AUCTORES
Globalize your Research
Review Article | DOI: https://doi.org/10.31579/2693-4779/208
1. Associate Professor SDM Institute of Nursing Sciences,Shri Dharmasthala Manjunatheshwara University, Sattur, Dharwad, Karnataka.
*Corresponding Author: Rangappa Ashi, Associate Professor SDM Institute of Nursing Sciences,Shri Dharmasthala Manjunatheshwara University, Sattur, Dharwad, Karnataka.
Citation: Praveen B. Katti, Poonam, Rangappa.S. Ashi, (2024), Advancements in Patient Care and Safety: Integrating Nursing Innovations for Enhanced Healthcare Outcomes, Clinical Research and Clinical Trials, 10(3); DOI:10.31579/2693-4779/208
Copyright: © 2024, Rangappa Ashi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 08 May 2024 | Accepted: 25 June 2024 | Published: 07 August 2024
Keywords: hand haptic; haptic sleeve; hill type model; human-robot interface (hri); intent signal
In the realm of virtual environments, hand haptic technology plays a crucial role in capturing the nuanced movements of a user’s hands and fingers. This is complemented by a haptic sleeve that bridges the gap between the arm and hand, effectively translating these movements into corresponding actions performed by a robot avatar within the virtual space. Furthermore, these innovative devices are adept at relaying the force and texture felt by the robot avatar as it interacts with objects in the virtual environment back to the user. This interaction crafts an immersive experience, mirroring the sensation of physically touching and manipulating the objects. The prediction of wearer's joint torques uses the Hill-type model and is made through the flexion movement of the elbow joint.
As the user engages in object manipulation through the robot avatar, the haptic feedback disseminates throughout the entire arm, enriching the user experience with a wide spectrum of tactile sensations. This advancement in haptic technology significantly enhances the realism of robot operation, thereby improving the dynamics of human-robot interaction.
In A New Health System for the 21st Century, the Patient safety and patient care is a fundamental activity and responsibility of an organized work or activities of health care professionals that create cultures, processes, procedures and environments in health care that consistently and sustainably lower risks, reduces the occurrences of avoidable harm, make error less likely and reduce its impact when it does occur. Presently, patient centered care involves the sharing of information with patients, family and health care team with patients needs (including physical, psychosocial, and occupational and management of waste equipments during care, procedure and transport of patient.) Beliefs and expectations.
The Culture of Quality and Safety
In 1999, The Institute of Medicine released a sobering report titled To Err is Human: Building a Safer Health System, which stated that an estimated 98,000 hospitalized patients die each year from medical mistakes. The report was not intended to blame providers or hospitals but, rather, to clarify those bad systems of care (and not bad people) were largely responsible for these deadly mistakes. Furthermore, the report hoped to rally health care providers, administrators, regulators, and patients around a national imperative toward creating a culture of safety and developing systems of care to improve health care quality. In a subsequent report, A New Health System for the 21st Century, the health care system has many great successes, but there continue to be opportunities for improving quality, access, and cost. The fee-for-service health care paradigm is shifting toward value-based care and will require accountability around quality assurance and cost reduction. As a result, many health care entities are rallying health care providers, administrators, regulators, and patients around a national imperative to create a culture of safety and develop systems of care to improve health care quality. However, the culture of patient safety and quality of care requires rigorous assessment of outcomes, and while numerous data collection and decision support tools are available to assist in quality assessment and performance improvement, the public reporting of this data can be confusing to patients and physicians alike and result in unintended negative consequences. This article explores the aims of health care reform, the new ideas of AI (artificial intelligence) efforts to create a culture of quality and safety, the principles of innovative in care and quality improvement, and how these ideas can be applied to patient care and medical practice.
Patient care: it’s a type of model in which fully involvement of expertise in health care to identify, satisfy the full range of patients and family’s needs, and preferences.
Or
A model of prevention, treatment and management of illness and preservation of physical and mental well-being through the services offered by the health care team.
Patient safety: a type of process or structure whose application reduces the probability of adverse event, unsafe acts within the health care system, through the best practices lead to optimal patient outcomes.
Method of Presentation
six aims for health care reform:
First, health care must be safe. “Primum non nocere” (first do no harm) should no longer be the sole burden of individual providers. Instead, hospitals must be held accountable for maintaining systems of care that ensure patient safety.
Second, health care should be effective. Health care providers must use evidence-based medicine and evidence-based practice. Since the best science and clinical practices in medicine continue to evolve, every practitioner should be expected to participate in life-long learning through continuing medical education to remain up to date. Reliance on tradition and anecdotal personal experience should no longer be acceptable practice. The phenomenon of “illusory superiority”—otherwise known as the “Dunning-Kruger effect” (a type of cognitive bias, where people with little expertise or ability assume they have superior expertise or ability. This overestimation occurs as a result of the fact that they don't have enough knowledge to know they don't have enough knowledge.) Highlights that poor performer often lack the skills and knowledge to identify their own poor performance.
Third, care should be patient centered. “For the secret of the care of the patient is in the caring for the patient.” High-quality care needs to be respectful of the patient's values and receptive to the patient's input. All care decisions and therapeutic plans—including the rationale, risks, costs, and benefits—should be proactively explained to the patient. The “best possible outcome” is optimally decided through shared decision making by a highly competent care team and a well-informed patient.
Fourth and fifth, care should be timely and efficient. Unnecessary delays and prolonged waiting times can be frustrating and dangerous for patients depending on their underlying medical conditions. In addition to caring for their patients' welfare, all care providers should be good stewards of valuable health care resources. After an attentive patient evaluation, any blood tests, diagnostic imaging, and invasive procedures should be tailored to confirm or refute the provider's differential diagnosis specific for that individual patient. Whenever possible, decisions and plans should avoid wasting valuable equipment and precious time.
Lastly and arguably most importantly, care must be equitable. The quality of care should not vary based on a patient's personal characteristics, gender, race, religion, geography, or socioeconomic status. Every person across the country should have access to high-quality value-based care.
1) patient identification
PPID Tip #1: Use two forms of identification: Always use at least two separate methods of identifying a patient, such as the patient’s name and date of birth. Do not use patient room number as an identifier.
PPID Tip #2: Involve the patient: Ask patients to identify themselves before receiving medication or treatment and encourage patients to participate in all stages of the process. If possible, ask patients or family members to verify identifying information to ensure its accuracy.
PPID Tip #3: Listen for questions: If a patient or family asks a question or expresses confusion about something related to patient identification, stop and listen. This may be the warning you need to prevent an error.
PPID Tip #4: Ask, don’t confirm: Use specific language to ask a patient to identify themselves. Do not ask them to confirm their name. Instead say, “Please tell me your name.”
PPID Tip #5: Standardize your methods: If you are part of a multi-facility healthcare organization, take steps to standardize your approach to patient identification among all of the facilities within the system. For example, standardize how names are displayed in electronic health records. Then, audit your policies and processes regularly to discover any potential system-wide risks.
PPID Tip #6: Have a plan for no name, same name: Provide clear protocols to staff members for identifying patients who lack identification, and for distinguishing the identity of patients with the same name.
PPID Tip #7: Snap a photo: Update your protocols to include patient photos, such as on patient wristbands. The use of patient photos is still in the minority among hospitals but it’s a powerful defense against patient identification errors.
PPID Tip #8: Don’t leave without labeling: Always label blood and other specimens in the presence of the patient. It’s too easy to forget which label goes with which specimen.
PPID Tip #9: Pay attention to your little voice: Establish clear protocols for questioning test results or findings when they are not consistent with the patient’s clinical history. If something doesn’t look right, it probably isn’t.
PPID Tip #10: Get it right from the start: Create clearly defined policies and procedures for the registration process to prevent patient registration errors from affecting care later in the visit. Devote adequate staffing resources to the registration team so they don’t feel rushed, which is often a source of errors.
PPID Tip #11: Embrace digital technology: Implement automated healthcare technology systems –
PPID Tip #12: Discuss and learn: Foster a culture where patient identification errors can be called out and discussed without fear of retribution. Every error offers an opportunity for learning and improvement.
Everyone has their own way of coping with pain and finding hope in times of distress. When walking through a health crisis, many turn to spirituality for comfort, and many people find their spiritual center in religion. The World Religion Database counts 18 major religious categories around the world. Scholars estimate that about 2,400 religions exist in total. Many peoples’ identities are informed by their race, culture, ethnicity, gender, or religion. When it comes to receiving medical care, many patients will make decisions based on their identity in some or all of these categories.
Religion provides resources for coping with stress that may increase the frequency of positive emotions and reduce the likelihood that stress will result in emotional disorders such as depression, anxiety disorder, suicide, and substance abuse. The major problems such as Birth control, abortion, Autopsy and organ donation, Euthanasia and Death associated problems can be resolved.
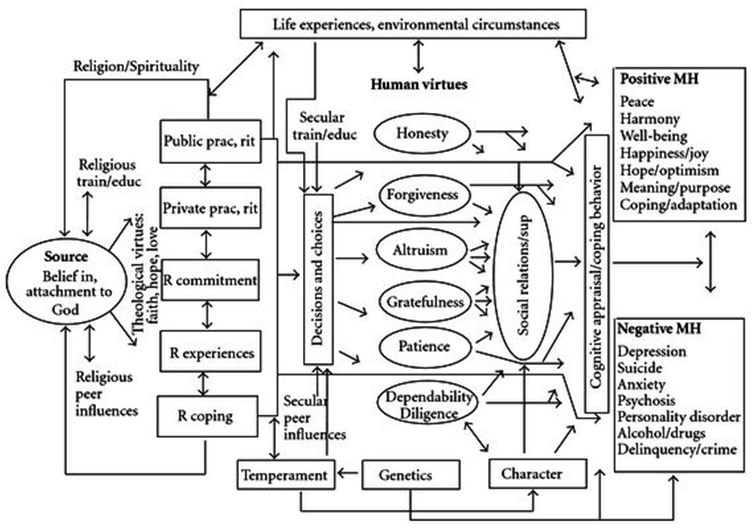
Figure 1: from ncib.nlm.nih.com
3) Patient Centered Care
Patient-centered care focuses on the patient and the individual's particular health care needs. The goal of patient-centered health care is to empower patients to become active participants in their care.
Person-centered care affording people dignity, compassion and respect. Offering coordinated care, support or treatment. Offering personalized care, support or treatment. Supporting people to recognize and develop their own strengths and abilities to enable them to live an independent and fulfilling life.
Figure 2: https://images.app.goo.gl/7TdrDucat5wKtjJGA
Benefits of Patient-Centered Care
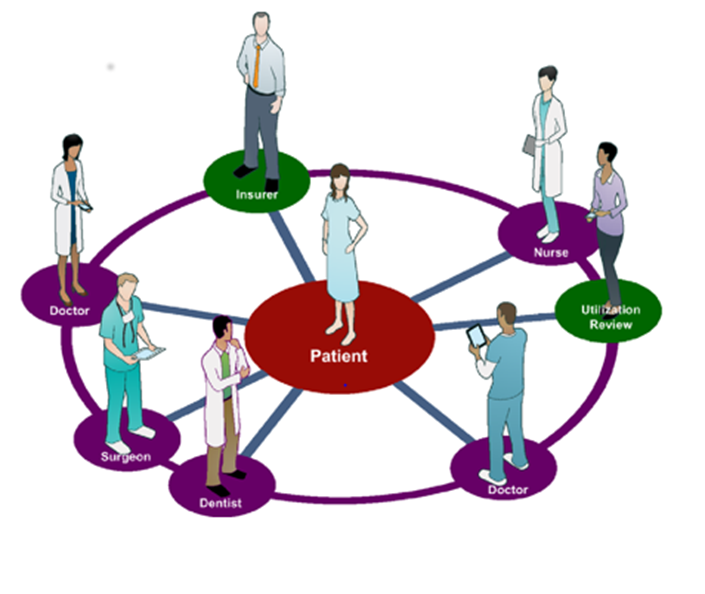
Figure 3
Ai Assisted Drone
Artificial Intelligence-based devices assist researchers to broaden the levels of identification, detection, and delivery services. Generative AI in healthcare is a rapidly evolving field, encompassing the use of AI to generate realistic data, such as synthetic medical images, to train algorithms and accelerate research. This innovative technology not only creates synthetic data but also plays a pivotal role in transforming diagnostics. In fact, it brings about a level of precision that was once unimaginable. Moreover, healthcare professionals, armed with the capability to analyze vast datasets, are now empowered to achieve early detection and more accurate diagnosis of medical conditions. Drones provide efficient diagnostics, detections, and supervision in aerial cases through high-performance built-in computers, thermal scanners, high-resolution cameras, and other tools.
We can use the AI drones in highly risk of accident regions, floods and other natural disasters, high altitude regions, in forest area to rescue of highly vulnerable children’s, old women and old age peoples and pregnant women. Also, in the more populated areas where high risk of accidents are occurs, there we have to activates it and control the area. Which involves travelling in that area every 2 hours, if anything happens related to health which have basic information such as identification of type and basic needs of patients and nearby health services centers and emergency CPR and resuscitation services by using surrounded peoples of incident.
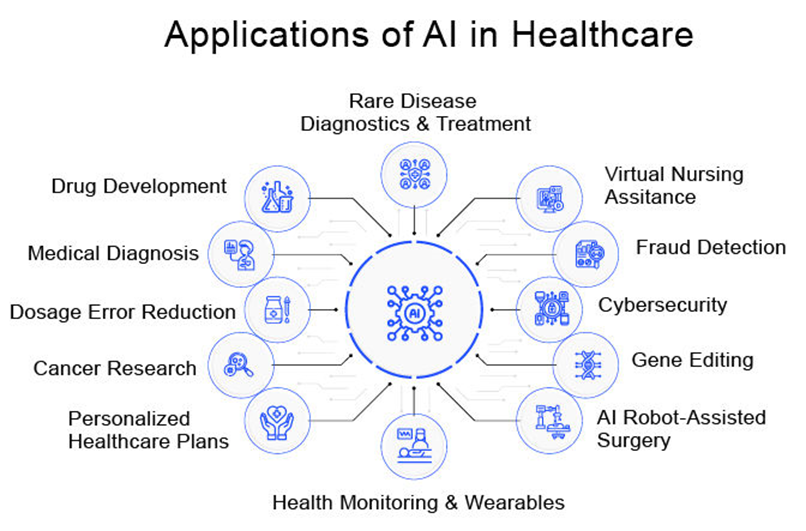
Figure 4: https://www.delveinsight.com
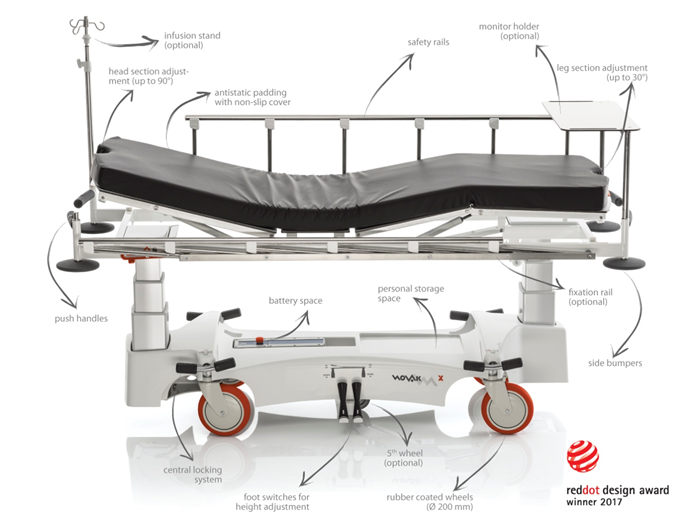
Smart Strechers
I. Integration of Gps and Tracking Systems for Enhanced Safety
A. Explanation of how GPS integration enhances the safety of rescue operations.
B. Benefits of real-time tracking and location data for responders.
Real-time tracking is a pivotal feature enabled by GPS integration. It allows incident commanders and rescue teams to monitor the precise location of stretchers and their occupants in real-time. This level of visibility enhances situational awareness, enabling responders to make informed decisions swiftly. Furthermore, it aids in the coordination of multiple teams operating in a rescue scenario, promoting efficient resource allocation and teamwork.
C. Technical details of GPS and tracking system integration.
The technical underpinnings of GPS integration in rescue stretchers involve the utilization of satellite signals to triangulate the stretcher's position. These systems typically consist of GPS receivers, which communicate with satellites, and onboard software for data processing. The collected data, including latitude, longitude, altitude, and timestamp, is transmitted to a central monitoring station via secure channels. Encryption and authentication measures are often employed to safeguard the integrity and privacy of this critical information.
II. Incorporating Telematics for Remote Monitoring and Communication
Telematics technology has become a crucial component in the realm of rescue stretcher innovation. By seamlessly integrating telematics systems, these stretchers are now equipped with advanced capabilities that significantly enhance their effectiveness in emergency situations. In this section, we will delve into the key aspects of telematics technology and how it revolutionizes rescue stretcher functionality.
A. Overview of Telematics Technology and Its Relevance to Rescue Stretchers
B. How Telematics Enables Remote Monitoring of Vital Signs and Conditions
C. Communication Features and Their Impact on Coordination During Rescues
III. Foldable and Compact Designs for Easy Storage and Transport
Another significant innovation in rescue stretcher technology is the development of foldable and compact designs. These designs have transformed the way rescue stretchers are stored, transported, and deployed in emergency situations.
A. Importance of Compact Design in Rescue Stretcher Technology
B. Advantages of Foldable and Portable Stretcher Models
C. Considerations for Storage and Transportation in Rescue Operations
IV. Advances in Materials for Improved Durability and Weight Reduction
A. Discussion on the Role of Materials in Rescue Stretcher Innovation
In the realm of rescue stretcher technology, the choice of materials plays a pivotal role in determining the effectiveness and reliability of these critical life-saving devices. Over the years, advancements in materials science have led to significant improvements in both durability and weight reduction. In this section, we delve into the critical role that materials play in the innovation of rescue stretchers.
Materials are the building blocks of any rescue stretcher. The choice of materials impacts not only the overall strength and longevity of the stretcher but also its weight and portability. In high-stress rescue scenarios, the reliability of the stretcher is paramount, making material selection a primary consideration.
The rigors of rescue operations demand that stretchers withstand harsh environmental conditions and rough handling. Traditionally, stretchers were constructed using materials like steel, which offered exceptional durability but came with a substantial weight penalty. However, modern materials have opened up new possibilities for balancing durability and weight.
B. Benefits of Lightweight Materials for Ease of Handling
Lightweight materials have revolutionized the world of rescue stretchers, making them significantly more maneuverable and user-friendly. This section outlines the advantages of employing lightweight materials in stretcher design.
C. Examples of Cutting-Edge Materials Used in Modern Stretcher Construction
To illustrate the practical application of advanced materials in modern rescue stretcher technology, let's explore some examples of cutting-edge materials that have been integrated into the construction of these vital tools.
V. Emerging Trends in Rescue Stretcher Designs and Features
A. Exploration of Recent Trends Shaping the Future of Rescue Stretcher Technology
In an ever-evolving field like rescue stretcher technology, staying abreast of emerging trends is crucial. This section explores the latest developments that are shaping the future landscape of rescue stretcher design and features.
B. Analysis of Innovative Features Such as Adjustable Configurations and Ergonomic Design
In this subsection, we take a closer look at two innovative features—adjustable configurations and ergonomic design—that are gaining traction in the field of rescue stretcher technology.
C. Considerations for Adapting to Evolving Rescue Scenarios and Needs
As rescue scenarios evolve and become increasingly complex, stretcher technology must adapt accordingly. This subsection outlines key considerations for manufacturers and responders alike to ensure that stretcher designs meet the evolving demands of modern rescue operations.
new innovative idea of patient transport 1
Ambulance
al-time tracking and GPS systems: play a crucial role in improving ambulance service efficiency. By equipping ambulances with GPS devices, emergency response teams can accurately track and monitor their location. This enables efficient dispatching, as the nearest available ambulance can be assigned to a particular emergency. Real-time tracking also helps in avoiding traffic congestion by redirecting ambulances to less congested routes, saving valuable time during emergencies.
Mobile applications: can serve as powerful tools for streamlined communication and coordination in ambulance services. Through dedicated ambulance service apps, dispatch centers can easily receive emergency calls, locate nearby available ambulances and assign them to emergencies promptly. These apps can also provide essential information to paramedics en-route, such as the patient's medical history, allergies and any pre-existing conditions. Efficient communication and data exchange through mobile apps enhance the overall quality of care provided during transportation.
Integration of telemedicine and remote medical support: can significantly enhance ambulance services in India. Telemedicine allows medical professionals to remotely assess patients' conditions, provide initial guidance to paramedics and make critical decisions before they reach the hospital. This real-time consultation reduces the risk of misdiagnosis and helps in delivering appropriate care during transportation. Additionally, remote medical support can facilitate communication between paramedics and specialized medical experts, ensuring optimal care for patients with complex medical needs.
Emerging technologies such as drones: can play a vital role in emergency medical transport. Drones equipped with medical supplies and equipment can swiftly reach remote or inaccessible areas, delivering necessary aid before an ambulance arrives. These drones can also provide real-time video streaming, allowing medical professionals to assess the situation and guide on-site responders. Integrating drones into the ambulance service infrastructure can significantly reduce response time and save lives, especially in hard-to-reach regions.
Electronic Health Records (EHR): it has the potential to revolutionize patient information management in ambulance services. By adopting EHR systems, paramedics can have instant access to a patient's medical history, allergies and prescribed medications. This information enables them to provide appropriate treatment and medication during transportation, enhancing patient safety. Seamless data transfer between ambulances and hospitals through EHR systems improves continuity of care and reduces the risk of errors or duplicated medical tests.
Overcoming Infrastructure Limitations: While technology offers immense potential, it is essential to address infrastructure limitations to ensure its effective implementation. Connectivity issues in remote areas need to be resolved to enable real-time communication and tracking. Governments and stakeholders should invest in improving internet connectivity and mobile network coverage, particularly in underserved regions. Additionally, establishing robust communication networks dedicated to emergency services can facilitate efficient communication between dispatch centers, ambulances and hospitals.
Collaboration with Stakeholders: Improving ambulance services with technology requires collaboration among various stakeholders. Governments should take the lead in promoting technology adoption by initiating partnerships with healthcare providers, technology companies and non-governmental organizations (NGOs). Such collaborations can facilitate the development of comprehensive technological solutions and encourage knowledge sharing. Engaging the community through awareness campaigns can generate support and participation, fostering a sense of responsibility towards emergency medical services.
Training and Skill Development: To effectively leverage technology, it is crucial to train ambulance staff in its proper usage. Training programs should focus on equipping paramedics with the skills to utilize technology effectively and efficiently. Special emphasis should be placed on the operation of GPS systems, mobile applications, telemedicine platforms and electronic health record systems. By ensuring that ambulance staffs are trained in utilizing these tools, the overall quality of emergency medical services can be significantly enhanced.
Future Prospects and Recommendations: The future of ambulance services in India holds immense potential with emerging technologies such as artificial intelligence (AI) and Internet of Things (IoT). AI-powered algorithms can help predict emergency hotspots, optimize ambulance routing and provide real-time traffic updates to ambulance crews. Integration of IoT devices can enable seamless communication between ambulances, hospitals and traffic management systems, ensuring a coordinated and efficient response.

New ambulance works as semi hospital 1
Safety In Diagnosis, Treatement and Surgery
Ai Assisted Emergency Medicine
If we fail to address the urgent matters, serious consequences will emerge. That’s what we call as emergencies. On theme of “DAY OR NIGHT WE DO IT RIGHT”.AI assisted, enhanced care and treatment to better fight for the lives of those we care, cure. And also, to eliminate the suffering of those we can’t.
Innovation Are
Robotic Surgery
It is one which are creator of efficiency, removing the barrier of time and effort. Robotic surgery is a method to perform surgery using very small tools attached to a robotic arm. The surgeon controls the robotic arm with a computer. Robotic surgery is similar to laparoscopic surgery. It can be performed through smaller cuts than open surgery. Robotic surgery may be used for a number of different procedures, including: Coronary artery bypass, cutting away cancer tissue from sensitive parts of the body such as blood vessels, nerves, or important body organs, Gallbladder removal, Hip replacement, Hysterectomy, Total or partial kidney removal, Kidney transplant, Mitral valve repair, Pyeloplasty (surgery to correct ureteropelvic junction obstruction), Pyloroplasty, Radical prostatectomy, Radical cystectomy, Tubal ligation etc.
To operate using the Robotic system, your surgeon makes tiny incisions in your body and inserts miniaturized instruments and a high-definition three-dimensional camera, and sometimes skin incisions are not required at all. Then, from a nearby console, your surgeon manipulates those instruments to perform the operation. Which works on without man power, protects from rays and harmful radiation protection shield. Which also have validation, up to date diagnostic pattern, and evaluate and analyzing the surgery procedure. Minimally invasive are just two fancy words that mean smaller incisions. These types of surgeries mean shorter hospitalization and faster recovery for patients.
Other benefits may be:
Educational Programme
“Prepare and prevent instead of repair and repent.”
Concepts in accident prevention
Primary prevention: removal of circumstances causing injury - e.g., traffic speed reduction, fitting stair gates for young children, reducing alcohol consumption.
Secondary prevention: reduces severity of injury should an accident occur - e.g., use child safety car seats, bicycle helmets, smoke alarms.
Tertiary prevention: optimal treatment and rehabilitation following injuries to minimize long-term consequences - e.g., effective first aid, appropriate hospital care.
Clinical roles for health professionals in accident prevention
These include:
Advice to patients: health workers such as health visitors can sometimes be well placed to identify accident risks or medical conditions conferring risk and to advise accordingly - for example:
Child accident prevention: Identify hazards (e.g., if a family is being seen by a health visitor at home or if treatment is being sought for accidental injury). Advise about prevention - e.g., stair gates, keeping chemicals out of reach, etc.
Patients with medical conditions: Identify and treat accident-causing conditions - e.g., obstructive sleep apnea, visual or balance disorders, Sleep disorder, Diabetes, Epilepsy, Attention deficit hyperactivity disorder (ADHD). Give appropriate advice on fitness to drive. Advise patients on how to minimize accident risks from their medical condition. Identify unacceptable risks and intervene where appropriate - for example: Identify vulnerable children and adults with recurrent injuries or at high risk. This includes those who are experiencing neglect and may require child protection procedures. Consider reporting to the Driver and Vehicle Licensing Agency (DVLA) patients who fail to comply with medical driving regulations.
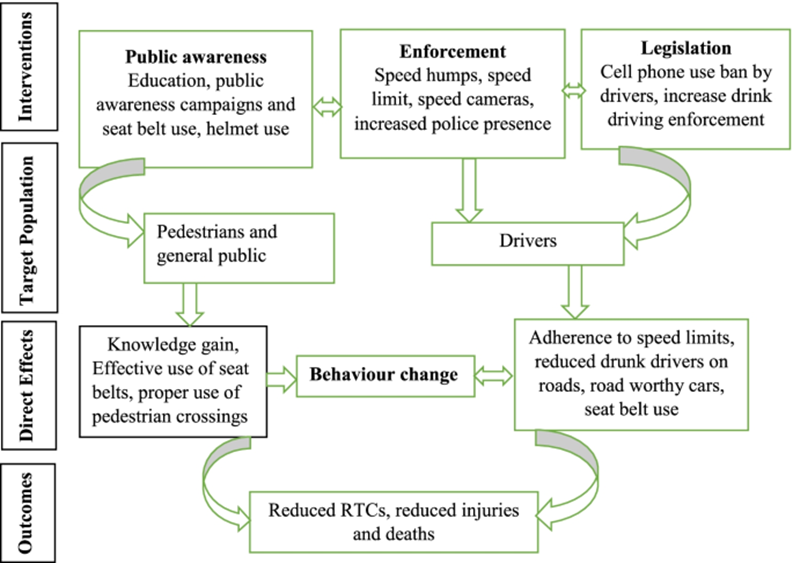
Figure 5: bmcpublichealth.biomedcentral.com
Vaccination
Vaccination is an act of love for ourselves, our families and our communities. We predict that the development of virtually all vaccines licensed from this point forward will involve some form of genetic engineering. Entire viral genomes can now be cloned into bacterial or yeast vectors, allowing manipulation of genes prior to “rescue,” or regeneration of infectious organisms in culture. These techniques enable the rapid custom design of organisms for use in vaccines.
Other Innovation Are

vaccination 1
Crispr Gene Editing
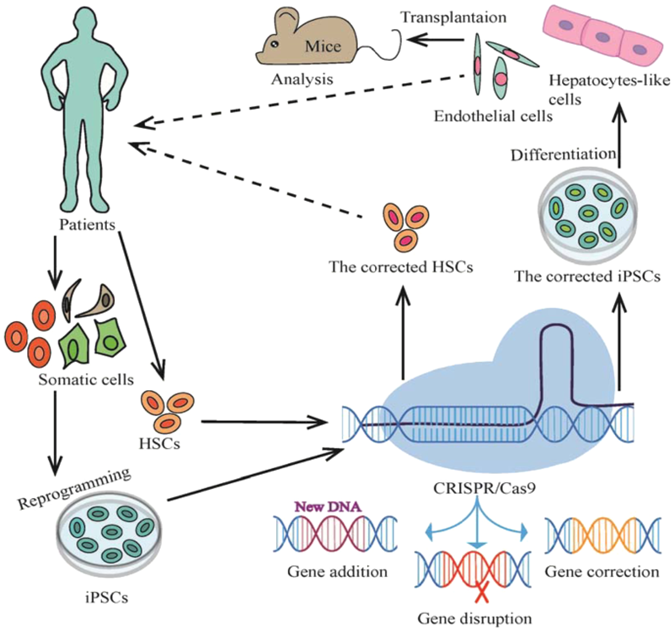
Crispr Technology 1
Smart Bandages
Optimal wound healing requires a delicate balance of various chemical and physical factors and bandages are often used to achieve the stable environment needed for tissue repair. However, the conventional wound coverings used by providers to constantly monitor wound temperature, pressure, and moisture levels are often inefficient. To solve the smart bandages, wound care is now more efficient and effective.
Smart bandages are wound coverings that incorporate technology to help optimize the tissue repair process. Smart bandages function via various sensors which detect, record and regulate physical and chemical factors that affect the rate of wound healing. Smart wound bandages may help wound care experts plan for, prognosticate, and manage acute to chronic wounds of various etiologies more effectively than traditional bandages. The functioning of smart bandages depends on the type of sensors integrated within the bandage material. Smart bandages integrate a thin layer of flexible electronics within the bandage which can detect and interpret thermal changes, oxygen/moisture content, as well as pressure variations at the wound site they overlay.The commonest types of sensors incorporated within smart bandages include: Thermal sensors, Oxygen saturation sensors, Wound pressure sensors, pH sensors, Oxygen Saturation Sensors etc.

Smart bandage image 1
Biomedical Waste Management
“There is no such thing as away when we throw anything away it must go somewhere”
Biomedical waste (BMW) is any waste produced during the diagnosis, treatment, or immunization of human or animal research activities pertaining thereto or in the production or testing of biological or in health camps. It follows the cradle to grave approach which is characterization, quantification, segregation, storage, transport, and treatment of BMW.
Only about 10%–25% of BMW is hazardous, and the remaining 75%–95% is nonhazardous. The hazardous part of the waste presents physical, chemical, and/or microbiological risk to the general population and health-care workers associated with handling, treatment, and disposal of waste.
Innovatives
Plasma Gratification: Plasma, referred to as the "fourth state of matter," is a very high temperature, highly ionized (electrically charged) gas capable of conducting electrical current. Examples of plasma in nature include lightning and gas at the surface of the sun. Plasma technology has a long history of development and has evolved into a valuable tool for engineers and scientists who need to use very high temperatures for new process applications. Man-made plasma is formed by passing an electrical discharge through a gas such as air or oxygen (O2). The interaction of the gas with the electric arc dissociates the gas into electrons and ions, and causes its temperature to increase significantly, often exceeding 6,000°C, nearly as hot as the sun's surface.Plasma gasification is an extreme thermal process using plasma which converts organic matter into a syngas (synthesis gas) which is primarily made up of hydrogen and carbon monoxide.
Advantages:
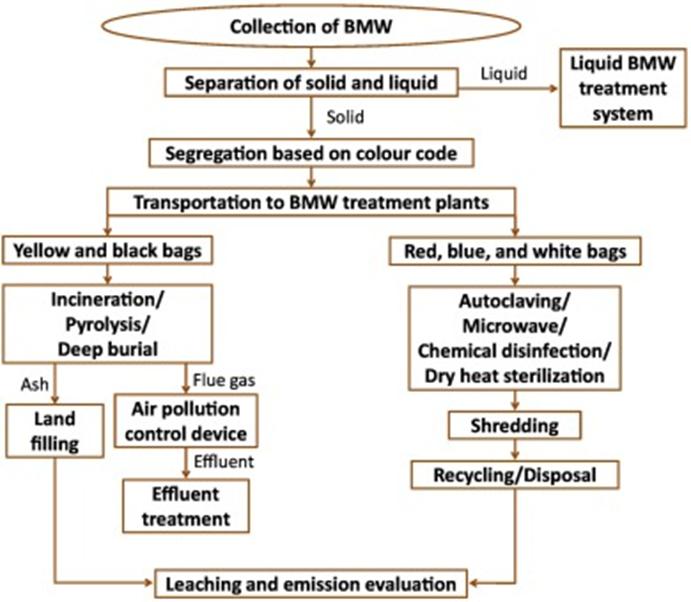
Figure 6
Safety precaution programmers
Tele Medicine
“Make an impact, with no sound of income.”
Telemedicine enables patients to receive medical attention at the convenience of both doctor and him, and at the same time, he is safe. This technology allows people to take blood pressure medicine, refill medications, and recall their appointments and Web-based visits with a doctor or nurse practitioner are another form of interactive appointment. For all scenarios, electronic health technology makes chronic illness control easier by simply placing care monitoring apps and smartphones in the hands of patients. This method is applicable for diagnosis, treatment, prevention, research data evaluation as well in continuing education.
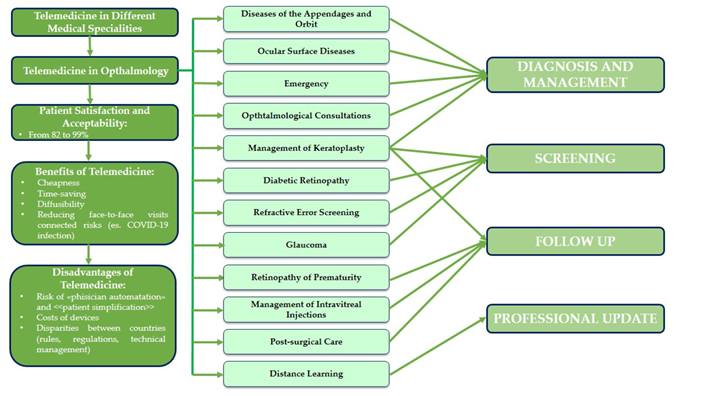
Figure 7: with example in ophthalmological disease
Importance Of Innovation in Health Care
"‘Health innovation’ improves the efficiency, effectiveness, quality, sustainability, safety, and/or affordability of healthcare. This definition includes ‘new or improved’ health policies, practices, systems, products and technologies, services, and delivery methods that result in improved healthcare.” there are three different kinds of innovation that can make health care better:
a) Consumer-focused: Focusing on the way consumers use health care.
b) Technology-based: Developing new products and treatments.
c) Business model: Focus on integrating different healthcare organizations.
The primary aim of Al in healthcare is to analyse relationships between or treatment techniques and patient outcomes. Al can achieve fast and accurate Diagnostics. It will be very helpful to reduce the human errors as well as the cost of treatment. The challenges experienced in health care came as a result of a wrong approach towards the invention of a new technology system. In their attempt to reduce errors, we have to introduced the new system into their existing structure.
The implementation of the new technology took a longer period since it had to be halted to allow changes to be made. The changes would have been easily made in the structure rather than the new system. Which also
helps in Easy access to patient medical records, Reduction in medical errors, Greater patient care, Improved patient education, Reduction in cost etc. We do hope you find this article informative and useful for your studies and practice.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti
Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation. “The peer review process was efficient and constructive, and the editorial office provided excellent communication and support throughout. The journal ensures scientific rigor and high editorial standards, while also offering a smooth and timely publication process. We sincerely appreciate the work of the editorial team in facilitating the dissemination of innovative approaches such as the Bonori Method.” Best regards, Dr. Matteo Bonori.

I recommend without hesitation submitting relevant papers on medical decision making to the International Journal of Clinical Case Reports and Reviews. I am very grateful to the editorial staff. Maria Emerson was a pleasure to communicate with. The time from submission to publication was an extremely short 3 weeks. The editorial staff submitted the paper to three reviewers. Two of the reviewers commented positively on the value of publishing the paper. The editorial staff quickly recognized the third reviewer’s comments as an unjust attempt to reject the paper. I revised the paper as recommended by the first two reviewers.

Dear Maria Emerson, Editorial Coordinator, Journal of Clinical Research and Reports. Thank you for publishing our case report: "Clinical Case of Effective Fetal Stem Cells Treatment in a Patient with Autism Spectrum Disorder" within the "Journal of Clinical Research and Reports" being submitted by the team of EmCell doctors from Kyiv, Ukraine. We much appreciate a professional and transparent peer-review process from Auctores. All research Doctors are so grateful to your Editorial Office and Auctores Publishing support! I amiably wish our article publication maintained a top quality of your International Scientific Journal. My best wishes for a prosperity of the Journal of Clinical Research and Reports. Hope our scientific relationship and cooperation will remain long lasting. Thank you very much indeed. Kind regards, Dr. Andriy Sinelnyk Cell Therapy Center EmCell
