AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2768-2757/168
1General surgeon, Assistant professor, Surgery Department, Zahedan medical faculty, Zahedan University of Medical Sciences, Zahedan, Iran.
2Associated professor, Nephrologist, Department of Internal Medicine, Ali Ibne Abi Taleb Hospital, Zahedan University of Medical Sciences, Zahedan, Iran.
3Associated professor, Biostatics Department, Health Promotion Research Center, Zahedan University of Medical Sciences, Zahedan, Iran.
4Dentist, Periodontology resident, Dental Faculty, Tehran University of medical Sciences, Tehran, I.R. Iran.
5Associated professor, Pathologist, Department of Pathology, School of Medicine, Cellular and Molecular Research Centre, Ali Ibne Abi Taleb Hospital, Zahedan University of Medical Sciences, Zahedan, Iran.
6Infectious disease specialist, Assistant professor, Department of Internal medicine, Ali Ibne Abitaleb Hospital, Zahedan University of medical Sciences, Zahedan, I.R. Iran.
7Professor of physiology, Department of Physiology, Zahedan medical faculty, Zahedan University of Medical Sciences and Health Services, Zahedan, Iran.
*Corresponding Author: Ahmad Reza Shahraki., General surgeon, Assistant professor, Surgery Department, Zahedan medical faculty, Zahedan University of Medical Sciences, Zahedan, Iran.
Citation: Ahmad R. Shahraki, Elham Shahraki, Mahdi Mohammadi, Elahe Shahraki, Ali Reza Khazayi, et al, (2025), Time and Surgery Duration Effects on Renal Function Tests in Patients with Laparoscopic Cholecystectomy in Zahedan Ali Ibn Abi Taleb Hospital (South East of Iran), Journal of Clinical Surgery and Research, 6(3); DOI:10.31579/2768-2757/168
Copyright: © 2025, Anthony Edward Boakye. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 20 February 2025 | Accepted: 03 March 2025 | Published: 28 March 2025
Keywords:
The prevalence of gallstones has significantly increased, such that only in the US about one million cases are diagnosed each year [1]. This disease imposes a significant therapeutic-economic burden on the healthcare systems, even in western countries, to the extent that between 10% - 20% of people in the European and American societies are suffering from gallstones [2, 3] and refer to hospital emergency rooms with acute abdominal pains [4]. In most cases, gallstones symptoms are not significant. As about 25% - 50% of those suffering from gallstone develop several complications, it is necessary to remove their gallbladder [5] using surgical techniques such as laparoscopic cholecystectomy, which is highly common. Laparoscopic cholecystectomy is one of the most common abdominal surgeries and the standard treatment for gallstones and cholecystitis [6]. In addition, it is a noninvasive technique [7] intended to reduce the potential damages of the disease [8]. Apart from several advantages, laparoscopic cholecystectomy is associated with better homeostasis compared to open surgeries [9]. Due to several reasons, including the need for a small incision, low pain, short duration of hospitalization, early recovery, early start of eating food, and, in general, the quick return to daily activities, the laparoscopic cholecystectomy is the preferred option to treat most of the cases who suffer from the gallbladder [10, 11]. According to the currently available evidence, about 0.04 of cases who underwent the laparoscopic cholecystectomy develop complications [12] such as bile duct injury, acute biliary tract obstruction extrahepatic biliary duct rupture, falling gallstones into the abdominal cavity, and the subsequent formation of an abscess. Moreover, it also may cause some intraoperative complications, such as hemodynamic changes during blowing the gas into the peritoneum, including cardiac output, increased systemic vascular resistance, hypertension, heart rate changes, and reduced respiratory capacity [13]. In addition, it may cause some changes in the body, such as changes in acid-base, pulmonary status, cardiovascular system, and hemodynamic. There are reported that attributed changes in the liver function to impaired portal vein flow, decreased venous flow, and variations in intracranial pressure [14]. A dysfunction in the blood flow to the liver not only may result in liver dysfunction but also can disrupt the production of proteins made in hepatocytes, including coagulation factors (PT, PTT, and INR) [15]. Some empirical evidence reported PT and PTT levels following laparoscopic cholecystectomy [15, 16]; however, the evidence are still inconclusive over changes in the INR factor [16]. But Laparoscopy induced AKI is related with both hormonal stimuli for renal vasoconstriction and increased intra-abdominal pressure, causing hypoxemia and tubular renal injury. In conclusion, very few cases of laparoscopy induced AKI in young patients with no previous renal disease have been reported. Surgeons must consider this complication in the differential diagnosis of postoperative AKI [17]. As old patients are more prone to have pre-existing renal dysfunction, these patients are at increased risk of renal complications associated with laparoscopic surgery. In addition, living kidney donors are commonly operated via a laparoscopic approach. The effects of laparoscopy on renal hemodynamics and their potential consequences on kidney function should therefore be acknowledged by nephrologists [18].
This study did to show Laparoscopic Cholecystectomy is safe for kidneys yet.
3.1. Research Design:
The current study was carried out following a quasiexperimental design and using a convenience sampling method (for screening).
3.2. Statistical Society and Participants:
The statistical society of the present study included those scheduled for laparoscopic cholecystectomy, for whatever reasons, at Ali ibn Abi Taleb Hospital in Zahedan. A total of 21 cases were recruited.
3.3. Inclusion and Exclusion Criteria:
The inclusion criteria, which were determined based on previous studies, were as follows: all patients with symptomatic gallstones who based on ultrasonography findings had stones in their gallbladder, being aged 18 to 75 years, a maximum body mass index (BMI) of 40, normal levels of BUN and Cr markers, and being ready to undergo the surgery[13]. The exclusion criteria were patients’ intolerance to general anesthesia, having irrevocable coagulation disorders, suffering from metastatic lesions, and those whose surgery was changed from laparoscopic to open surgery during the surgery [19].
3.4. Experimental Design:
The present study was carried out in a way that, before the surgery, a venous catheter was considered for the patients, and their anesthesia was initiated with a dose of propofol (2 - 3 mg/kg) and fentanyl (0.5 g/kg) in the first 5 minutes, and it continued with 200 - 250 _g/dL of propofolper minute. Then, the orotracheal intubation was performed. During the surgery, their applicable ringer’s solution was 20 cc/kg. The surgery was conducted using the four-port technique, i.e., a 10-mm umbilical port, which was the first port that entered the abdomen with the aid of a port needle after pumping the gas into the abdomen, a 10- mm xiphoid port, a 5-mm mid-clavicular port at the Murphy point, and a5-mmmid-clavicular port in the adjacency of umbilicus. During the surgery, the intra-abdominal pressure was maintained by a maximum of 15 mmHg of carbon dioxide, and the patients were under continuous cardiac and Capnography monitoring. The patients’ blood samples were collected at three different time points, i.e., before the surgery (time point 1), 30 minutes after pumping the carbon dioxide gas into the abdomen (time point 2), and 30 minutes after removing the last port from the abdomen (time point 3). The blood samples taken in these time points were examined concerning daily BUN, Cr serum levels and then were transferred to a laboratory under a cold chain for further investigations [14]. It should be noted that the current study was carried out without a sexual preference (women), and steps mentioned in the anesthesia service reviews and the protocol of the American Society of Anesthesiologists were followed; hence, no preoperative preventive measure was taken. Furthermore, there were no indications for the Intraoperative injection of low-molecular-weight heparin (LMWH) and antibiotics. Time of surgery measured from starting induction of anesthesia for first step and second step from pumping the carbon dioxide gas into the abdomen. Finishing time is third step and gas exit from abdomen and forth step is extubation of patient.
3.5. Statistical Analysis:
Data analysis was performed using SPSS Ver.22 by repeated measures and Bonferroni follow-up test.
Before examining the research hypotheses, The Kolmogorov-Smirnov test was applied to test for a normal distribution, which indicated the normality of all variables, as the significance values of the normality tests were greater than 0.05. In addition, the assumption of equal variances was examined for each variable by Levene’s test, which resulted in significant levels for all investigated variables. Hence, the assumption of equal variances was observed.
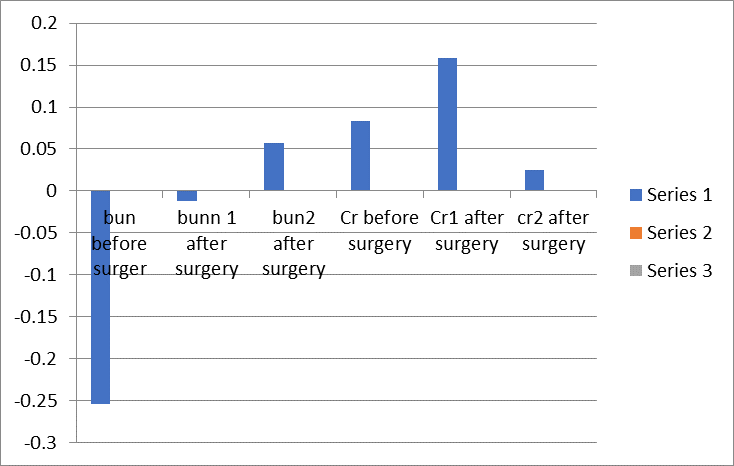
Figure 1: Time- Changes of BUN and Cr on SD (p<0>
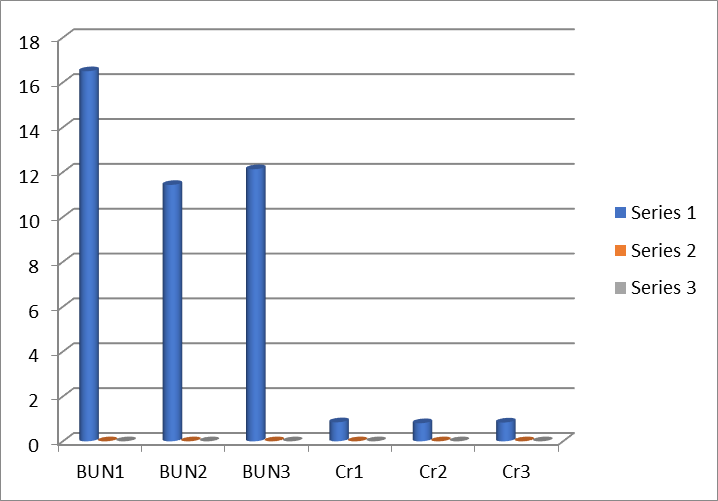
Figure 2: Changes of BUN and Cr on Mean (p<0>
It shows that BUN can be affected by laparoscopic surgery and it is significant.
It shows that Cr can be affected by laparoscopic surgery but it is not significant.
Timing:
First time to second, third and fourth time relationship was measured. The mean time between one and four is 98 minutes and mean between two
and three is 81 minutes. Mean time between one, two, three and four measured and this time compare with Renal function tests.
First time: Start anesthesia
Second time: start gas insufflation
Third time: exit the gas
Forth time: extubation of patient
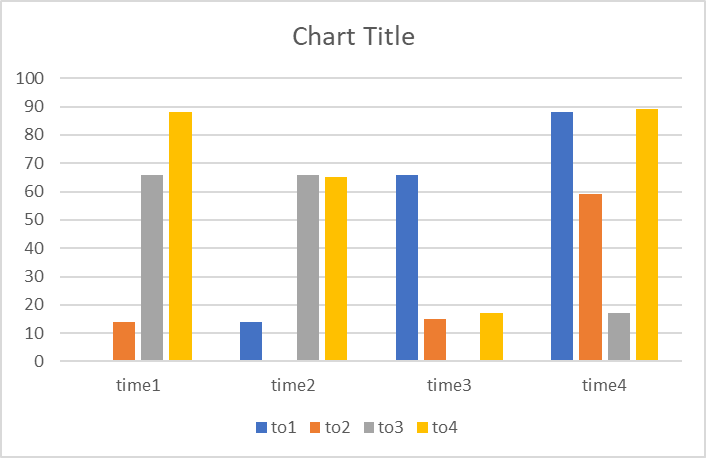
Figure 3: Changes of time on Mean (minutes)
It shows it is not correlation between duration of a surgery from beginning to finishing on renal function tests.
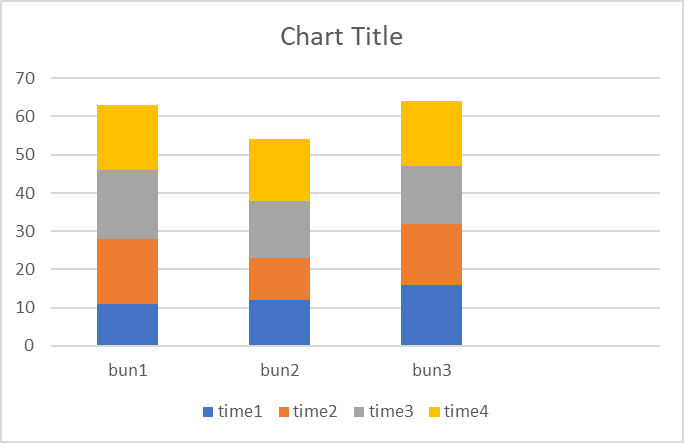
Figure 4: Changes BUN in time on Mean (minutes) (p<0>
It shows it is not correlation between duration of a surgery from beginning to finishing on BUN.
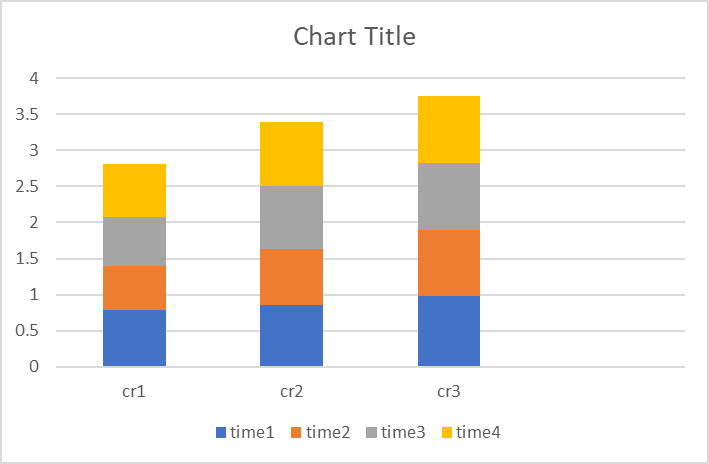
Figure 5: Changes Cr in time on Mean (minutes) (p<0>
It shows it is not correlation between duration of a surgery from beginning to finishing on Cr.
Time and duration of surgery cannot effect on renal function tests.
This study demonstrated that the Laparoscopic cholecystectomy surgery was only effective in changing (i.e., increasing) the BUN and did not have any significant effects on Cr. Bun changes can be affected by low protein diet, dehydration before or during surgery. Pneumoperitoneum during laparoscopy results in transient Oliguria and decreased glomerular filtration and renal blood flow. The presence of oliguria and elevated serum creatinine is suggestive of acute renal injury. Serum cystatin C has been described as a new marker for the detection of this type of injury. In this study, our aim was to compare the glomerular filtration rate estimated using cystatin C levels with the rate estimated using serum creatinine in patients with normal renal function who were undergoing laparoscopic surgery. [20] Thus, except for the impacts of Pneumoperitoneum on portal vein flow due to liver functions and their related in inflammatory responses, some intervening factors, such as age, BMI, surgery duration, and surgical injuries, affect (either directly or indirectly) can change the BUN. Accordingly, patients with risk factors such as senescence, obesity, or a long wait for laparoscopic surgery, are likely to have significant coagulation activations. They are considered a high risk group who are prone to the development of deep vein thrombosis following the surgery, which certainly causes a kind of Thromboprophylaxis. In this regard, laparoscopic surgery activates the coagulation and Bronchiolitis pathways and changes the height of the bTG and coagulation tests. It is necessary to mention some limitations and biases of our study. Firstly, not having the opportunity to assess the functions of the pancreas and other organs in the abdomen during the surgery, due to its high cost. Secondly, not having the chance to examine the functions of the organsafter the surgery to evaluate postoperative changes. Thirdly, all participants of the present study were females who none of them was admitted to public hospitals. But sometimes Laparoscopy induced AKI is related with both hormonal stimuli for renal vasoconstriction and increased intra-abdominal pressure, causing hypoxemia and tubular renal injury. In conclusion, very few cases of laparoscopy induced AKI in young patients with no previous renal disease have been reported. Surgeons must consider this complication in the differential diagnosis of postoperative AKI [19]. As old patients are more prone to have pre-existing renal dysfunction, these patients are at increased risk of renal complications associated with laparoscopic surgery. In addition, living kidney donors are commonly operated via a laparoscopic approach. The effects of laparoscopy on renal hemodynamic and their potential consequences on kidney function should therefore be acknowledged by nephrologists.[18]. As in Previous researches Laparoscopic cholecystectomy have no effects on coagulation and Liver function tests [21]. Time and duration of surgery cannot effect on renal function tests. It Shows nowadays this way is Safe and useful but more researches is needed [22]. Opioid-free anesthesia as a part of multimodal analgesia and a new anesthesiology technique is a safe procedure, where opioid-related negative effects in patients undergoing elective laparoscopic cholecystectomy are avoided [23]. Residents' operative time improves as experience with LC increases. These improvements become more profound after adjusting for the seniority of the Teaching assistant [24]. The mean length of hospital stay after surgery was significantly longer in patients operated by residents [25]. Laparoscopic cholecystectomy with the participation of residents is safe, even in their first years of training. There is an additional cost of about 10% in the treatment of patient operated with the participation of first-year residents. There was no significant difference in the cost of the group operated by second-year residents [26]. Resident involvement in LC with different degrees of complexity did not affect postoperative outcomes. The participation of a resident as operating surgeon is not an independent risk factor and may be considered ethical, safe, and reliable whenever implemented in the background of a residency-training program with continuous supervision and national accreditation. The sum of other procedures not related to a LC should be taken as a risk factor of morbidity [27]. Study demonstrates that in selected patients, senior residents can safely perform LC when supervised by senior staff surgeons [28]. Significant variation exists between documentation between resident and attending cholecystectomy consents, with residents including more complications than attendings on their consent forms. These data suggest that experience alone does not predict content of written consents, particularly for common ambulatory procedures. Education regarding the purpose of informed consent and what should be included in one may lead to a reduction in variability between providers [29]. Surgeon's demographics, personal experiences, and specialty appear to significantly influence their teaching styles and the educational experience residents receive regarding informed consent [30].
LC is safe in children and, although most complications are minor, almost 1/5 complications require interventions, mostly due to bleeding and biliary tree complications. Mortality has not been reported in pediatric LC (31). The evolution of cholecystolithiasis in the pediatric population can present serious complications, emphasizing the need to avoid temporizing cholecystolithiasis in children and adolescents because laparoscopic cholecystectomy in this group is safe, with low complication rates (32).
Variations of the hemocoagulative parameters in patients undergoing laparoscopy are still a matter of study (33).
Ethical Approval and Consent to participate:
The content of this manuscript are in accordance with the declaration of Helsinki for Ethics. No committee approval was required. Oral and written consent to participate is granted by the patient families.
Consent for publication:
“Written informed consent was obtained from the patient's legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.”
Availability of supporting data
It is available.
Competing interests:
The author declares that they have no competing financial interests and nothing to disclose.
Funding:
Zahedan University of Medical Sciences.
The authors have no conflicts of interests to declare.
Ahmad Reza Shahraki is the surgeon of patient and writes this paper.
Ali Reza Khazy assists the surgery, Mehdi Mohammadi calculate statics, Elham Shahraki involved in patient examination and Inclusion and Exclusion Criteria, Elahe Shahraki participate in collecting data's , Abbas Ali Niazi did the Lab exams, Hamide Mirshekari and Mohammad Reza Shahraki edit paper.
Generally, it can be argued that despite observing some variations in the BUN test during the laparoscopic surgery, the Cr level did not change and timing have no effects on them, Hence it can be considered as a safe surgical intervention for renal and liver functions.