AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2690-1897/240
Ferhat Abbas University. Sétif, faculty of Medicine. Algeria Research laboratory "Laboratory of Investigation and Specialized Research in Health, Environment and Innovations" (LIRSSEI). General Surgery Department; Sétif University Hospital. Algeria.
*Corresponding Author: Ouahab Ilhem, Ferhat Abbas University. Sétif, faculty of Medicine. Algeria Research laboratory
Citation: Ouahab Ilhem, (2025), What Surgery for Complicated Intestinal Crohn's?, J, Surgical Case Reports and Images, 8(2); DOI:10.31579/2690-1897/240
Copyright: © 2025, Ouahab Ilhem. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 04 February 2025 | Accepted: 19 February 2025 | Published: 26 February 2025
Keywords: crohn's disease; complications; resistance to medical treatment; surgery; complex management
Complications are characteristic of Crohn's disease. Surgery is the standard treatment for complicated forms.
The aim of our study is to clarify the role of surgery in the management of complicated intestinal Crohn's disease and to assess morbidity and mortality. Retrospective study from January 2014 to October 2024, collecting all complicated forms of Crohn's disease operated on in the general surgery department; Sétif University Hospital. The main complications found in our operated patients are stenosing, fistulizing and abscess complications. We deplored one death in the immediate postoperative period. Eleven patients presented with postoperative complications (anastomotic fistulas and surgical site infection). Postoperative recurrence was observed in five cases. The management of complicated forms of Crohn's disease requires multidisciplinary consultation. Surgery improves patient comfort but morbidity remains significant.
Crohn's disease (CD) is a chronic intestinal inflammatory disease whose origin remains of unknown cause to this day. It can affect all segments of the digestive tract from the mouth to the anus with predilection for the terminal ileum, the colon and the anoperineal region. Currently, it is clearly increasing with preference in young adults. It is often a serious disease, requiring multidisciplinary management. Currently, there is no curative treatment. The contribution of new therapies is only symptomatic and aims to induce the longest possible remission.
The chronic and recurring nature of this disease means that one in two patients will be operated on during its progression. Surgery is necessary in more than 80% of patients with Crohn's disease (1). Regardless of the type of intervention performed, it will not cure the patient, who will be exposed in the long term to a recurrence in the remaining intestine, and this in the majority of cases (2).
This risk must give priority to the principle of intestinal sparing and only operate on complicated symptomatic and/or resistant forms or after failure of medical treatment.
The aim of the study is to clarify the good indications for surgery in the management of complicated intestinal Crohn's and to evaluate morbidity and mortality. Anoperineal lesions of Crohn's disease are not elucidated in this study.
This is a retrospective study from January 2014 to October 2024, collecting all complicated forms of intestinal Crohn's disease operated in the surgery department; Sétif University Hospital. The patients were referred by the internal medicine department, gastroenterology unit, through surgical emergencies and received at the outpatient consultation of digestive and general surgery. The data were collected on hospitalization records, outpatient follow-up in collaboration with the attending physician.
One hundred and ninety (190) patients were collected in our study. - Sex: 107 (56%) men and 83 (44%) women with a sex ratio M / F of 1.28.
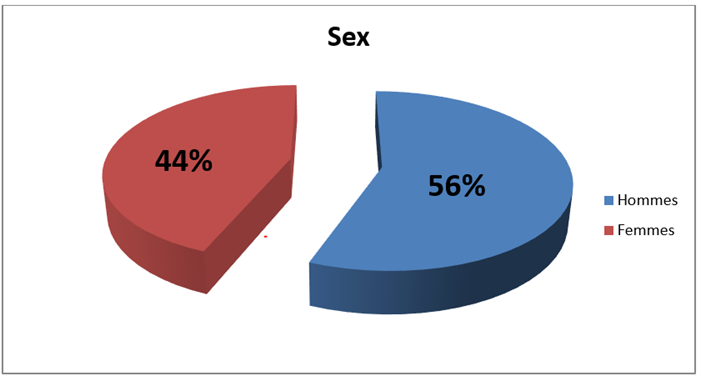
Figure 1: Gender distribution.
-Age: The mean age of the patients was 33 years (16 – 76 years).
- Mode of admission and history of Crohn's disease: Seventy-four percent (74%) of patients (n=140) were operated on as part of the surgical program where Crohn's disease was known or suspected and 26% of patients (n=50) were operated on urgently for acute intestinal obstruction or painful and febrile syndrome of the right iliac fossa or acute peritonitis.
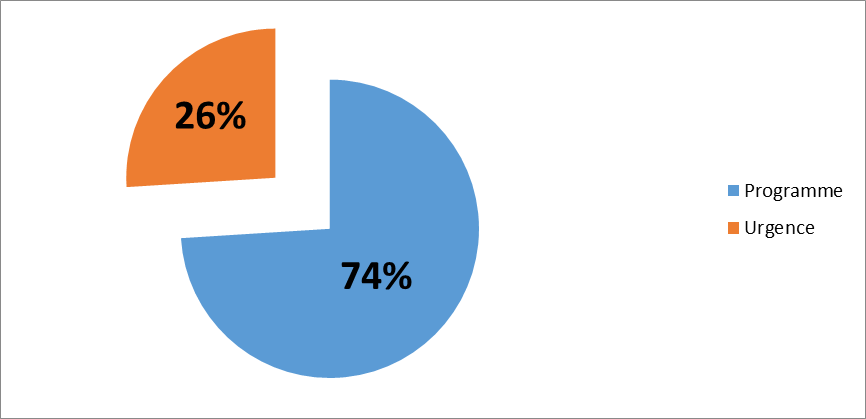
Figure 2: Distribution of patients according to admission method.
- Indications for surgery: -Good surgical indications were represented by the following complications: *Acute intestinal occlusion in 17% (n = 32), *Repeated subocclusive syndrome in 34% (n = 65), *Digestive fistulas in 39% of cases (n = 75) including 24% (n = 45) of enteroenteral fistulas, 5% (n = 10) of enteroenteral fistulas with intra-abdominal abscess, 1% (n = 2) of enterosigmoid fistulas, 3% (n = 5) of enterovesical fistulas, 1% (n = 3) of enterouterine fistulas and 5% (n = 10) of enterocutaneous fistulas. *Acute generalized peritonitis in 3% (n = 5); *Abscess at the level of the right iliac fossa in 3% (n = 6) (radio-guided drainage then surgical resection); *Terminal ileitis with acute appendicitis in 4% (n = 7) (primary emergency appendectomy before any surgical resection).
-Additional examinations: Additional examinations were performed in our patients. Abdominopelvic CT scan was performed in 20% (n = 38), entero-MRI in 74% (n = 140), abdominopelvic ultrasound in 7% (n = 13), unprepared abdomen in 4% (n = 7). Endoscopy was performed in 47% (n = 90).
intestinal lesions : The ileocecal location was predominant in 67% (n = 127) followed by the intestinal location in 20% (n = 39) then that of the colon in 13% (n = 24).

Figure 3: Topography of intestinal lesions in Crohn's disease.
-Type of complications: The complications generated in our series were represented by intestinal stenosis in 51%, by internal fistulas in 39%, terminal ileitis with acute appendicitis in 4%, abscess of the right iliac fossa in 3% and perforation in 3%.
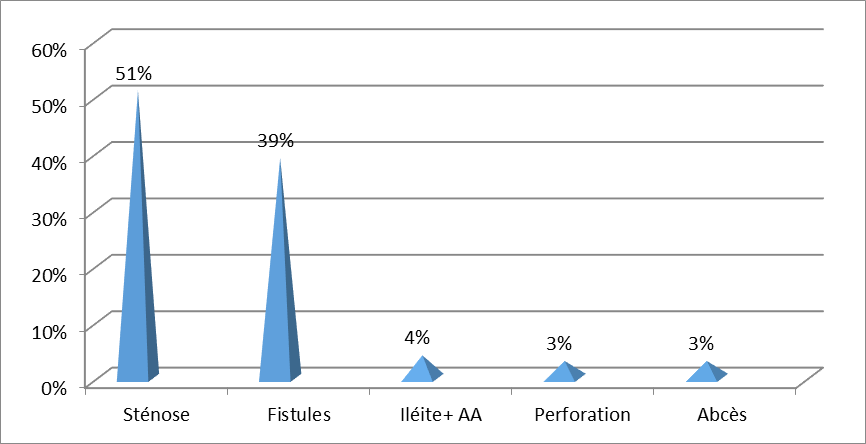
Figure 4: The different complications of Crohn's disease in our series.
- Treatment: *Medical treatment:
Sixteen percent (n = 30) of patients operated on cold in the surgical program received specific treatment for Crohn's disease such as salicylate derivatives, 42% (n = 80) received an immunosuppressant and 20% (n = 28) were on corticosteroid therapy and 1% (n = 2) were put on anti TNF alpha before surgery.
*Surgical treatment: All patients in our series were operated on by laparotomy. Ileocecal resection was performed in 92% (n = 175): Ileocecal resection removing the fibrous stenosis responsible for subocclusive syndromes in 34% (n = 65), ileocecal resection removing enteroenteral fistulas in 24% (n = 45), ileocecal resection with suture of the sigmoid colon (victim of the lesion) in 0.5% (n = 1), ileocecal resection with sigmoid resection (diseased sigmoid) in 0.5% (n = 1), ileocecal resection with suture of the bladder and bladder catheterization in 3% (n = 5), ileocecal resection with suture of the uterus in 1% (n = 3), ileocecal resection after radioguided drainage of the intra-abdominal abscess in 3% (n = 6), ileocecal resection at the same time as surgical drainage in 5% (n = 10), ileocecal resection after failure of medical treatment 13% (n = 25) and emergency ileocecal resection removing the stenosed colonic segment in 7% (n = 14). Flattening of the cutaneous fistula. Right hemi colectomy was performed in 5% (n = 10) and segmental ileal resection in 3% (n = 5).
- The immediate restoration of continuity was cold in 155 patients, i.e. a rate of 82% and a stoma was performed urgently in 18% (n = 35).
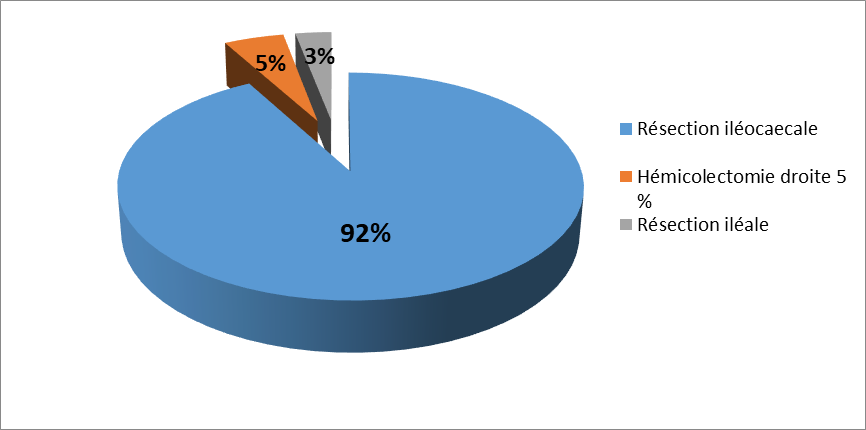
Figure 5: Surgical gestures performed.
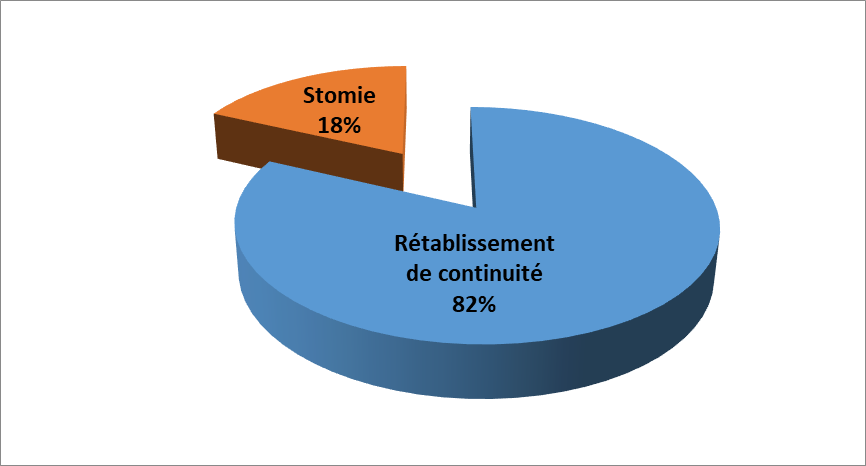
Figure 6: Restoring continuity.
- Postoperative course: *The immediate postoperative course was simple for all patients operated on cold except for 2 cases of surgical site infection. *For patients operated on urgently, anastomotic fistulas were observed in 4 patients and surgical site infection in 5 patients. The duration of hospitalization was 5 to 7 days postoperatively. *We deplored one case of death of a patient operated on for acute intestinal obstruction in emergency in a cachectic state. *Recurrence occurred in 5 patients (3%).
| Post-operative care: | Number (Nb): | Percentage (%): |
| Anastomotic fistulas: | 4 | 2 |
| Surgical site infection: | 7 | 4 |
| Death | 1 | 0.5 |
| Recidivism | 5 | 3 |
| Total : | 17 | 9 |
Table 1: Morbidity, mortality and recurrence of Crohn's disease in our series.
All operated patients received post-operative medical treatment, such as immunosuppressants or anti-TNF alpha or both combined, initiated by gastroenterologists.
Surgical treatment is part of the therapeutic arsenal in the management of Crohn's disease. The indications for surgery are for progressive complications of the disease on the one hand and on the other hand for the failure of prior medical treatment. Seventy to eighty percent of CD carriers will have to undergo surgical treatment, in greater proportion on the small intestine than on the colon (3), at least once in the ten years following diagnosis (4). Surgery improves the quality of life but it will not cure the patient who will remain exposed to recurrence. The principle of surgery is to limit the indications to complicated forms and / or resistant to medical treatment, and to limit intestinal resection to lesions responsible for the observed symptoms only.
The male gender was predominant in our study 56 % male versus 44
Crohn's disease is a lifelong inflammatory disease of the digestive tract. It is a disease of young people that is often serious. Its management is complex, requiring medical-surgical skills. Crohn's disease is an enigma where the pathophysiology and multifactorial etiology are still not understood and there is no curative treatment (35-36). Currently, there is no standardized management. Surgery is the reference treatment for symptomatic complications and relapses of medical treatment. Postoperative prophylactic medical treatment is mandatory to avoid recurrences (37).
The authors declare no conflicts of interest.