AUCTORES
Globalize your Research
Short Communication | DOI: https://doi.org/10.31579/2640-1053/232
1Department of Pathological Anatomy, Arrazi Hospital, University Hospital of Mohammed VI - Marrakech / Faculty of Medicine and Pharmacy of Marrakech - Cadi Ayyad University Marrakech/Morocco.
2Guelmim Faculty of Medicine and Pharmacy - Ibn Zohr Agadir University Guelmim- Morocco 81000.
3Department of Ophthalmology, University Hospital of Mohammed VI - Marrakech / Faculty of Medicine and Pharmacy of Marrakech - Cadi Ayyad University Marrakech/Morocco.
4Department of Radiology, Arrazi Hospital, University Hospital of Mohammed VI - Marrakech / Faculty of Medicine and Pharmacy of Marrakech - Cadi Ayyad University Marrakech/Morocco.
*Corresponding Author: Imane Boujguenna, University Hospital of Mohammed VI - Marrakech / Faculty of Medicine and Pharmacy of Marrakech - Cadi Ayyad University Marrakech/Morocco.
Citation: H. Rachidi, I. Boujguenna, C. Dabaj, M. Dref, A. Moutaouakil, et al, (2025), Unusual Location of a Melanoma: Consider it in The Presence of Decreased Visual Acuity, J. Cancer Research and Cellular Therapeutics. 9(2); DOI:10.31579/2640-1053/232
Copyright: © 2025, Imane Boujguenna. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 28 February 2025 | Accepted: 07 March 2025 | Published: 14 March 2025
Keywords: melanoma; choroid; histology; immunohistochemistry
Choroidal melanoma (CM) is malignant neoplasm of melanocytes in choired. It is the most common intraocular malignant neoplasm in adults. The diagnosis is based on histological and immunohistochemical examination. These tumors have a pejorative prognosis and their evolution is marked by the appearance of metastases especially in the liver. Currently, the development of genomic analyzes has led to a better understanding of the molecular mechanisms involved in oncogenesis. Therapeutic management has become much more difficult since the appearance of conservative treatments to keep the eye. We report a new case of choroidal melanoma in a 29-year-old patient diagnosed at the pathology department of the Mohammed VI CHU (Marrakech, Morocco). The aim of this work is to study the anatomo-clinical and evolutionary aspects of this infrequent entity.
Choroidal melanoma develops from melanocytes located in the choroidal tract, which consists of the choroid, ciliary processes, and iris. It is the most common tumor among intraocular tumors [1]. Its appearance may be linked to the degeneration of melanocytes or a nevus. The clinical symptoms as well as the radiological assessment allow for the suspicion of choroidal melanoma, but the definitive diagnosis relies primarily on histopathological examination combined with immunohistochemical study. It is a serious disease marked by a high rate of metastases, particularly hepatic. We report a case of primary choroidal melanoma in a 29-year-old patient. Based on this observation, we will analyze the anatomo-clinical characteristics of choroidal melanomas and describe the morphological particularities of the different histological types.
Clinical presentation: Mr. H.E, 29 years old, with no particular pathological history, consulted for a progressive decrease in visual acuity of the right eye over the past 2 months without any other associated signs. The ophthalmological examination revealed decreased visual acuity with a normal anterior segment examination. The posterior segment examination highlighted a convex, achromic subretinal mass in the vitreous, and the ocular tension was 11 mmHg. The fundus examination revealed the presence of a pigmented lesion in the superotemporal quadrant. It was then decided to perform an ultrasound, which showed the presence of a dome-shaped hypoechoic choroidal lesion in the superotemporal region with signs of choroidal excavation and without rupture of Bruch's membrane (Figure 1). Magnetic resonance imaging was performed and showed the presence of a focal intravitreal thickening adherent to the temporal sclera of the right eye, measuring approximately 3 mm and extending over about 10 mm, convex inward in T1 hyperintensity, T2 hypointensity, associated with a vitreous detachment (Figure 2). A hepatic ultrasound showed the absence of metastases. Given these clinical and paraclinical data strongly suggesting a malignant melanoma, enucleation seemed to be the best solution, thus allowing for a pathological examination of the globe. On the macroscopic level, the optic nerve was resected up to 0.3 cm. Upon opening the sclera, a small lesion of dark color and translucent appearance was present. Upon histological examination, the lesion corresponded to a malignant tumor proliferation with a lobular architecture. It is made up of large cells, sometimes globular, sometimes spindle-shaped. The nuclei are large, housing a prominent nucleolus. Presence of abnormal mitoses estimated at 4 mitoses/10 fields at high magnification. Their cytoplasm was loaded with melanic pigments. The stromal reaction was fibro-inflammatory. Presence of associated tumor necrosis. The margin of the optic nerve was healthy. Absence of invasion of the lamina cribrosa, ciliary body, and sclera (Figure 3). The immunohistochemical study was conducted and showed a cytoplasmic staining of the tumor cells with the anti-Melan A antibody and the anti-HMB45 antibody (Figure 4). The patient was then followed up regularly and so far, no distant metastasis has been detected.
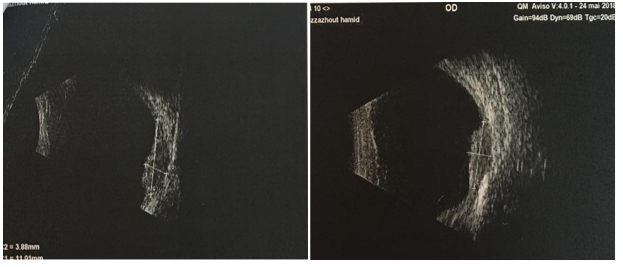
Figure 1: On ultrasound, a dome-shaped hypoechoic choroidal lesion in the superotemporal quadrand with a sign of excavation choroidal and without rupture of the Bruch's membrane.
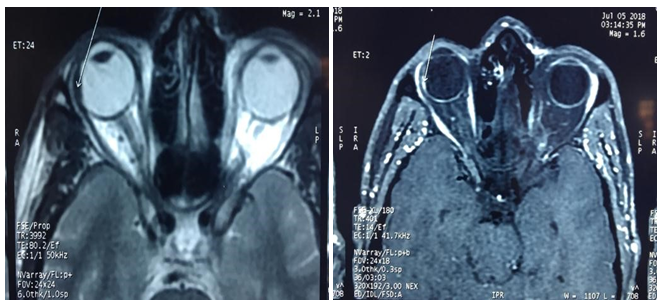
Figure 2 : At the MRI, a temporal choroidal lesion of the right eyeball shows hyperintensity on T1, hypointensity on T2, and enhancement after contrast agent injection.
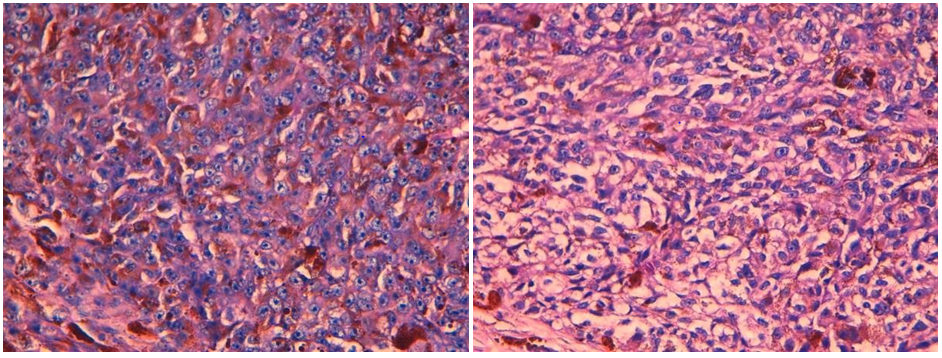
Figure 3 : Upon histological examination, it is a mixed malignant tumor proliferation with lobular architecture. It is composed of large cells, sometimes epithelioid, sometimes spindle-shaped.
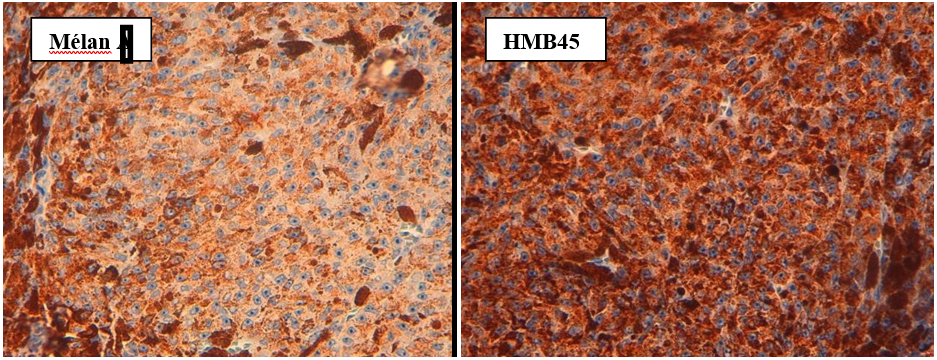
Figure 4 : The immunohistochemical study revealed a cytoplasmic staining of tumor cells with the anti-Melan A antibody and the anti-HMB45 antibody.
Choroidal melanoma is the most common intraocular malignant tumor in adults with an incidence of 6 to 7.2 per million per year and represents 5% of all melanomas [2]. A growth in the number of cases reported annually has been noted and can be explained by an increase in the incidence of the disease and the attention given to its diagnosis. The average age of diagnosis is 55 years with a male predominance [3]. It is rarely observed before the age of 20 [4]. Its etiology has not yet been elucidated. Congenital melanosis and congenital nevi have been identified as predisposing factors [5]. It is more common in individuals with light skin and light-colored irises. However, the links between sun exposure and the development of choroidal melanoma have not been proven [6]. This tumor originates from the melanocytes of the choroidal tract, which consists of the iris, ciliary processes, and choroid. Clinically, the symptoms primarily depend on the topography and size of the lesion. Located most often at the level of the choroid, the tumor is generally asymptomatic at first. The increase in size subsequently causes a scotoma or poorly systematized visual disturbances, which form the alert symptoms in most cases [7]. The fundus examination remains a key test for the diagnosis and evaluation of choroidal melanoma. It is complemented by ultrasound, which typically shows a convex image at the vitreous level with low echogenicity and a less echogenic area at its posterior part due to the attenuation of the tumor tissue and also the presence of a choroidal excavation. MRI serves as an adjunct in therapeutic decision-making and allows for the specification of the lesion's characteristics, as well as its extension to the optic nerve and orbit. The lesion appears as hyperintense on T1 and proton density, and hypointense on T2 with a clear but variable enhancement [8]. In the presence of any clinical and paraclinical suspicion of a choroidal melanoma, histological confirmation is always necessary.
The performance of a cytological biopsy of an intraocular tumor is the subject of numerous controversies because it exposes the patient to the risk of dissemination, retinal detachment, and hemorrhage. Histopathological analysis remains the key examination. It allows to confirm the diagnosis of choroidal melanoma, to evaluate the histoprognostic criteria, and to specify the topographic extension [9]. From a histological perspective, two classical forms of choroidal melanoma are distinguished based on the morphotype of the tumor cells. The distinction between spindle cells and epithelioid cells can be difficult. Choroidal melanomas with spindle cells have a better prognosis and are characterized by very elongated cytoplasm with poorly visible boundaries and a small nucleus with a small or imperceptible nucleolus. Choroidal melanomas with epithelioid cells that have a more severe progression are often large, globular, with clear cytoplasmic boundaries, and contain a vesicular, voluminous, and nucleolated nucleus. In our case, the described histological form is the mixed form. The topographic analysis of choroidal melanomas must focus on the ciliary body, the iris, and the lamina cribrosa. The search for intra-vascular extension must be conducted carefully, as well as extra-scleral extension. The status of the optic nerve as well as that of the peri-nerve meningeal sheaths must be specified [9,10]. It seems important to us to emphasize a determining factor for prognosis, which is the size of the tumor. The diameter of the tumor is measured at the level of the widest implantation base. Beyond a certain thickness and width, it becomes uncertain to consider conservative treatment because the preservation of the eye may only be temporary [11]. The search for the expression of melanocytic differentiation markers (Mélan A and HMB45) is rarely done routinely [10]. These markers are useful in highlighting a minimal tumor infiltrate located intra-vascularly or intra-neurally. Its main differential diagnosis is intraocular carcinomatous metastasis. More rarely, in the presence of a tumor localized in contact with the ciliary processes, one should consider a leiomyoma or a schwannoma. Therapeutic management remains controversial and complex. Conservative treatment should be adopted whenever possible. However, if the melanoma exceeds a certain size, it is no longer reasonable to attempt to save the eye at all costs [12]. In about half of the patients, regardless of the treatment, the progression is marked by the development of metastases, often located in the liver. These metastases develop rapidly after the initial diagnosis, occurring mainly within the 3 years following local treatment. The prognosis is then poor with a median survival of 6 months. Choroidal melanoma is a very simple pathology from a genetic standpoint, which contrasts with its often severe progression. It is most often a mutation of the GNAQ or GNA11 genes that represents the initiating molecular anomaly. The nature of the acquired anomalies seems to be decisive for the course of the disease: an inactivating mutation of the BAP1 gene characterizes tumors with a high risk of metastasis, whereas mutations of SF3B1 or EIF1AX are associated with lesions with a favorable outcome [12].
Choroidal melanoma is a serious disease, marked by a high rate of metastases, particularly hepatic. Histopathological examination allows for a positive diagnosis and specifies the histoprognostic factors. Recent progress has been made, allowing for a better understanding of the molecular mechanisms involved in the oncogenesis of choroidal melanoma.