AUCTORES
Globalize your Research
Review Article | DOI: https://doi.org/10.31579/2578-8868/364
Neurosurgical Department, Clínica Juaneda Miramar, Palma de Mallorca, Balearic Islands, Spain.
*Corresponding Author: Gonçalo Januário, Neurosurgical Department, Clínica Juaneda Miramar, Palma de Mallorca, Balearic Islands, Spain.
Citation: Gonçalo Januário (2025), Unilateral Biportal Endoscopy (UBE), Recommendations for the Interlaminar Approach, J. Neuroscience and Neurological Surgery, 17(3); DOI:10.31579/2578-8868/364
Copyright: © 2025, Gonçalo Januário. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Received: 24 February 2025 | Accepted: 11 March 2025 | Published: 17 March 2025
Keywords: unilateral biportal endoscopy; interlaminar approach; spine pathologies; minimal invasive; disc herniation; stenosis; foraminotomy
The field of spinal surgery has evolved significantly over the past few decades, with advancements in minimally invasive techniques aimed at reducing surgical trauma, recovery time, and improving patient outcomes.One such is a novel technique, the Unilateral Biportal Endoscopy (UBE) Interlaminar Approach, which has gained attention for its effectiveness in treating a variety of spinal pathologies, particularly those involving the lumbar spine. Furthermore, it is a technique that presents economic advantages in relation to the uniportal approach and with good clinical results.UBE interlaminar approach is a minimally invasive technique used for spinal procedures, particularly in the treatment of various lumbar spine conditions. This approach utilizes two small portals: one for the endoscope and the other for the working instruments, providing a clear, high- definition view of the spinal structures through the interlaminar space.The interlaminar approach targets the epidural and intradural spaces, offering access to areas such as the lumbar nerve roots and disc herniations. Using UBE we can achieve precise decompression of nerve structures with minimal disruption to surrounding tissues. The benefits of this technique include reduced blood loss, shorter recovery times, and lower complication rates compared to traditional open surgeries. The UBE interlaminar approach combines the advantages of endoscopic visualization with the precision of minimally invasive techniques, improving patient outcomes while minimizing the risks typically associated with open spinal surgery.This article aims to provide an overview, review the methodology, clinical indications, advantages, outcomes, and potential challenges of the UBE interlaminar approach, emphasizing its role in advancing and transforming spinal surgery.
Unilateral Biportal Endoscopy (UBE) is a minimally invasive surgical technique used in spine surgery. This approach involves the use of two portals or small incisions on the same side of the patient’s body, one for the endoscope and the other for the surgical instruments. The technique has been particularly prominent in spinal procedures, offering advantages over traditional methods like open surgery.
UBE was first popularized in spinal surgery for its ability to reduce muscle disruption and facilitate more precise, less invasive access to the spine. It has since gained recognition in a range of spinal procedures, from discectomies to decompressions and associated with spinal fusions when necessary. Unlike traditional open surgery, UBE allows for visualization and manipulation of the surgical site with minimal tissue dissection, offering enhanced recovery times and reduced complication rates.
With this technique, at this time, we can do two approaches interlaminar or extraforaminal. In this manuscript we will present the interlaminar approach.
The UBE interlaminar approach is a minimally invasive technique used to access the spinal canal through the interlaminar space, between two vertebras, mainly often at the level of the lumbar spine. Recently, there has been an increase in the applicability of this approach at other levels of the spine, such as the cervical and thoracic spine.
This approach allows surgeons to visualize and treat pathologies such as lumbar disc herniation, spinal stenosis, and degenerative disc disease without the need for extensive muscle dissection or the risks associated with traditional open surgery.
Indications for UBE in Spine Surgery:
Key Features and Advantages of UBE:
1. Minimally Invasive: two small incisions with less muscle dissection and tissue trauma compared to open surgery.
2. Better Visualization: the endoscopic system provides high-definition, magnified views of the surgical area, allowing for more precise and accurate procedures.
3. Enhanced Recovery: patients present faster recovery times, less postoperative pain and shorter hospital stays.
4. Reduced Blood Loss: UBE typically results in minimal blood loss compared to traditional open surgery.
5. Lower Complication Rate: UBE is a minimally invasive procedure with a reduce risk of complications such as muscle destruction, infections and nerve damage.
Procedure Overview:
During UBE, the surgeon creates two small incisions, one for the endoscope and the other for the surgical tools, on the same side of the patient’s body. The procedure can be done with different types of anesthesia, mainly with general anesthesia as in our center.
The surgery is typically guided by real-time intraoperative fluoroscopy or neuronavigation system and allows for an efficient, controlled procedure with reduced risk of muscle, ligament, and nerve injury.
UBE is continuing to evolve, with increasing application not only in spinal procedures but potentially in other areas of minimally invasive surgery. As advancements in technology and techniques improve, UBE may become a more commonly used approach in various surgical fields due to its promise of enhanced patient outcomes.
1. Two Portals for Minimally Invasive Access:
This technique uses two small incisions to create the portals, one for the endoscope and the other for surgical instruments. The endoscope provides real-time high-definition visualization of the surgical field, while the second portal allows for the manipulation of surgical tools, such as microdiscectomy instruments or spinal drills.
2. Interlaminar Space Access:
The interlaminar space, located between the laminae of adjacent vertebrae, is accessed through the portals. This area provides a route to the spinal canal for decompression of nerve roots and removal of disc herniations located medial or paramedial but always inside the canal.
3. Preserving Paraspinal Musculature:
The UBE technique significantly reduces the need for muscle stripping and retraction, which is common in traditional open spinal surgery. This preservation of paraspinal muscles contributes to a faster recovery and reduces the risk of post-operative complications like muscle atrophy.
4. High-Resolution Endoscopic Visualization:
The use of high-resolution endoscopes provides clear and magnified views of the surgical site. The correct flow of saline solution and the control of hemostasis, with the different devices such as monopolar coagulation, bipolar forceps, bone wax, permite a most clear vision. This allows for precise identification of the anatomical landmarks and treatment of spinal pathologies with minimal risk to surrounding structures such as the spinal cord, nerve roots, and blood vessels.
1. Minimally Invasive:
One of the most significant advantages of the UBE interlaminar approach is its minimally invasive nature. The procedure typically involves only small incisions (usually less than 1 cm in length), which reduces soft tissue disruption and blood loss compared to traditional open surgeries. This is especially advantageous for patients with comorbidities or those who are at higher surgical risk. Also reduce the instability in the spine during the follow-up.
2. Reduced Postoperative Pain and Recovery Time:
Due to the minimal soft tissue damage and muscle preservation, patients experience less postoperative pain. The reduced need for muscle dissection leads to a quicker recovery time, with many patients able to return to normal activities within a few weeks as opposed to several months required after open surgery.
3. Lower Risk of Complications:
The UBE technique, by preserving vital structures and providing excellent visualization, is associated with a lower risk of complications, such as nerve injury, bleeding, or infection. Additionally, the precision of the endoscopic tools reduces the risk of damage to the spinal cord or nerve roots during decompression procedures. With the high range of tools movements in UBE we reduce the risk of instability, even in cases with severe stenosis. The advantage of being able to use angled cameras allows for better visualization without having to remove more bone structure.
4. Enhanced Precision and Accuracy:
The high-definition camera and magnification capabilities of the endoscope allow surgeons to perform procedures with greater precision. This is especially beneficial in complex cases where anatomical variations or nerve root compression is present. Attention an control the saline solution flow and the hemostasis for preserve a clear vision during all the procedure.
5. Cosmetic Benefits:
The small incisions required for the procedure result in minimal scarring, providing an additional cosmetic advantage over open surgery.
1. Lumbar Disc Herniation:
One of the most common indications for UBE is the removal of herniated discs, especially when they cause nerve compression and associated symptoms like radiculopathy or sciatica. The interlaminar approach offers a direct route to the disc while avoiding the need for extensive muscle retraction or laminectomy.
2. Spinal Stenosis:
UBE has been successfully used to treat lumbar spinal stenosis, which is a narrowing of the spinal canal that can lead to nerve compression and pain. The technique allows for decompression of the spinal canal without the need for open laminectomy, preserving spinal stability.
3. Foraminotomy:
In cases where nerve root compression occurs at the neural foramina, the UBE interlaminar approach can be used for foraminotomy, a procedure that enlarges the neural foramen to alleviate pressure on the nerve root.
4. Degenerative Disc Disease:
The UBE technique can also be used for treatments related to degenerative disc disease, where endoscopic procedures may be performed to remove damaged disc material or stabilize the spine using minimally invasive techniques.
5. Spinal Tumors:
The ability to visualize the spinal canal through small incisions has also made the UBE approach useful for removing spinal tumors, particularly in cases where the tumor is located in the posterior or lateral aspects of the spinal canal. This is a high challenge but can offer for the patient a quickly and best recover when compared with the open surgeries. Depend the size and the location of the tumor maybe needed more than two portals to can control the craneal and caudal section of the lesion. In cases of intradural tumors pay attention to the pressure of the saline solution and increase the control of the hemostasis to maintain a clear vision and respect the anatomical landmarks, the vessels and the nerve roots.
The UBE interlaminar approach offers numerous benefits and permit the minimal invasive treatment of the most common pathologies (disc herniation, central stenosis, foraminal stenosis, etc). There are some challenges and limitations associated with its use:
1. Technical Skill and Learning Curve:
The UBE technique requires a high level of technical skill and experience. Surgeons need to be proficient in endoscopic procedures, and there is a learning curve associated with the proper handling of endoscopic instruments and the interpretation of real-time endoscopic imagery. It’s mandatory at the beginning select the most “easy cases” to prevent and reduce complications.
2. Limited Access in Complex Cases:
In some cases, the approach may be limited by the anatomy of the patient or the complexity of the pathology. For example, extensive disc herniation, severe spinal deformities or tumors, may make the interlaminar space difficult to access or require additional techniques. Like always we need to select the correct approach depending the patient pathology type, location and size.
3. Equipment and Setup:
The procedure necessitates specialized equipment, including high-definition endoscopes, video systems, and specialized surgical tools. The majority of the tools that we use is UBE are common with open surgery. The cost of this equipment can be prohibitive for some institutions, and it requires appropriate setup and maintenance.
4. Limited Depth of Penetration:
The approach is particularly effective for addressing pathology located in the posterior aspects of the spinal canal. However, for conditions affecting deeper structures or anterior portions of the spine, the UBE technique may not provide sufficient access. The surgeon or the team experience is very important in this point and at the beginning it's important search the most easy cases to reduce the risks of complications
How to Perform the Unilateral Biportal Endoscopy (UBE) Interlaminar Approach: Step-by-Step Recommendations:
The UBE interlaminar approach is the most used, and apply the minimally invasive technique to provides excellent access to the spinal canal through a combination of precise visualization and surgical manipulation. Here’s a general guide on how to perform the procedure, including key recommendations and steps to ensure successful outcomes:
1.1 Patient Selection:
• Indications: UBE is best suited for treating conditions like lumbar disc herniation, spinal stenosis, foraminal stenosis, and some other degenerative diseases.
• Contraindications: Severe scoliosis, significant posterior bony deformity, and other anatomical abnormalities may complicate access or make UBE “impractical”.
1.2 Imaging:
• MRI/CT Scans: Preoperative imaging should be reviewed to understand the pathology (e.g., disc herniation, stenosis, etc) and to identify the level of the spine being treated. These images guide the portal placement and we can use it in fusion with neuronavigation device.
• Radiography in flexion and extension to rule out the presence of instability that could be a contraindication to performing simple decompression surgery (without fusion).
1.3 Anesthesia:
• General anesthesia is typically used to ensure patient immobility during the procedure, though some variations may involve regional anesthesia. In our center we operate all the patients under general anesthesia.
1.4 Positioning:
• Prone Position: The patient is placed in a prone position on a spinal frame or operating table with proper padding to minimize pressure and ensure stable positioning.
• Fluoroscopy: Fluoroscopy is used intra-operatively to confirm the level of surgery and guide portal placement (Figure 1).
• Neuronavigation: provides guidance to the surgeon in the selection of entry points and during the surgery. Helps to plan a ideal surgical approach to the targeted lesion. Reduce the risk and radiation exposure. Also permit identify and defining the anatomical landmarks (Figure 1).

Figure 1: A: c-arm device; B: neuronavigation system; C: intraoperative image with fusion or radiography and neuronavigation.
2.1 Marking the Surgical Area:
• Mark the midline of the lumbar spine and the targeted interlaminar space based on preoperative imaging.
2.2 Portal Placement:
• Two-Port Technique: The UBE technique involves two small incisions, the use of fluoroscopy or neuronavigation is mandatory to select the best placement of the skin incisions for create the portals (Figure 2).
• Endoscope Portal: The first portal, typically 6–10 mm, is placed at the lateral border of the spinous process at the targeted interlaminar space. This portal is used for inserting the endoscope.
• Instrument Portal: The second portal is placed approximately 2-3 cm distance from the endoscope portal for the insertion of surgical instruments. Both portals should be aligned to ensure optimal visualization and instrument maneuverability. Ideally they allow triangulation work (figure 2B).
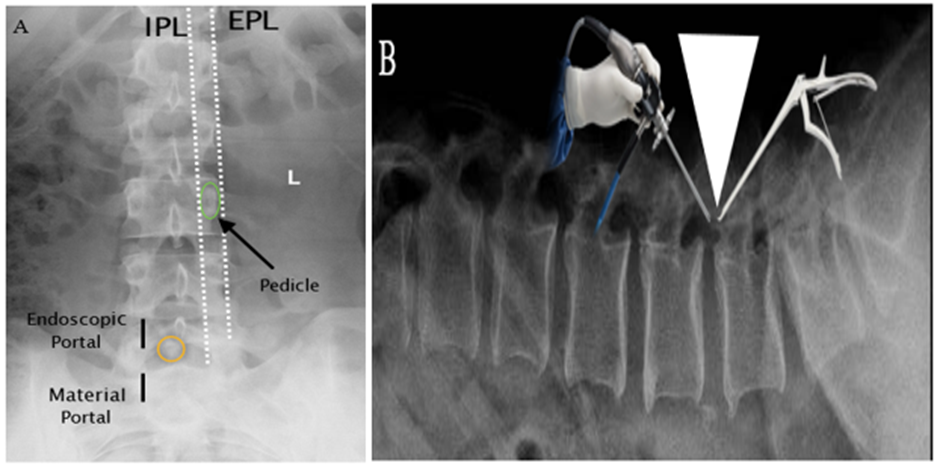
Figure 2. A: lumbar spine anteroposterior radiography, in black marks correspond to the skin incisions for interlaminar approaches for right L5-S1.
The orange circle indicates spine-laminar junction, the initial targeting area.
IPL- internal pedicle line; EPL- external pedicle line.
B: triangulation work (white triangle). We should always triangulate the endoscope and the surgical instruments.
2.3 Soft Tissue Dissection:
• Using a blunt dissection technique, carefully separate the skin and muscle tissue to reach the lamina without excessive retraction. This minimizes damage to paraspinal muscles and soft tissues. The anatomical corridor for the interlaminar approach, present two potential ways. The interfascicular related with the two small muscles of the multifidus, and the space containing fat and connective tissue located between the multifidus and the lamina. In some centers they use dilators, in our center we don’t use it because we consider the blunt dissection with periostotome safety and less invasive and permit respect the anatomical corridor.
• Muscle Preservation; Search and respect natural paths to access the interlaminar space. When we respect the two potential spaces, describes above, we can be converted to an atraumatic working path, UBE guarantees the same indications as conventional spinal surgical treatments but with concepts of minimally invasive surgery. Avoid excessive muscle stripping to preserve muscle function and enhance postoperative recovery.
3.1 Insertion of the Endoscope:
• Insert a high-definition endoscope through the first portal. A rigid endoscope with 14 mm lenght, 4 mm diameter , 0º lens. In same cases we can use 30 º lens for death angles or in cases of bilateral decompression. Use saline irrigation to clear the surgical field for better visibility. For a perfect visualization its very important the saline solution fluid between the input and output portal but also do a correct hemostasis during all the procedure.
3.2 Navigating the Endoscope:
• Advance the endoscope toward the interlaminar space. As you approach the lamina, ensure a clear view of the dural sac, nerve roots, and herniated disc (if applicable).
• In some cases, fluoroscopy or navigation systems may be used to guide precise instrument placement and confirm anatomical landmarks. Important identify and respect the landmarks and if the doubt exist we check with navigation to confirm the correct location. The surgeon must always check if what he sees on the endoscope screen corresponds to what the image from the navigation system gives us.
3.3 Surgical Instrument Insertion:
• Insert the surgical instruments (e.g., shavers, Kerrison punch, Indian knife to open the posterior longitudinal ligament, dissectors, nerve hook, or pituitary punch for microdiscectomy) through the second portal. Its importante use the endoscope for guidance and real-time visualization of all the surgical field.
• Discectomy or Decompression: Depending on the pathology, perform a discectomy (removal of herniated disc material) or decompression (removal of bone or ligamentous structures causing stenosis). With UBE we can do discectomy and unilateral, foraminal or bilateral decompression. It’s one of the great advantages of this technique with two small skin incision we can cross the midline, respect the dural folk and decompress the contralateral side with excellent results.
3.4 Avoiding Neural Injury:
• Throughout the procedure, monitor the position of the nerve roots and dural sac to avoid injury. The endoscope’s magnification and illumination help identify key structures in real time. It’s very important as describe above a correct circulation of the saline solution and a perfect hemostasis during all the procedure and particularly inside the canal near the duramater and the nerve root.
4.1 Final Inspection:
• After completing the decompression or disc removal, perform a final inspection to ensure adequate relief of the pathology, and verify that no foreign material (e.g., disc, bone or ligaments fragments) remains.
4.2 Surgical drainage
• We recommend placing a drain and maintaining it during 24 h to help to eliminate the remains water. Before place the drainage (Redon-Mini-Sets) we also recommend compress the area around the portals to facilitate removal of the saline solution.
4.3 Closing the Incisions:
• Minimal Suturing: Close the small incisions with absorbable sutures. The incisions are typically small enough, less than 1 cm, that no extensive closure is required.
• Dressing: Apply a sterile dressing over the incisions.
4.4 Postoperative Care:
• Monitoring: Keep the patient under observation for a few hours to monitor for complications, such as bleeding or nerve damage. In our center we maintain the patient 12-24h after the surgical procedure.
• Pain Management: Provide appropriate pain relief, typically through oral analgesics, since post- operative pain is minimal compared to open surgery.
• Mobilization: Encourage early mobilization within 6-12 hours postoperatively to promote recovery and reduce the risk of complications like deep vein thrombosis (DVT).
5. Follow-Up and Long-Term Care
• Postoperative Imaging: A postoperative MRI or CT scan may be performed to assess the completeness of the decompression or disc removal. If the patient present a very good clinical evolution we don’t do routinely postoperative imagen control.
• Physical Therapy: Patients may benefit from a course of physical therapy to strengthen the spine and surrounding musculature, further enhancing recovery.
• Follow-Up Appointments: Regular follow-up visits should be scheduled to monitor for potential complications, such as recurrence of disc herniation, nerve injury, or spinal instability. In our center we do a follow up 1 week after the surgery, 1 month, 2 month, 3 month and 6 months. Posteriorly 1 time per year.
Key Recommendations for Success in UBE:
1. Preparation is Crucial:
2. Minimize Tissue Dissection:
• Preserve as much muscle tissue as possible. Excessive soft tissue or muscle dissection can increase postoperative pain and slow recovery.
3. Real-Time Visualization:
• Leverage the high-definition endoscopic visualization to guide every step of the procedure, from portal placement to tissue removal. This reduces the risk of inadvertent nerve injury.
4. Use Navigation Systems:
• If available, use intraoperative navigation systems to guide portal placement, especially in complex cases or patients with difficult anatomy.
5. Assess Postoperative Recovery:
• Ensure that the patient is comfortable, monitor for complications, and offer appropriate pain management. Early mobilization and rehabilitation are key to optimizing outcomes.
UBE interlaminar approach step by step:
This endoscopic approach share concepts in common with other minimal invasive techniques. As described above the interlaminar approach is recommended for disc herniation, central estenosis, uni or bilateral foraminal estenosis, spondilolysthesis grade I.
With this approach we pretend to create an atraumatic working corridor and space through the posterior muscles:
1. Patient under general anesthesia, in prone position, flexion legs for open the interlaminar space and the foramina.
2. Check the true anteroposterior view of the C-arm fluoroscopy, O-arm. We also do a lateral view radiography in special cases of obese patients or in cases of doubts about the ideal location of skin marks. We can also use neuronavigation in fusion with radiography, Computed tomography CT or Magnetic resonance, with less radiation.
3. The ideal portals location depend and it will be according to the anatomy and body weight of the patient.
4. Make a skin mark for the endoscopic portal, which is generally located 2-3 cm cranially from the working portal, in the left side approaches and right-hand dominant surgeons. In cases of right side approaches 2-3 cm caudal from the working portal for the right-hand dominant surgeons. Take in account the patient anatomy, the distance between the two marks its variable.
5. Protocol of asepsia with betadine/povidone with 3 decontamination. After put the surgical camps 10 cm around the skin incisions. Connect and check all the electronic devices (monopolar and grounding plate, bipolar forceps, endoscope with correct with balance), confirm the saline solution fluid, it’s important remove all air from the system by filling it with saline solution before entering it in the corresponding portal.
6. Confirm with with the imaging techniques available in the operating room the correct location of the skin marks after placement of surgical fields. Made the skin incisions with less then 1cm in both portals, posteriorly open correctly the fascia. This point is very important, it will be related to the adequate flow of saline solution communication between the both portals. That would contribute together with correct hemostasis to better vision and visualization of the anatomical landmarks and different structures.
7. The periostotome is inserted, in working portal, through the interfascicular space without resistance. The direction of the core dilator is from the medial margin of the lower pedicle to the junction of the spinous process and the lamina. The upper small muscle of the multifidus anatomically attaches to the mammillary body of the lower superior articular process, which is slightly lateral to the medial wall of the lower pedicle. Use fluoroscopy or neuronavigation support if necessary to guide you.
8. With this blunt dissection in the working portal we can separate the two small multifidus muscles to widen the working space with less muscle destruction or damage.
9. It’s important respect always the same entry point and the working portal tunnel.
10. Insert a periostotome in the endoscopic portal and do the same blunt dissection as in the working portal. It’s also very important respect always the same entry point and path to the interlaminar space, prevents unnecessary muscle destruction and disorientation. Finally, check and make a triangulation between the two portals.
11. Insert the sheath with an obturator through the endoscopic portal. The tip of the sheath must touch the lamina directly for less soft tissue in front of the lens. Move the directional guide to remove some soft tissue in front of the tip of the sheath. This motion is called the “sleeve-up technique”. With this simple maneuver we increase the image quality.
12. Insert the endoscope through the endoscopic sheath. Clear visibility of the lamina indicates proper placement. If the lamina is not visible, the scope should be touched to the bone, and the elevator through the working portal help remove some of the soft tissue in front of the endoscopic lens.
13. In the working portal, if necessary, use the periostotome, dissectors, Kerrison punch, shaver, monopolar, bipolar devices to improve the path (Figure 3). In some centers use specially designed semi-tubular retractor to retract the upper small multifidus muscle. This retraction can make a wider working space.
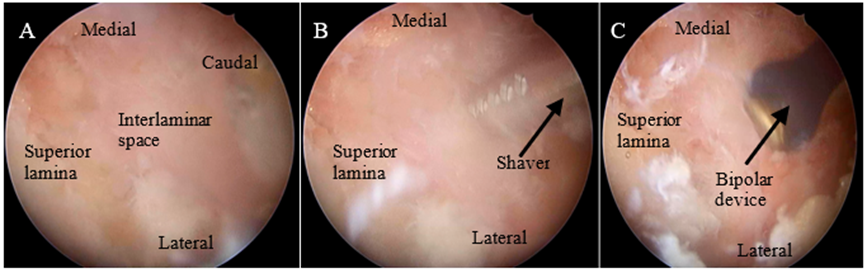
Figure 3: A- left interlaminar approach with the anatomical landmarks described. B- anatomical landmarks and shaver, used for improve the path to the interlaminar space. C- anatomical landmarks and bipolar device.
14. Keep clear in the image and in your mind the cranial, caudal, lateral and medial references. Also check triangulation work. If you have a doubt, confirm with the available intraoperative imaging techniques.
15. The correct identification of the anatomical landmarks permit performing the best approach and reduce the surgical risks or complications.
16. The next step is identify the initial target point on the intraoperative image, the junction of the spinous process and the lamina (Figure 2: orange circle).
17. Once at this point, the yellow ligament begins to detach from the lower portion of the upper lamina. Use a curette and making parallel, controlled, movements to the lamina from medial to lateral. If you notice a lot of resistance, you can also use the cutter or the kerrison punch or (Figure 4).
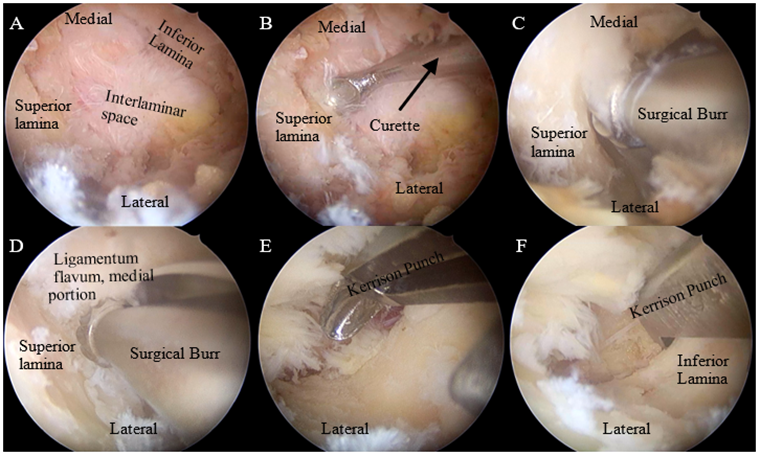
Figure 4: A- anatomical landmarks in left interlaminar approach; B- anatomical landmarks and curette to detach the ligamentum flavum; C, D- to improve the path to the canal we can also use the surgical burr. E, F- Kerrison punch other instrument to improve the way to the canal.
18. During all the surgery check the input-output of the saline irrigation. The correct fluid between the two portals permit a better vision.
19. Control the hemostasis during all the procedure it's very important. A good hemostasis with a correct fluid of saline solution permite a excellent vision and reduce the complications. Outside the canal we use monopolar device, inside de canal the bipolar forceps, if the patient present blood bone we can also use bone wax.
20. The interlaminar approach permit discectomy and unilateral or bilateral canal decompression, foraminotomy. (Figure 5).
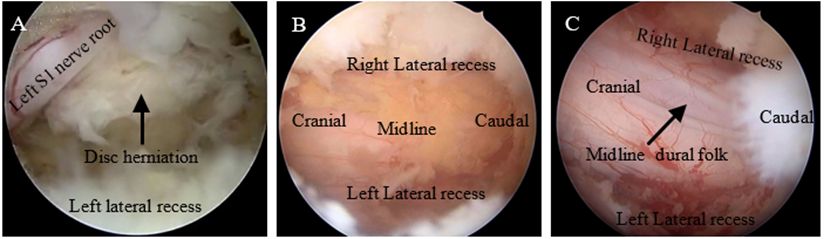
Figure 5: A- discectomy; B, C- anatomical landmarks in bilateral decompression.
21. The final part of the procedure, final inspection with a correct hemostasis technique, placing a drainage and close the incisions.
The Unilateral Biportal Endoscopy Interlaminar Approach represents a promising advancement in the field of spinal surgery. By utilizing minimally invasive techniques and high-definition visualization, UBE offers numerous benefits, including minimal invasiveness, reduced recovery time, and fewer complications, faster recovery, and fewer complications rates. While the technique presents certain challenges, particularly in terms of equipment costs and the learning curve for surgeons, its potential for improving patient outcomes in the treatment of lumbar spinal pathologies is significant.
UBE has revolutionized spinal surgery for a range of pathologies. Careful preparation, technical proficiency, and postoperative management are essential to ensure successful outcomes.
The UBE offers a safe and effective alternative to traditional open spine surgery, particularly for patients requiring decompression or disc removal.
Ongoing research and technological advancements will likely continue to refine this approach, making it a valuable option for spinal surgeons and patients alike.
All the patients, all my colleagues during my career especially to my mentor in endoscopic spine surgery Dr. Pedro Llinás. To my family for all the support.
All photos of the work belong to the author, and his rights are reserved. Copyright © reserved to the author