AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2692-9759/089
Research Scholar, College of Nursing, University of Kufa, Al-Najaf, Iraq.
*Corresponding Author: Ahmed Lateef Alkhaqani, Research Scholar, College of Nursing, University of Kufa, Al-Najaf, Iraq.
Citation: Ahmed L. Alkhaqani, (2023), Nursing Assessment of Cardiovascular System: Importance of History Taking and Physical Examination, Cardiology Research and Reports. 5(1); DOI:10.31579/2692-9759/089
Copyright: © 2023 Ahmed Lateef Alkhaqani, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 06 March 2023 | Accepted: 20 March 2023 | Published: 31 March 2023
Keywords: congenital heart disease; pulmonary veins; blood; valves
Assessment of a patient's cardiovascular system is crucial in identifying potential problems, determining a diagnosis, and creating a care plan. The nursing assessment process involves both history taking and physical examination. History taking is important in obtaining information about the patient's past medical history, risk factors for cardiovascular disease, symptoms, and medication use. This information can help to identify potential problems, such as high blood pressure or heart disease, and provide a baseline for comparison during subsequent assessments. Physical examination includes evaluating the patient's vital signs, such as blood pressure, heart rate, and rhythm, and listening to the heart and lungs for sounds that may indicate problems, such as murmurs or crackles. The examination may also involve palpating for peripheral pulses, evaluating for edema, and assessing skin color and temperature. Together, the information gathered during history taking and physical examination forms a comprehensive picture of the patient's cardiovascular system and provides the foundation for an effective nursing care plan.
A patient who presents with signs or symptoms of heart (cardiac) problems such as chest pain may be suffering a life-threatening condition requiring immediate attention. In this situation, you act quickly and perform the parts of the examination that are absolutely necessary (1). The history of cardiovascular provides physiological and psychosocial information that guides the physical assessment, the selection of diagnostic tests collection, and the choice of treatment options. During the process of taking a detailed history and performing a physical examination, the nurse has an opportunity to create consonance with the patient and to evaluate the general emotional status of patient (2).
The cardiovascular system:
The heart and the blood vessels are made up of the cardiovascular system. The heart is a muscle that pumps blood throughout the body. That is about the size of a clenched fist in a healthy adult. The blood s, which makes up the vascular system, has two main networks: pulmonary circulation and systemic circulation (3). The cardiovascular system performs two basic functions: It delivers oxygenated blood to body tissues and removes waste substances through the action of the heart (4).
Anatomy and physiology:
The heart is a hollow, muscular organ about the size of a closed fist. It is located between the lungs in the mediastinum, behind and to the left of the sternum. The heart extent is the area between the second and the fifth intercostal space. Its right border aligns with the right border of the sternum. The left border aligns with the left midclavicular line (5). Figure 1.
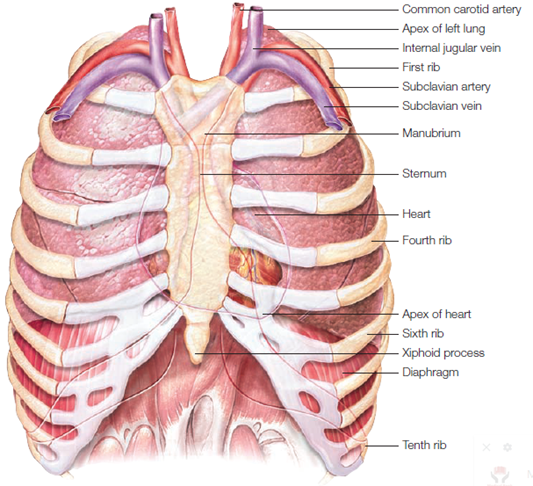
Figure 1: The heart’s location
Atria and ventricles
The heart has four chambers, two atria and two ventricles separated by a cardiac septum.
The upper atria have thin walls, which serve as blood reservoirs. They also promote the amount of blood that travels into the lower ventricles, which fill primarily by gravity. The left ventricle pumps blood against a much higher pressure than the right ventricle so that its wall is two and one-half times thicker (5).
The right side of the heart, made up of the right atrium and right ventricle, distributes venous blood (deoxygenated blood) to the lungs through the pulmonary artery (pulmonary circulation) for oxygenation. The right atrium receives blood returning from the superior vena cava (head, neck, arms, and upper limbs), inferior vena cava (trunk and lower limbs), and coronary sinus (coronary circumference) (6).
The left side of the heart, composed of the left atrium and left ventricle, distributes oxygenated blood through the aorta (systemic circulation) to the remainder of the body. The left atrium receives oxygenated blood from the pulmonary circulation via the pulmonary veins. Besides that, the amount of pressure needed to pump the blood determines the thickness of a chamber wall (4).
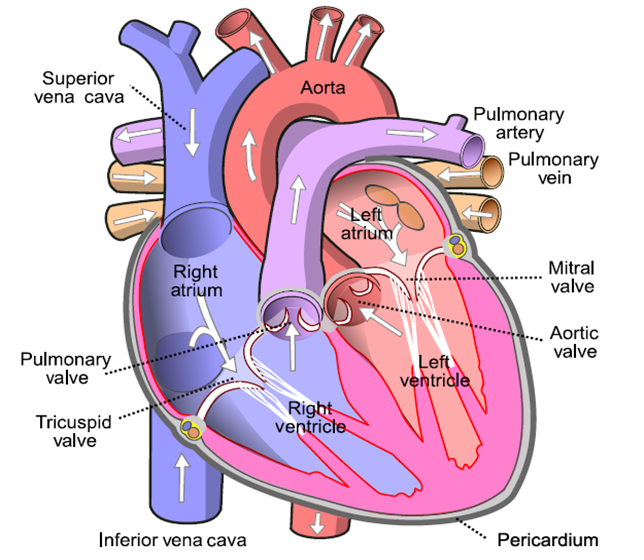
Figure 2: Structures of the heart
Cardiac Cycle
Is the rhythmic movement of blood through the heart. There are two phases of it, diastole and systole. In diastole, the ventricles relax and fill with blood. This takes up the cardiac cycle on two-thirds. The contraction of the heart in systole. During systole, blood is pumped out of the ventricles and fills the pulmonary and systemic arteries. This is one-third of the cardiac cycle (7).
Diastole.
In diastole, the ventricles are relaxed, and the AV valves (i.e., the tricuspid and mitral) are open. (Opening of the normal valve is acoustically silent.) The pressure in the atria is higher than that in the ventricles; therefore, blood pours rapidly into the ventricles. This first passive filling phase is called early or protohistoric filling (8).
Toward the end of diastole, the atria contract and push the last amount of blood (about 25% of stroke volume) into the ventricles. This active filling phase is called presystolic, or atrial systole, or sometimes the atrial kick. It causes a small rise in left ventricular pressure. (Note that atrial systole occurs during ventricular diastole, a confusing but important point) (7).
Systole
The filling phases during diastole result in a large amount of blood in the ventricles, causing the pressure in the ventricles to be higher than in the atria. This causes the AV valves (mitral and tricuspid) to shut. Closure of the AV valves produces the first heart sound (S1), which is the beginning of systole. This valve closure also prevents blood from flowing backward (a process known as regurgitation) into the atria during ventricular contraction (9).
Event of the cardiac cycle:
The autonomic nervous system controls the heart, which pumps blood through the entire body. The vascular network that carries blood throughout the body consists of high-pressure arteries, which deliver the blood, and low-pressure veins, which return it to the heart (10).
Heart Sounds:
Events in the cardiac cycle generate sounds that can be heard through a stethoscope over the chest wall. These include normal heart sounds and occasionally extra heart sounds and murmurs Figure (3) (Jolobe and Vijay, 2015).
Normal Heart Sounds
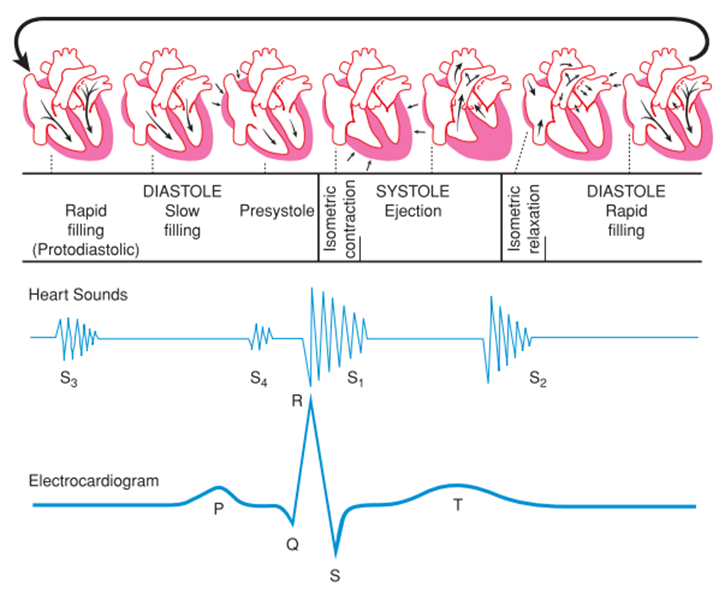
Figure 1: Cardiac Cycle
General examination
The purpose of examining the cardiovascular system is to assess the function of the heart as a pump and arteries and veins throughout the body in transporting oxygen and nutrients to the tissues and transporting waste products and carbon dioxide from the tissues. Your assessment of the cardiovascular system is important because cardiovascular disease is the most prevalent health care problem in the United Kingdom. Over 250 000 deaths per year are attributed to cardiovascular disease (13).
History Taking
The patient’s history is his health status major subjective data source. Physiological, psychological, and psychosocial information (including family relationships and cultural influences) can be obtained which will inform you about the patient’s perception of his current health status and lifestyle (14).
It will give insight into actual and potential problems as well as provide a guide for the physical examination. It is important to use open questioning to elicit the patient’s presenting complaint (15).
Provides the diagnosis most often: history, physical, or diagnostic tests (16).
Components of the Health History
Begin by asking the patient his name, address, telephone number, birth date, age, birthplace, Social Security number, race, nationality, religion, and marital status. Also, find out the names of anyone living with the patient, the name and telephone number of the person to call in an emergency, and the patient's usual source of health care (17).
The most common chief complaints of the cardiovascular system include chest pain, dyspnea, fatigue and weakness, irregular heartbeat, and peripheral changes (especially dry skin and extremity pain). In some patients, chest pain may radiate to other body parts, including the jaw, back, left arm, right arm, elbows, little fingers, teeth, and scrotum.
Further elucidation of the symptom/complaint should establish the frequency, duration, exacerbation, and severity of symptoms; assessment tools provide a framework for assessment, and SOCRATES is a popular tool:
The nurse asks for childhood diseases such as rheumatic fever as well as chronic illnesses such as pneumonia, tuberculosis, thrombophlebitis, pulmonary embolism, MI, diabetes mellitus, thyroid disease, or chest injury when determining the patient is past clinical history.
The nurse also asks about occupational exposures to cardiotoxic materials. Finally, the nurse seeks information about previous cardiac or vascular surgeries and any previous cardiac studies or interventions (19).
A significant part of history is the identification of risk factors for cardiovascular disease. Risk factors are categorized as major uncontrollable risk factors; major risk factors that can be modified, treated, or controlled; and contributing risk factors(2).
An evaluation of lifestyle and risk factors pertinent to cardiac disease should be undertaken. It is important to be non-judgmental but to ask questions sensitively and objectively. Key lifestyle factors include cigarette smoking, misuse of alcohol, recreational drug use, lack of exercise and/or obesity. Cigarette smoking is the strongest modifiable risk factor for heart disease. Seek to evaluate if the patient has ever smoked and if so, how much and for how many years(18).
Other Contributing Factors
The family history offers information about a potential predisposition to disease (e.g., heart attacks) and whether a patient may have cause to be especially concerned about a specific disease (e.g., mother died from cancer). Patients might be reluctant to talk about relatives’ illnesses if they were mental diseases, epilepsy, or cancer. Constructing a genogram of the patient’s family history will be useful for quick referral(20).
The nurse also inquiries about cardiovascular problems such as hypertension, elevated cholesterol, coronary artery disease, MI, stroke, and peripheral vascular disease(21).
Although the physical symptoms provide many clues regarding the origin and extent of cardiac disease, social and personal history also contribute to the patient’s health status. The nurse inquiries about the patient’s family, spouse or significant other, and children. Information about the patient’s living environment, daily routine, sexual activity, occupation, coping patterns, and cultural and spiritual beliefs contribute to the nurse’s understanding of the patient as a person and guides interaction with the patient and family.
Physical examination
The physical examination aims to gather objective data to confirm or refute any differential diagnoses identified from the focused history. An initial assessment should clarify if the patient is in pain or anxious, and any evidence of dyspnea, pallor, diaphoresis, or cyanosis would require urgent investigation. Examination of the cardiovascular system should include the whole circulatory system, not just the heart, and utilizes the following approach: inspection, palpation, and auscultation (19).
The general approach to heart assessment:
Appropriate patient preparation is essential to obtain accurate findings during the cardiovascular examination. The patient should be comfortable and calm, as anxiety may elevate the blood pressure or change the heart rate or rhythm [14].
Equipment needed for examination:
Cardiac assessment requires examination of all aspects of the patient to be evaluated, using the standard steps of inspection, palpation, and auscultation. A thorough and careful examination helps the nurse detect subtle abnormalities as well as obvious ones [7].
While taking the history and before inspecting the cardiovascular system, you must assess the general condition of the patient as a routine. The following points need to be examined from the cardiovascular point of view [9].
Dysmorphic features
Hands:
Provide clear instructions to the patient and minimize the number of movements they need to make (don’t have them turning their hands back and forth multiple times)
Hands out with palms downwards
Splinter hemorrhages – reddish/brown streaks on the nail bed – bacterial endocarditis
Hands out with palms facing upwards:
Cyanosis: reflects the oxygenation and circulatory status of the patient. Cyanosis is a bluish skin and mucus membrane discoloration due to reduced hemoglobin [6].
Central cyanosis manifests at a mean capillary concentration of 4 gm/dl of reduced hemoglobin. In general, when the systemic arterial saturation is less than 85%, cyanosis is manifest [12].
Clubbing loss of angle at the base of a nail. Clubbing of fingernails concerning the heart suggests cyanotic heart disease [9].
Mechanism: Platelet-derived growth factors are not inactivated in the lungs due to the right to left shunt. This results in the development of AV shunts in the distal phalanges, which results in swelling [20].
Testing
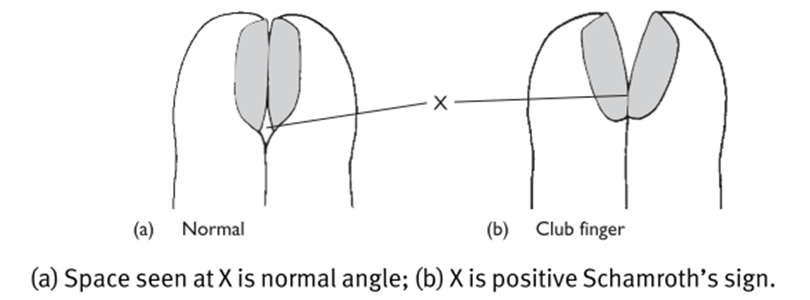
Figure 2:
Cardiac Causes
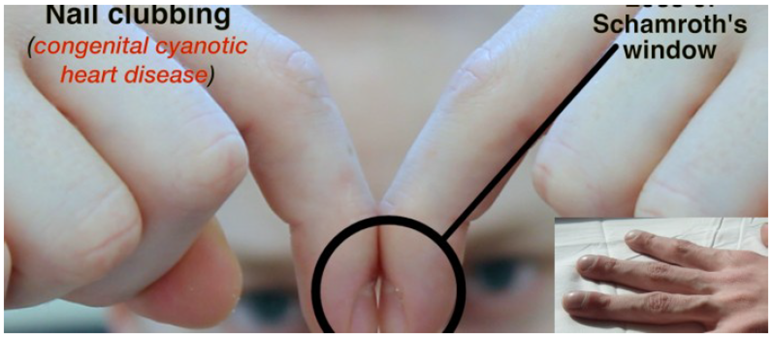
Figure 3:
Edema: is fluid accumulating in the interstitial spaces; it is not present normally.
Evaluating edema: When you detect edema, determine the degree using a scale of +1 to + 4. Press your fingertip firmly for 5 to 10 seconds over a bony surface, such as the subcutaneous tissue over the patient's tibia, fibula, sacrum, or sternum. Then, note the depth of the imprint your fingertip leaves on the skin. A slight imprint indicates +1 edema. If the imprint is deep and the skin is slowly returning to its baseline shape, the edema is a +4. The skin swells so much with severe edema that fluid cannot be displaced. Called brawny edema, this condition resists pitting but makes the skin appear distended [7].
Causes
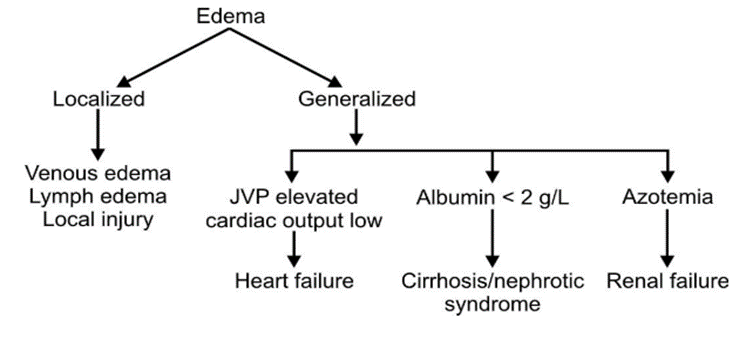
Figure 4:
Inspection of the precordium
Inspection begins as soon as the patient and nurse interact. The general appearance and presentation of the patient are key elements of the initial inspection. It is necessary to note the ability of the patient to move and speak with or without distress. Consider the patient’s posture, gait, and musculoskeletal coordination [23].
When assessing the pericardial, firstly, the examiner should be, observe the pericardial for symmetry, color, skin lesions, rash, and scars [12].
Aortic area: No pulsation should be visible. A pulsation at the aortic area is abnormal. A pulsation at the aortic area indicates an aortic root aneurysm.
Pulmonic area: No pulsation should be visible. A pulsation is an abnormal finding. A pulsation at the pulmonic area indicates pulmonary valve stenosis.
Midprecordial area: No pulsation should be visible. A pulsation or retraction at the Midprecordial area is considered abnormal findings. A left ventricular aneurysm causes mid-precordial pulsation. While precordial diseases may cause Midprecordial retraction [12].
Tricuspid area: No pulsation should be visible. A pulsation at the tricuspid area is considered an abnormal finding. A right ventricular enlargement can cause tricuspid pulsation.
Mitral area: Normally, there is a pulsation in the mitral area; this point is also knowing as a point of maximum impulse. A hypokinetic (decreased movement) pulsations at the mitral area are considered abnormal. Hypokinetic pulsation can be caused by certain conditions that put more fluids between the left ventricle and the chest wall, such as pericardial effusion and cardiac tamponade. Also, obesity, low-output states, and decreased myocardial contractility can cause this type of pulsation. Hyperkinetic pulsations (increased movement) are always abnormal when located in the mitral area. High–output states such as mitral regurgitation, thyrotoxicosis, severe anemia, and left-to-right shunt can cause this type of pulsation [24].
The neck:
CV assessment includes the survey of vascular structures in the neck—the carotid artery and the jugular veins. The carotid artery and internal jugular vein lie beneath the sternomastoid muscle. The external jugular vein runs diagonally across the sternomastoid muscle [7].
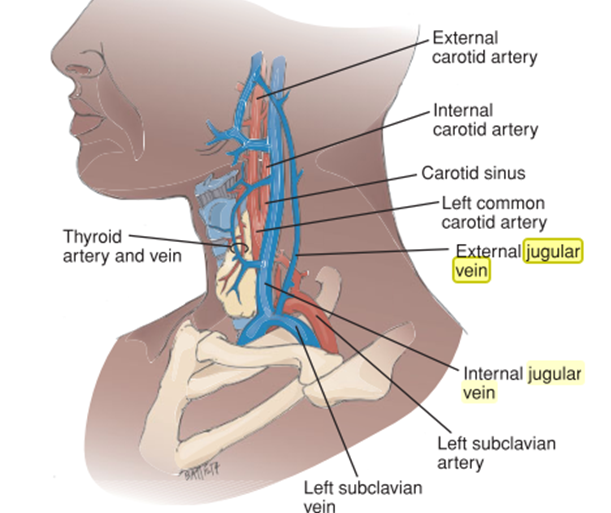
Figure 5: Major neck vessels, including the carotid arteries and jugular veins.
Jugular Venous Pulse and Pressure:
Pressure in the jugular veins reflects right atrial pressure (RAP) and provides the nurse with an indication of heart hemodynamics and cardiac function. The height of the blood level in the right internal jugular vein indicates RAP because there are no valves or obstructions between the vein and the right atrium [23].
Observe the height of the jugular venous pulsation (JVP). Position the patient lying at approximately 45° to the horizontal with his head on pillows. Shine a torch at an angle across the neck. Look at the veins in the neck. Use tangential lighting [20]. Next, the angle of Louis is located by palpating where the clavicle joins the sternum (suprasternal notch). The examining finger is slid down the sternum until a bony prominence is felt. This prominence is known as the angle of Louis. A vertical ruler is placed on the angle of Louis. Another ruler is placed horizontally at the level of the pulsation. The intersection of the horizontal ruler with the vertical ruler is noted, and the intersection point on the vertical ruler is read [9].
To estimate CVP, measure the vertical distance between the highest level of visible pulsation and the angle of Louis. Normally, this distance is less than TVs" (2.9 cm). Add 2" to this figure to estimate the total distance between the highest level of visible pulsation and the right atrium. A total distance that exceeds 4" (10 cm) may indicate elevated CVP and right ventricular failure [25].

Figure 6: Observe for a raised JVP
Suppose the patient has a central venous line connected to a hemodynamic monitoring system. In that case, you can observe jugular vein pulsations to obtain information about the dynamics of the right side of the heart. As you assess, use the carotid pulse or heart sounds to time the venous pulsations with the cardiac cycle. Finally, inspect the carotid arteries, noting whether the pulsations are weak (hypokinetic) or strong and bounding (hyperkinetic). Figure 4 [2].
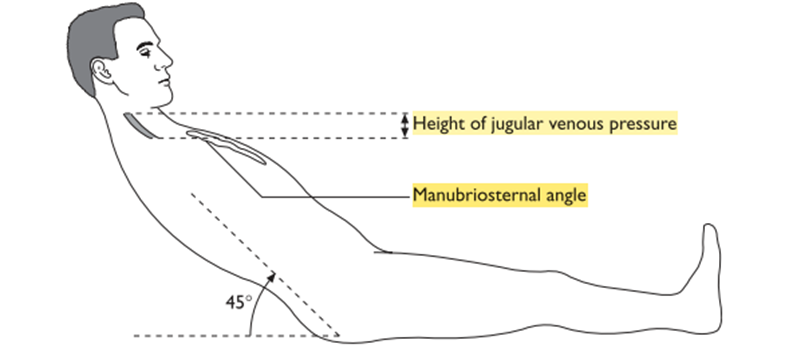
Figure 7: Assessment of jugular venous pressure. Place the patient supine in bed and gradually raise the head of the bed to 30, 45, 60, and 90 degrees.
Inspect the hepatojugular reflux
Hepatojugular (Abdominojugular) reflux occurs in right ventricular failure. It can be demonstrated by pressing the periumbilical area firmly for 30 to 60 seconds and observing the jugular venous pressure. If there is a rise in the jugular venous pressure by 1 cm or more that is sustained throughout pressure application, abdominojugular reflux is present. Kussmaul's sign is a paradoxical elevation of jugular venous pressure during inspiration and may occur in patients with chronic constrictive pericarditis, heart failure, or tricuspid stenosis(22).
A positive hepatojugular reflux sign is suggestive of right-sided heart failure/tricuspid regurgitation
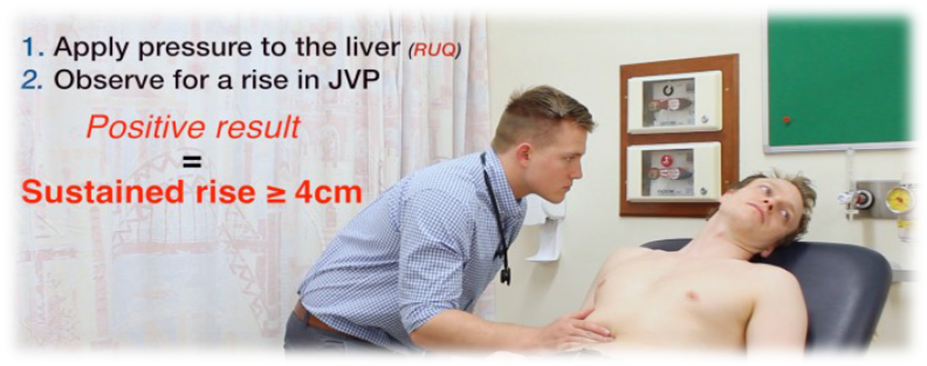
Figure 8: Assess for hepatojugular reflux
Cardiovascular assessment continues with palpation and involves the use of the pads of the finger and balls of the hand. Using the pads of the fingers, the carotid, brachial, radial, femoral, popliteal, posterior tibia, and dorsalis pedis pulses are palpated. The peripheral pulses are compared bilaterally to determine rate, rhythm, strength, and symmetry. The 0-to-3 scale is used to rate the strength of the pulse. The carotid pulses should never be assessed simultaneously because this can obstruct flow to the brain [22].
Carotid pulse: Lightly place your fingers just medial to the trachea and below the jaw angle. Carotid pulse assesses character & volume e.g., the slow rising character in aortic stenosis [26].
Femoral pulse: Press relatively hard at a point inferior to the inguinal ligament. For an obese patient, palpate in the crease of the groin halfway between the pubic bone and the hipbone [27].
Popliteal pulse: Press firmly against the popliteal fossa at the back of the knee.
Posterior tibia pulse: Apply pressure behind and slightly below the malleolus of the ankle [7].
Dorsalis pedis pulse: Place your fingers on the medial dorsum of the foot while the patient points the toes down. In this site, the pulse is difficult to palpate and may seem to be absent in healthy people.
Brachial pulse: Position your fingers medial to the biceps tendon.
Radial pulse: Apply gentle pressure to the medial and ventral de of the wrist just below the thumb [25].
Radial pulse – assess rate & rhythm
Palpate both radial pulses simultaneously. They should occur at the same time in a healthy adult. A delay may suggest aortic coarctation.
Collapsing pulse: associated with aortic regurgitation
You should feel a tapping impulse through the muscle bulk of the arm as the blood empties from the arm very quickly in diastole, resulting in a palpable sensation(20).
This is a Water hammer pulse and can occur in normal physiological states (fever/pregnancy), or in cardiac lesions (e.g., AR / PDA), or in high output states (e.g., anaemia / AV fistula/thyrotoxicosis)

Figure 9: Collapsing pulse
Arterial pulses: Weak pulses indicate low cardiac output or increased peripheral vascular resistance, as occurs in arterial atherosclerotic disease. Weak pedal pulses are common in elderly patients. A strong bounding pulse occurs in patients with hypertension and in high cardiac output states, such as exercise, pregnancy, anemia, and thyrotoxicosis [9].
Rating Scale Used for Assessing Strength of Pulses:
0 Absent pulse
1+ Present but diminished pulse
2+ Average normal pulse
3+ Moderately increased
4+ Markedly increased pulse
Rate: The resting heart rate shows considerable variation ranging between 60 to 100 beats/min. The rate should be counted for at least 30 seconds. When the rhythm is irregular, count for a full one minute [25].
Rhythm: The normal rhythm is initiated from the sinus node, and this follows a regular cycle within physiological variations. The rhythm can be intermittently irregular or can be continuously irregular. The common causes for an intermittently irregular pulse are either ventricular premature beats or supraventricular premature beats [6].
Palpation of precordium
The nurse may feel a thrill (vibrations that feel similar to what one feels when a hand is placed on a purring cat), heaves (lifting of the cardiac area secondary to an increased workload and force of the left ventricle contraction, or pulsation. The patient should be in a supine position for this portion of the assessment [24].
Palpate the cardiac landmarks for:
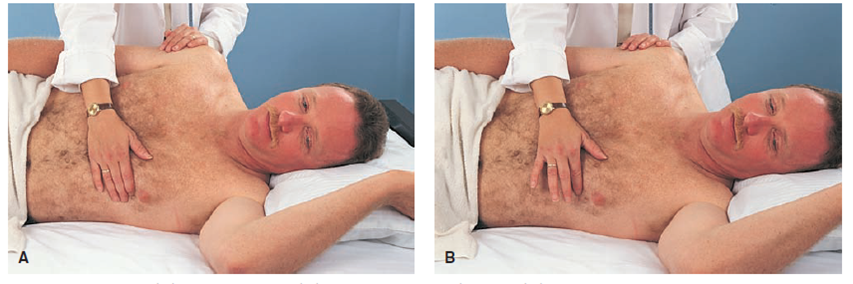
Figure 10:
Aortic area: No pulsation, thrills or heaves should be palpated. Aortic regurgitation or stenosis can caused a turbulent blood flow in the left ventricle, which may be palpated as a thrill [28].
Pulmonic area: No pulsation thrills or heaves should be palpated. Pulmonic regurgitation or stenosis can cause a turbulent blood flow in the right ventricle, which may be palpated as thrills.
Midprecordial area: No pulsation thrills or heaves should be palpated. Both left ventricular aneurysm, and right ventricular enlargement can produce a pulsation in the midprecordial area [19].
Tricuspid area: No pulsation thrills or heaves should be palpated. Tricuspid regurgitation or stenosis can cause a turbulent blood flow in the right atrium, which may be palpated as thrills. Right ventricular enlargement can produce heaves at the tricuspid area, secondary to increased ventricular workload [19].
Mitral area: Palpate the mitral area for pulsation, thrills, or heaves. If a pulsation (apical impulses) is not palpable, turn the patient to the left side and palpate in this position.
The apical impulse can be palpated at approximately half of the adult population, 1-2 cm in diameter, and the amplitude is small and can be felt directly after the first heart sounds. Mitral stenosis or mitral regurgitation may produce thrills from the turbulent of blood at the left atrium [29].
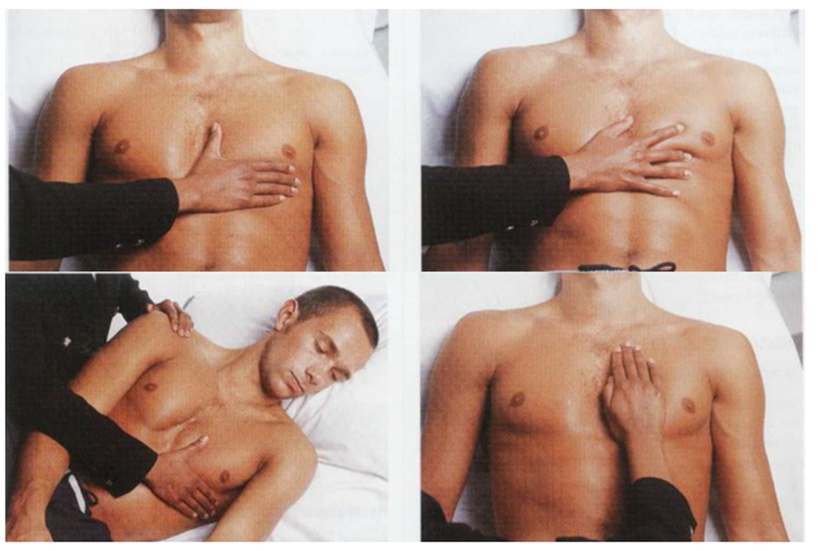
Figure 11:
Left ventricular hypertrophy produced a laterally displaced apical impulse to the sixth intercostal space. In addition, the hypertrophied muscles work harder during a contraction to produce a heave or sustained apical beats. This occurs in many cases, such as aortic stenosis, systemic hypertension, sub-aortic stenosis, and hypertrophied cardiomyopathy.
A hypokinetic pulsation less than 1-2 cm in diameter can be caused by the same cause listed under the hypokinetic pulsation in the inspection of the mitral area [30].
With the advent of radiological means of evaluating cardiac size, percussion is not significantly contributing to cardiac assessment. However, a gross determination of heart size can be made by percussing for the dullness that reflects the cardiac borders [31].
Data obtained by careful and thorough auscultation of the heart are essential in planning and evaluating care of the critically ill patient [23].
Listen with the stethoscope over all five auscultatory areas during auscultation, first with the diaphragm and then with the bell. Be sure to listen through several cardiac cycles to allow yourself enough time to become oriented to the sounds and to hear any subtle changes [31].
The examination should be done in a quiet, well-lighted, comfortable room, and the patient should be relaxed and comfortable properly gowned, and adequately exposed to the waist. Usually, the examination is initiated from the right side [12].
The patient is placed in a recumbent position with the trunk elevated 30 to 45 degrees. To help here abnormal sounds, the patient may be asked to roll partly onto the left side (left lateral decubitus position). This position helps bring the left ventricle closer to the chest wall [23].
The key is to use a systematic approach to listening and describing what is heard. There are four valves (mitral, tricuspid, pulmonary and aortic), and each has an auscultatory area. These areas reflect sounds transmitted in the direction of blood flow as it passes through the valves, not surface markings of the valves. For this reason, there are fi rekey listening areas [32]:
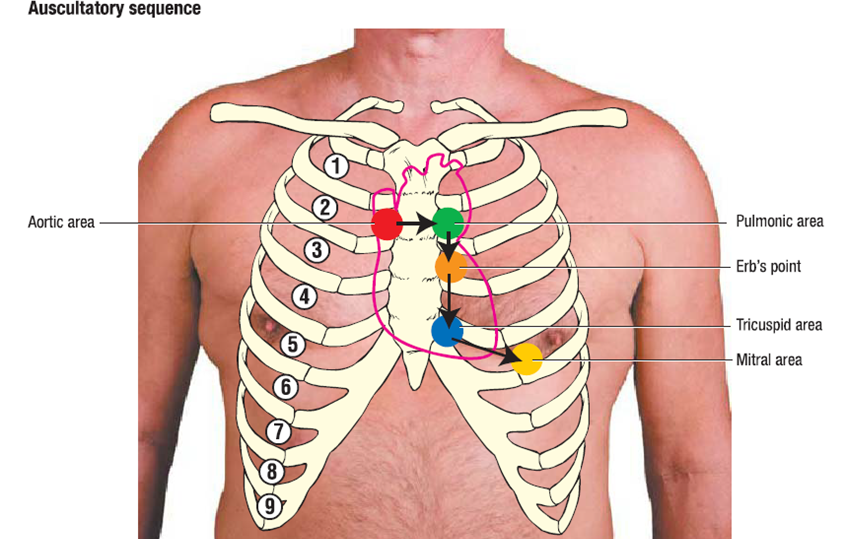
Figure 12: Area of auscultation
Capillary refill: Capillary refill time provides an estimate of the rate of peripheral blood flow. When the tip of the fingernail is depressed, the nail bed blanches. When the pressure is released quickly, the area is repercussed and becomes pink. Normally, reperfusion occurs almost instantaneously. More sluggish reperfusion indicates a slower peripheral circulation, such as in heart failure. Normal is <2>hypovolemia More sluggish reperfusion indicates a slower peripheral circulation, such as in heart failure [33].
Blood pressure:
Measure blood pressure and note any abnormalities – hypertension/hypotension
Narrow pulse pressure is associated with Aortic Stenosis
Wide pulse pressure is associated with Aortic Regurgitation
You will often not be expected to carry this out (due to time restraints), but make sure to mention that you’d ideally like to measure blood pressure in both arms [19].
Temperature: Temperature and moistness are controlled by the autonomic nervous system. Normally, hands and feet are warm and dry. Under stress, the periphery may be cool and moist. In cardiogenic shock, skin becomes cold and clammy.
Temperature: cool peripheries may suggest poor cardiac output/hypovolemia [20].
Pulse oximetry
Pulse oximetry provides a noninvasive method of monitoring SpO2 levels, either continuously or intermittently. It is widely used in both pre-hospital and hospital settings. The normal SpO2 is >95%. Indications for use include the following [27]:
Place the probe on the patient’s finger or earlobe. If SpO 2 is monitored continuously, the nurse must change the probe's position regularly to prevent the formation of pressure ulcers and finger stiffness. If the fingers are used, remove nail polish or anything else that may cause problems with the analysis, such as blood, paint, or grime. Set the monitor alarms. Avoid placing the BP cuff on the same arm as the probe, as this will interrupt the readings. The following can lead to inaccurate readings [34]:
Do not consider SpO2 levels in isolation, but also consider the clinical presentation. In some cases, ABG will need to be obtained [35].
Varicose Veins: Are tortuous dilations of the superficial veins that result from defective venous valves, intrinsic weakness of the vein wall, high intraluminal pressure, or arteriovenous fistulas.
Diagnostic Evaluation
Diagnostic tests and procedures are used to confirm the data obtained by the history and physical assessment. Some tests are easy to interpret, but expert clinicians must interpret others. All tests should be explained to the patient. Some necessitate special preparation before they are performed and special monitoring by the nurse after the procedure [36].
Laboratory tests may be performed for the following reasons:
Cardiac Biomarker Analysis
Plasma levels of cardiac biomarkers are used to diagnose acute MI in conjunction with the history, physical examination, and ECG. These substances leak into the bloodstream after injured myocardial cells rupture their cell membranes. Biomarkers have a specific timeline for when they first rise, peak, and then return to normal. This timeline helps the clinician decide which test to order based on the timing of patient’s symptom onset [34].
Reading a rhythm strip
12-lead electrocardiogram (ECG)
The Electrocardiogram (ECG) is a graphic record of the electrical activity generated by the heart's cells, recorded at the body surface by electrodes and displayed on a cardiac monitor or ECG paper as a visual record. The electrodes detect the electrical current generated by depolarization and repolarization of the atria and ventricles during each cardiac cycle [18]. The largest electrical current flows from the base to the apex of the heart in a right to left direction [34].
Analyzing a Rhythm Strip: the analyzing should always be given in the same sequence:
Finally, you need to pull together all your ECG findings and draw a conclusion about what the ECG shows, placing your findings in the context of the clinical information provided. This is where you apply your knowledge of the ECG and what each ECG feature can indicate in order to draw conclusions about the patient’s condition [37].
Finally, the purpose of examining the cardiovascular system is to assess the function of the heart as a pump and arteries and veins throughout the body in transporting oxygen and nutrients to the tissues and transporting waste products and carbon dioxide from the tissues. A patient with signs or symptoms of heart (cardiac) problems, such as chest pain, may suffer a life-threatening condition requiring immediate attention. The history of cardiovascular provides physiological and psychosocial information that guides the physical assessment, the selection of diagnostic tests collection, and the choice of treatment options.
No funding.
The author declares no conflict of interest to declare for publication
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti
Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation. “The peer review process was efficient and constructive, and the editorial office provided excellent communication and support throughout. The journal ensures scientific rigor and high editorial standards, while also offering a smooth and timely publication process. We sincerely appreciate the work of the editorial team in facilitating the dissemination of innovative approaches such as the Bonori Method.” Best regards, Dr. Matteo Bonori.

I recommend without hesitation submitting relevant papers on medical decision making to the International Journal of Clinical Case Reports and Reviews. I am very grateful to the editorial staff. Maria Emerson was a pleasure to communicate with. The time from submission to publication was an extremely short 3 weeks. The editorial staff submitted the paper to three reviewers. Two of the reviewers commented positively on the value of publishing the paper. The editorial staff quickly recognized the third reviewer’s comments as an unjust attempt to reject the paper. I revised the paper as recommended by the first two reviewers.

Dear Maria Emerson, Editorial Coordinator, Journal of Clinical Research and Reports. Thank you for publishing our case report: "Clinical Case of Effective Fetal Stem Cells Treatment in a Patient with Autism Spectrum Disorder" within the "Journal of Clinical Research and Reports" being submitted by the team of EmCell doctors from Kyiv, Ukraine. We much appreciate a professional and transparent peer-review process from Auctores. All research Doctors are so grateful to your Editorial Office and Auctores Publishing support! I amiably wish our article publication maintained a top quality of your International Scientific Journal. My best wishes for a prosperity of the Journal of Clinical Research and Reports. Hope our scientific relationship and cooperation will remain long lasting. Thank you very much indeed. Kind regards, Dr. Andriy Sinelnyk Cell Therapy Center EmCell
