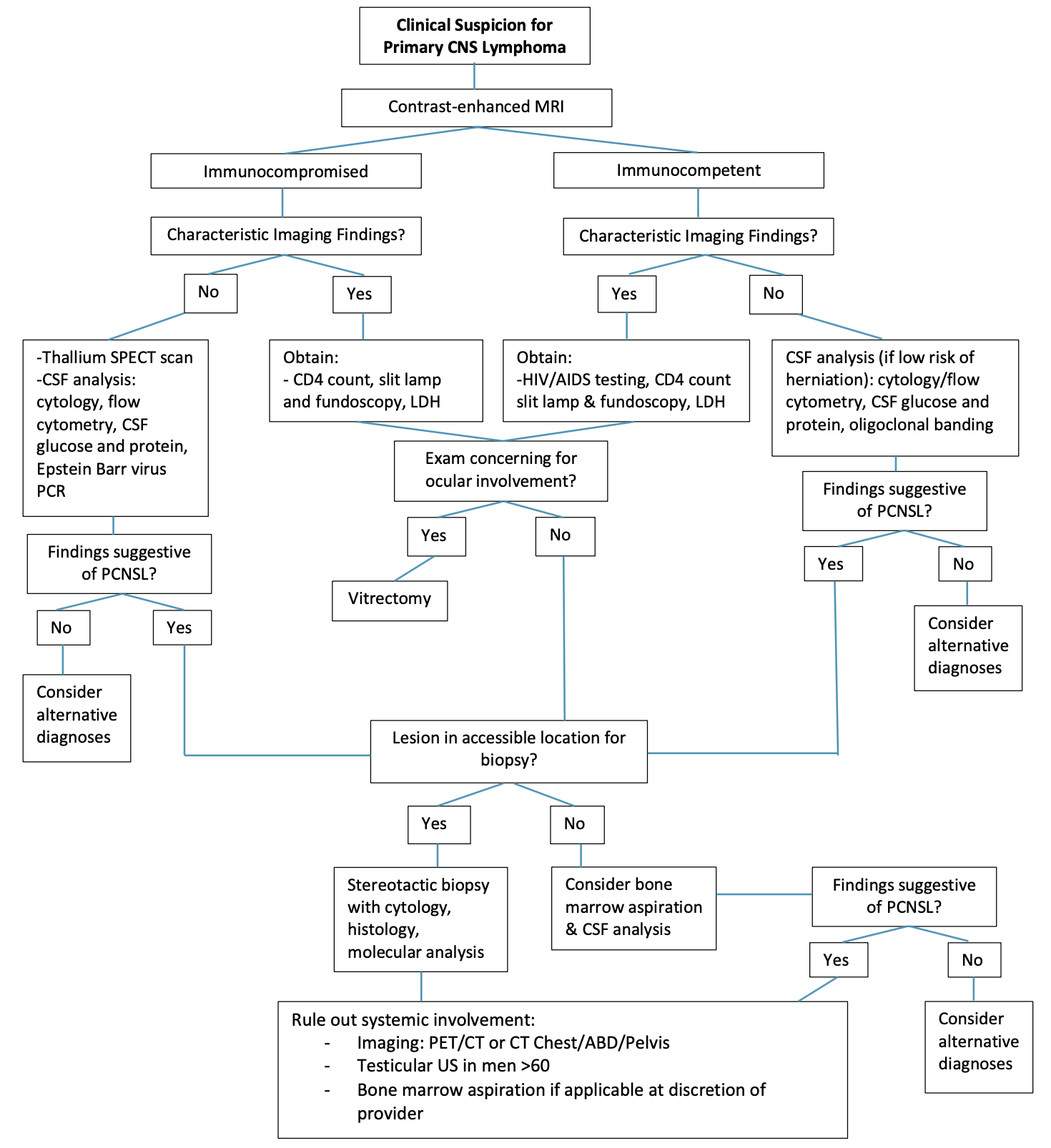
Diagnostic Imaging
Contrast enhanced MRI is the primary imaging modality recommended to evaluate for primary CNS lymphoma. As soon as PCNSL is suspected, an imaging study should be performed. It is common for CT scans and MRI to reveal PCNSL, which is hypercellular, has a high nuclear/cytoplasmic ratio, disrupts blood-brain barriers, and attacks the superficial and periventricular regions of the brain. However, CT negative findings are not an absolute indication of PCNSL because false-negative CTs can also occur [16]. It is recommended to use fluid-attenuated inversion recovery (FLAIR) before and after contrast injection. Traditional sequences include T1WI pre, and post-contrast, FLAIR,
T2WI and DWI [17]. Recently, CE-T2W FLAIR shows promise in assessing for subtle leptomeningeal and pachymeningeal disease [18].
The location of the lesion is predominantly supratentorial in the white matter of the frontal or parietal lobes or subependymal regions, although infratentorial lesions have been found to be associated with poorer prognosis and outcomes [19-21]. Other sites affected by primary CNS lymphoma include the eye, spinal cord, nerves, or disseminated systemic involvement [11].
Immunocompetency alters imaging findings
Imaging findings typically vary between immunocompetent patients and immunocompromised patients. Typical findings in immunocompetent patients include intense and homogenously enhancing single lesions (60–70% of cases) or multiple lesions (30–40% of cases) without necrosis and with relatively minimal edema, usually localized in the periventricular space. In contrast, immunocompromised patients are more likely to have multifocal lesions with irregular or peripheral contrast enhancement in contrast-enhanced T1 sequences due to the presence of necrotic regions. Hemorrhage is more common in this group; however, is not universally present [22]. This occasionally presents a diagnostic challenge as similar findings are present in immunocompromised patients with cerebral toxoplasmosis or progressive multifocal leukoencephalopathy as well. Thallium 201 single photon emission (SPECT) CT is a helpful adjuvant imaging tool in these clinical situations as increased uptake is observed in CNS lymphoma [23].
AIDS-defining illnesses, including cryptococcosis, can also present with peripherally enhancing cryptococcosis, but they can be distinguished by dilated perivascular spaces with pseudocyst formation and superimposed leptomeningeal enhancement. In addition to ring-enhancing tuberculomas, leptomeningeal enhancement, especially in the basal cisterns, and patchy meningeal enhancement are common findings in CNS tuberculosis [24].
After diagnosis confirmation and treatment initiation, contrast enhanced MRI is routinely performed to evaluate treatment response. The degree of contrast enhancement for these lesions may vary subtly between institutions, magnetic strength (tesla), contrast dosing, timing, and imaging protocols [18]. It is recommended to use the same scanner capabilities and protocols. This should include consistency in contrast dose and administration timing as these subtleties may alter the degree of detected lesion enhancement [18].
Differentiating PCNSL from glioblastoma on imaging
A diffusion-weighted image can be particularly useful in distinguishing PCNSL from other brain tumors, such as glioblastoma, due to PCNSL's high cellularity, which prevents water molecules from diffusing [25]. T1-weighted images frequently indicate hyper- or isointense lesions, whereas T2-weighted images frequently demonstrate isointense or hypo-intense lesions. Necrosis is common in conventional MR imaging in glioblastoma, while homogeneous enhancement without necrosis indicates PCNSL [26]. The conventional findings may, however, overlap in cases of atypical glioblastoma with or without necrosis and atypical PCNSL with necrosis, resulting in difficult differentiation [27]. Since the histological analysis has indicated that there are distinct differences in the microenvironmental tumor vasculature between these two tumor types [28]. it is possible to assess microvascular permeability and neovascularization noninvasively using dynamic contrast-enhanced MRI (DCE) and dynamic susceptibility contrast MRI (DSC) [29]. According to DSC MRI, glioblastoma has a higher cerebral blood volume than PCNSL. Although DSC-MRI agents have a greater effect on T2 than DCE-MRI agents, T2 effects decrease when the agents enter the interstitial space [30], whereas T1 effects persist when they enter the interstitial space. Using pharmacokinetic parameters such as volume transfer constant, extravascular extracellular space, and vascular plasma space, T1-based DCE-MRI can be used to measure microcirculation permeability. As with rCBV, DCE-MRI results for differential diagnosis are not clarified. Some studies have found a higher permeability in PCNSL than in glioblastoma [31].
Differentiating PCNSL from toxoplasmosis on imaging
Primary CNS lymphoma and cerebral toxoplasmosis differ from one another in terms of contrast enhancement dynamics, with primary CNS lymphoma exhibiting delayed enhancement [32]. Toxoplasmosis is usually detected as multiple nodular or ring-enhancing lesions on a contrast-enhanced CT or MRI scan with associated vasogenic edema often disproportionate to the size of the lesions. The basal ganglia and the frontal and parietal lobes are frequent sites of these lesions [33,34]. As a result of its high cellularity, primary CNS lymphoma often exhibits attenuating or hyperattenuating mass lesions during CT examinations. CT or MRI can reveal round or oval homogeneous contrast enhancement and varying levels of edema within the lesions in a multifocal or periventricular distribution following contrast administration [35]. Signal intensity patterns were described in an MRI study as a means of separating cerebral toxoplasmosis from other diseases, including lymphoma. On contrast-enhanced T1-weighted images, the “eccentric target” sign, consisting of the innermost enhancing eccentric core, intermediate hypointense zone, and peripheral hyperintense enhancing rim, indicates cerebral toxoplasmosis when compared with other parenchymal lesions. The "concentric target" sign has been observed in cerebral toxoplasmosis in one-third of cases [36]. On T2-weighted MRI images, concentric zones of hypo intensity and hyperintensity have been identified, but further confirmation is required [37]. Compared with the previously described target sign on contrast-enhanced T1-weighted images, a target sign visualized on T2-weighted or FLAIR images had a hypointense core, an intermediate hyperintense region, and a peripheral hypointense rim. 71% of the patients in the series had either a T1-weighted or a 2-weighted FLAIR target sign that was contrast-enhanced. According to a study involving 13 patients using dynamic susceptibility contrast-enhanced MRI, lymphomas had significantly higher relative cerebral blood volumes (rCBVs) than toxoplasmosis lesions [38]. Lesions resulting from toxoplasmosis had an average rCBV of 0.98, whereas lymphoma lesions had an average rCBV of 2.07. For image-based lesion segmentation, hemorrhage, micro vessels, and necrosis were excluded. The reason for the difference in rCBV is the absence of vasculature in cerebral toxoplasmosis and the hypervascularity in lymphoma foci [39].
Magnetic resonance spectroscopy
MR spectroscopy can be useful for distinguishing toxoplasmosis from lymphoma. Choline levels (a marker of cellular turnover) are typically decreased in toxoplasmosis lesions, whereas they are typically elevated in CNS lymphomas. As a result, this difference is not reliable for distinguishing cerebral toxoplasmosis from primary CNS lymphoma [40]. Both of these conditions can have overlapping characteristics with peripheral enhancement and restricted diffusion.
Biopsy
In primary CNS lymphoma, tissue biopsy remains the gold standard to establish the diagnosis. The preferred method of biopsy is stereotactic serial rotating approach. An open approach with resection has been associated with worse outcomes due to hemorrhage [11]. In 2016, the World Health Organization (WHO) adjusted its classification to incorporate molecular findings into brain tumor diagnosis. Molecular testing is now mandatory and even trumps histological phenotype [41,42]. Even with this additional available testing, diagnosis of primary CNS lymphoma proves difficult. Cells are small and frequently consist of lymphocytes with variable atypical cytology [43]. This is a primary reason for limiting steroids prior to biopsy to enhance diagnostic yield. Genetic analysis has recently transitioned to the important role of the JAK-STAT pathway [44]. Particular emphasis has been placed on evaluation of Jak3 and Stat3 and the associated proinflammatory cascade [45]. Other important pathways identified and actively being investigated include NFkB DNA modification, CDKN2A deletions, B-cell receptor signaling, and mutations in MYD88, L265P and CD79B [44].
Ocular Involvement
Ocular involvement of primary CNS lymphoma in the initial stages are primarily asymptomatic. Intraocular involvement has been shown to occur in 15-25% of patients with primary CNS lymphoma16. The most common symptom observed is decreased visual acuity [46]. Due to the subtle presenting features, a thorough ophthalmologic exam with the use of slit lamp and fundoscopy is recommended but not routinely performed [47]. If exam findings are concerning, vitrectomy is recommended [46]. If vitreous biopsy is inconclusive, a chorioretinal biopsy can be used to exclude malignancy [17,18]. Chorioretinal biopsy can either be done through a transvitreal approach or transscleral approach [19].
Additional Diagnostics and Considerations
Presently, there are no serological studies that are clearly diagnostic for primary CNS lymphoma, although biomarkers are currently being investigated based on the inflammatory pathways highlighted above. As primary CNS lymphoma is associated with late HIV/AIDS illness, testing for HIV/AIDS status and CD4 counts is imperative during diagnostic workup [48,49]. Although a nonspecific marker of rapid cell turnover, elevated serum lactate dehydrogenase is associated with poor prognosis with primary CNS lymphoma [50], but otherwise due to poor specificity, has no diagnostic value.
Cerebrospinal fluid analysis
Cerebrospinal fluid (CSF) analysis is recommended but not required in all instances of primary CNS lymphoma [51]. Routine indices for CSF samples include cell count, protein, and glucose [8]. CSF cell counts and protein are normal in 33-60% of patients with primary CNS lymphoma [9-12]. Additionally, CNS lymphoma may show low CSF glucose (<73>2.5 times normal), neoplastic, lymphoid cells [8-14].
CSF evaluation is more pertinent in cases of leptomeningeal involvement or where biopsy is not feasible. Of note, baseline diagnostic imaging should be performed prior to performing lumbar puncture to rule out risk of herniation and to prevent induction of seeding if dural enhancement noted [52]. Recommended studies include CSF protein, glucose, and a combination of both flow cytometry and cytology. CSF protein counts are commonly elevated whereas CSF glucose counts are noted to be decreased [50-53]. Individually, flow cytometry and cytology have poor sensitivity and specificity as lymphocytes can rarely be detected in CSF. To increase sensitivity, it is advised to combine cytology and flow cytometry and to collect more than 10.5 cc of CSF for flow cytometry alone [51-54]. When diagnostic uncertainty exists in patients with HIV/AIDS, Epstein Barr virus polymerase-chain reaction (PCR) may also prove helpful as it has a higher sensitivity and is commonly associated with primary CNS lymphoma in immunocompromised populations [23,48,55]. Emerging research has unveiled new CSF biomarkers that could accelerate diagnosis and reduce risks associated with biopsy. These CSF biomarkers include: A proliferation-inducing ligand (APRIL), B cell activating factor (BAFF), transmembrane activator and soluble CAML interaction (s-TACI), soluble B-cell maturation antigen (s-BCMA), and interleukin-10 [50-56]. Although these biomarkers show promise, further investigation with independent cohorts is needed before routine testing for diagnosis can be established.
Evaluation of systemic disease
To exclude the presence of systemic involvement, bone marrow aspiration and systemic imaging should be performed [51,60]. Bone marrow aspiration is not necessary for disease diagnosis in every case as the likelihood for positive marrow aspirate result is low [60]. Another alternative is CT Chest, Abdomen, and Pelvis or PET-CT Whole Body for staging purposes to assess systemic spread [61]. These studies can miss spread to the testes however and groups have argued that testicular ultrasound should be performed in men greater than 60 years old as well [49]. As testicular involvement is rare, having a cut off of age 60 increases diagnostic yield [62].
Role of corticosteroids in PCNSL management
In the acute stages of establishing diagnosis, as alluded to above, it is critical to avoid corticosteroids. If they had already been started by a provider not familiar with lymphoma workup, taper down to the lowest dose possible as quickly as possible. Exposure to corticosteroids causes cytolysis within lymphocytes and has been reported to negatively impact accurate tissue biopsy and flow cytometry of both vitreous aspirate and CSF [63]. In addition, it can also decrease contrast enhancement of the lesions on MRI [59,63].
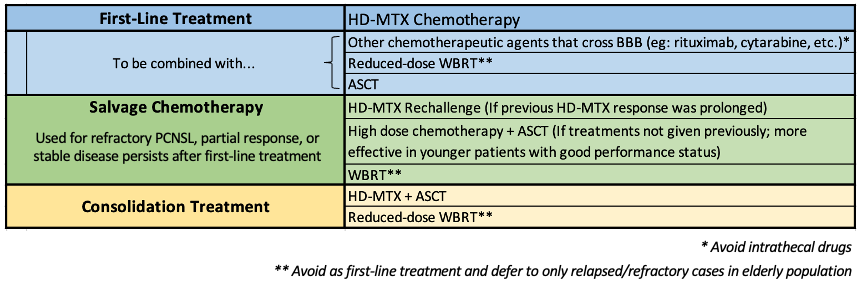
High dose methotrexate as first-line chemotherapy
For newly diagnosed PCNSL, induction chemotherapy is generally used to achieve a complete radiographic response (CR), which is then followed by consolidation therapy with the goal of eliminating residual disease and prolonging OS. There are several methods of medical management that still need further evaluation via prospective trials. However, the current first-line treatment (Table 1) standard is HDMTX-based induction chemotherapy [12,24]. Methotrexate is an antifolate and antimetabolite, which is now considered to be the single most beneficial agent that crosses the BBB and yields cytotoxic levels in CSF [65]. However, there is no consensus on the optimal dose, schedule, or chemotherapy combination. HDMTX is typically given via intravenous infusions at doses ranging from 3-8 g/m2 and for 10 days to no more than 2 to 3 weeks 65,66. Overall, response rates ranged from 35% to 74%, with median progression-free survival (PFS) of 10 to 12.8 months, and median OS of 25 to 55 months with HDMTX treatment [66-69].
Alternative chemotherapeutic combinations
Chemotherapeutic agents should include those known to cross the BBB [65]. Some prominent examples include cytarabine, temozolomide, rituximab, procarbazine, thiotepa, vincristine, carmustine, etoposide, ifosfamide, and cyclophosphamide [12]. Combo therapy of cytarabine and HDMTX showed an improved CR rate, 3-year PFS, and 3-year OS compared to HDMTX alone [70]. Rituximab alone or in a combination regimen is still being tested in clinical trials [12,65]. It does have some limitations in terms of penetrating the BBB due to its large size, and thus is thought to be more effective early in treatment due to BBB breakdown within tumors [65]. However, HDMTX and rituximab combo therapy has been shown to improve CR and OS rate in newly diagnosed PCNSL in retrospective studies [71-73]. Furthermore, intrathecal chemotherapy has not been prospectively studied. Retrospective studies also did not demonstrate any additional benefit from adding intrathecal drugs in patients treated with 3 g/m2 HDMTX [74-76]. Thus, it’s efficacy in PCNSL treatment is not clear and not currently advised as prophylaxis [65]. The paucity in evidence will require more investigation as to the efficacy of intrathecal chemotherapy. Lastly, another option is to add autologous stem cell transplantation (ASCT) or reduced-dose whole brain radiotherapy (WBRT) with first-line HDMTX.
Radiotherapy
Transitioning to the use of radiotherapy, it is important to note that the microscopically diffuse nature of PCNSL makes radiotherapy less effective than HDMTX as a standalone therapy [65]. One phase II clinical trial resulted in only an 11.6-month OS after a total dose of 40 Gy (with an additional 20 Gy to boost contrast enhancing lesions) [67]. In addition to inadequately controlling the progression of PCNSL, WBRT also leads to delayed neurotoxicity. This presents as white matter abnormalities, ventricular enlargement, and cortical atrophy on MRI. These neurocognitive deficits are particularly severe in the elderly [12,78]. A significant decline in the Karnofsky Performance Status Scale (20-50 points) with a marked reduction in quality of life has been observed in several studies following WBRT, especially in elderly populations [78,79]. While the mechanism of neurotoxicity is unclear, leading hypotheses include potential toxicity to vasculature, demyelination, or depletion of neural progenitor cells from the subventricular zone [80-82]. WBRT neurotoxicity is irreversible and is not used for newly diagnosed PCNSL. Thus, the consensus is to avoid WBRT as a standalone therapy, especially in elderly populations due to its delayed neurotoxic effects [65]. Reduced-dose WBRT in combination with HDMTX as first line therapy can be used in younger patients [12,64]. While the optimal dose has not yet been agreed upon, doses of 23–50 Gy to the whole brain, with or without a tumor bed boost, are currently used, with most protocols delivering a total dose of [40-45] Gy without boost, and standard fractionation (1.8-2 Gy/fraction) [65].
Autologous Stem Cell Transplantation (ASCT)
Another modality is high dose chemotherapy with ASCT (HDC/ASCT). Similar to radiotherapy, further investigation is needed to see if HDC/ASCT can be used as a first-line consolidation treatment for PCNSL. However, HDC/ASCT is an efficacious treatment in relapsed or refractory PCNSL, especially as salvage treatment in elderly patients [64,65]. In summary, while HDMTX is the agreed upon first line treatment for newly diagnosed PCNSL, it is recommended to use it in combination with other chemotherapeutic agents and possibly reduced-dose WBRT or ASCT, as these combinations show more disease control with less neurotoxicity as compared to WBRT alone [12].
Management considerations in elderly population
The previous discussions primarily focused on newly diagnosed PCNSL in younger populations. Best treatment protocols for elderly populations and refractory/relapsed PCNSL will now be explored. More than half of all PCNSL cases is in patients greater than 60 years old, making age itself a poor prognostic factor. Thus, it is important to avoid or at least defer WBRT until relapsed PCNSL due to the higher risk of neurotoxicity in elderly patients. Instead, HDMTX combination chemotherapy is considered the first-line treatment [12]. Unfortunately, more than half of HD-MTX responders’ relapse with very poor prognosis, proving the need for regular neuroimaging after initial treatment [12]. One retrospective study showed the median OS was 2 months for primary refractory patients and 3.7 months for patients who relapsed within the first year of the initial therapy [83].
Salvage therapy and novel chemotherapeutic agents
There is no clear data on a single optimal protocol for salvage treatments. Salvage treatments (Table 1) depend highly on a patient’s individual prognostic factors such as their age, previous treatments (and their responses), and comorbidities at the time of relapse [12]. Similar conclusions arise, however, in that monotherapies seem to be ineffective in relapsed/refractory disease, similar to newly diagnosed PCNSL. For example, when evaluating rituximab’s efficacy as a monotherapy (up to 8 weekly doses of 375 mg/m2) in a single study of 12 patients with refractory or relapsed PCNSL, results showed responses detected via MRI in 36% of patients [65,84]. One option is to use HDMTX again if the patient previously showed a prolonged response to it. Evidence for this lies in retrospective studies, reporting response rates between 85% and 91% and median OS times of 41-62 months [85,86]. In younger patients with good performance status who did not receive high-dose chemotherapy or prior ASCT, an alternative option is to use ASCT. This seems to be more effective in younger patients who had more chemo-sensitive disease [87]. Lastly, there are several agents being investigated. Some target PD-1 based on observed PD-1 activity in other lymphomas while others are Bruton’s tyrosine kinase (BTK) inhibitors. A few examples include nivolumab and ibrutinib among several others [87,89].
Recent advancements in clinical trials
Despite high relapse rates and associated neurotoxicity of treatment modalities, recent clinical trials have shown promising advancements in the treatment of this aggressive disease. Frigault et al. demonstrated the safety and efficacy of tisagenlecleucel (CD19-directed chimerical antigen receptor T-cell product) in patients with refractory PCNSL [13]. Other recent clinical trials have highlighted the safety and prospective optimal use of chemotherapeutic agents such as thiotepa [90], temozolomide [91], and pemetrexed [92] in the treatment of PCNSL [93-96]. Furthermore, innovative solutions to tackling difficulties in crossing the blood-brain barrier have been highlighted in recent studies. R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) is the mainstay of treatment in systemic diffuse large B cell lymphoma. It has not been utilized in the treatment of PCNSL due to difficulties with these agents in crossing the blood-brain barrier. Ferreri et al. recently showed that administration of R-CHOP preceded by NGR-hTNF (tumor necrosis-a coupled with the CD13+ vessel targeting peptide, NGR) showed promising responses and a better ability of these agents to enter the CNS, highlighting the potential of an expanded chemotherapeutic arsenal against PCNSL [97,98].
Surgical resection of lesion
Historically, surgical resection of lymphoma has been associated with worse outcomes [11,99] However, more recent studies of biopsy with surgical resection have pointed to lower complication rates and improved survival [100-102]. This may be credited to the development of improved imaging modalities and neurosurgical equipment as well as the use of adjuvant radiotherapy and methotrexate/R-CHOP therapy [103].
Role of Ommaya Reservoir as a diagnostic and therapeutic tool
Prophylactic intrathecal chemotherapy can be administered to reduce CNS relapse. Intrathecal chemotherapy has historically been administered via lumbar puncture in the lumbosacral cerebrospinal fluid (CSF) space [104]. The Ommaya reservoir is a device that sits between the cranium and the skin with a catheter extending into one of the lateral ventricles [105]. This site can be used to sample CSF and as an intrathecal chemotherapy delivery point [104].
There are many advantages to the Ommaya reservoir (Figure 2) over lumbar puncture. First, Ommaya reservoirs deliver chemotherapeutics directly to the cerebral area rather than relying on CSF circulation from the lumbar region. Secondly, lumbar puncture can be a challenging procedure in patients with spinal deformities and obesity [104] Ommaya reservoirs have the advantage of being very efficient and simple to use when compared to repeated lumbar punctures [104] One study on children receiving chemotherapy through both the lumbosacral route and the intraventricular route (Ommaya reservoir) found that the patients strongly preferred the Ommaya device to repeated lumbar puncture [106].
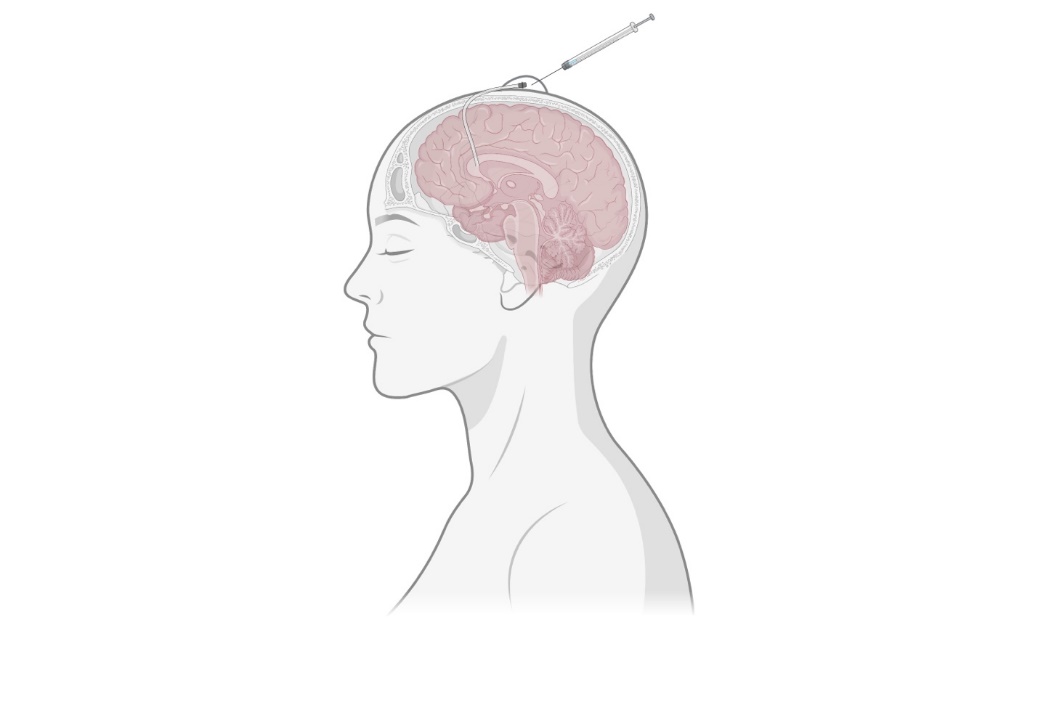
Potential complications associated with the use of the Ommaya reservoir include bacterial infection and catheter misplacement [104]. Bacterial CNS infection associated with Ommaya reservoir placement is quite rare at 1-5.5% [107,108]. Catheter misplacement into the brain parenchyma used to be much more common. Ommaya catheter placement into the parenchyma could lead to focal leukoencephalopathy [104]. However, advancements in imaging and neurosurgical technology have led to a significant reduction in this complication.
PCNSL represents a rare and aggressive disease with poor prognosis. While it is most commonly diagnosed in the immunocompetent patient, studies have shown an increasing incidence of this diagnosis in the elderly population. Diagnosis revolves around initial imaging followed by stereotactic biopsy. In comparison to other primary CNS lesions, resection is generally not recommended, although there is limited evidence showing benefit given advances in neurosurgical technology and technique. Despite a generally favorable response to first line therapy with high dose methotrexate, PCNSL has a high relapse/refractory disease rate which is associated with a worse prognosis. Although much of the current literature regarding management is limited to retrospective studies, recent clinical trials are showing promise and an expanded arsenal of therapeutic agents ranging from immunotherapy to agents that increase permeability of the blood-brain barrier. This is especially important given that there is a host of chemotherapy drugs such as R-CHOP that have been proven effective in systemic disease. Further studies will need to be conducted to better assess the efficacy and safety profile of these emerging regimens.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti