AUCTORES
Globalize your Research
Review Article | DOI: https://doi.org/10.31579/2639-4162/249
Intensive Care Department, Faculty of Medicine, Military Medical Academy, Armed Forces College of Medicine, Egypt.
*Corresponding Author: Yahya Abdel Tawab Mohammed Meky, Intensive Care Department, Faculty of Medicine, Military Medical Academy, Armed Forces College of Medicine, Egypt.
Citation: Yahya Abdel Tawab Mohammed Meky, (2024), The Association Between Thyroid Hormone Levels and Mortality Outcomes Among Sepsis and Septic Shock Patients, J. General Medicine and Clinical Practice, 7(20); DOI:10.31579/2639-4162/249
Copyright: © 2024, Yahya Abdel Tawab Mohammed Meky. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 06 December 2024 | Accepted: 20 December 2024 | Published: 23 December 2024
Keywords: thyroid hormones; sepsis; prognostic marker; FT3 (free triiodothyronine); FT4 (free thyroxine)
Background: Sepsis is a life-threatening condition triggered by an overwhelming immune response to infection. It significantly contributes to global morbidity and mortality. Thyroid hormone imbalances are prevalent in critically ill patients and can exacerbate metabolic dysfunction and worsen clinical outcomes. Further investigation into these connections is crucial for improved patient care.
Objectives: to study the relationship between thyroid hormone levels at baseline and outcomes of Sepsis and Septic Shock in critically ill patients.
Patients and methods: This observational, cross-sectional study was conducted in the general ICU at Maadi Military Medical Hospital, involving 62 critically ill patients with sepsis or septic shock. Patients aged 18 and older with culture-confirmed infections were included. Individuals with preexisting thyroid or cardiovascular conditions were excluded from the study.
Results: mean age of 52.3 years, a gender distribution that is about equal, and common comorbidities including diabetes (25.8 percentage) and hypertension (43.5 percentage). Thyroid hormone levels were greater in survival, and the mortality rate was 50 percentage (FT3, FT4). With an AUC of 0.886, FT3 showed a significant mortality prediction. Thyroid hormone levels, organ function, and infection all affect patient outcomes and are important indicators of prognosis in critical care settings.
Conclusion: The study highlights the strong association between thyroid hormone levels, particularly FT3, and patient outcomes in critically ill patients with sepsis and septic shock. Lower levels of FT3 and FT4 were linked to increased disease severity, prolonged ICU stays, and higher mortality rates. Notably, FT3 emerged as a particularly strong predictor of mortality. These findings suggest that monitoring thyroid hormone levels may be valuable in identifying high-risk patients and guiding therapeutic interventions to improve clinical outcomes in this patient population.
A dysregulated host response to infection results in organ failure and sepsis, a potentially fatal illness. Sepsis killed about 11 million people worldwide in 2017 and had a death rate close to 20% (Rudd et al., 2020). Sepsis is still a serious public health concern due to its rising occurrence, especially since each case can cost more than $27,000 to treat (Arefian et al., 2017; Dietz et al., 2017).
Particularly in times of stress and serious illness, thyroid hormones play an essential role in controlling metabolic processes (Lodha et al., 2007). Hospitalized individuals frequently have abnormal thyroid hormone levels, especially those who are elderly or unwell (Iglesias et al., 2009). Researchers are focusing more on how systemic disorders affect thyroid metabolism, which can result in conditions like euthyroid sick syndrome (NTIS) or low T3 syndrome (Liu et al., 2016). Low triiodothyronine (T3) levels are commonly seen in sepsis, which is explained by enhanced thyroxine (T4) conversion to reverse T3 and increased T3 catabolism (Warner and Beckett, 2010). In the intensive care unit (ICU), these modifications may have a negative impact on patient outcomes (Pérsico et al., 2023). Studies indicate that free T3 may predict death in intensive care unit patients, highlighting the connection between thyroid hormone levels and the severity of sepsis (Wang et al., 2012). To fully comprehend the predictive significance of thyroid hormone levels, particularly in patients suffering from septic shock, more investigation is necessary (Sun, Bao, and Guo, 2023). Furthermore, thyroid dysfunction can affect cardiac health; alterations in the duration of the QT interval are associated with both hyperthyroidism and hypothyroidism, which may result in severe arrhythmias (Wang, 2022). To demonstrate the vital role thyroid hormones, play in metabolic adaptation during critical illness, this study intends to examine the association between thyroid hormone levels and outcomes in critically sick patients suffering from sepsis and septic shock. This study sought to determine how baseline thyroid hormone levels and outcomes in critically sick patients with sepsis and septic shock relate to one another. It aims to ascertain whether these hormone levels might function as prognostic markers, which could impact treatment choices and enhance patient outcomes in critical care environments.
The Maadi Military Medical Complex's general intensive care unit will be the site of this cross-sectional, analytical, and observational study. Patients with sepsis or septic shock who are in critical condition are part of the study population.
Inclusion Criteria:
Patients who match the diagnostic criteria for sepsis/septic shock as stated in the Sepsis and Septic Shock 3.0 guidelines published in 2016 and who are over 18 years old and admitted to the intensive care unit (ICU) with infections that have been visually or culture-identified are eligible for inclusion (Rhodes et al., 2017). Studying the impact of thyroid disease on ECG measurements will only involve patients having sinus rhythm on the examined ECG.
Exclusion Criteria:
Exclusion criteria encompass:
Sampling:
The study will use a straightforward, non-probability sampling technique. T4 levels were considerably lower in non-survivor septic shock patients than in survivors, per earlier studies (Wang et al., 2021). It will take a minimum of 62 septic shock patients, comprising at least 31 survivors and 31 non-survivors, to obtain a significant comparison of thyroid hormone levels between survivor and non-survivor groups with a power of 80% and a significance threshold of 0.05.
Data Collection Tools and Procedure:
Sociodemographic Information: Details on the demographics of the patients was gathered.
Medical History: A thorough medical history was documented, with a focus on drug use and any thyroid conditions.
Clinical Examination: Vital sign assessments (heart rate, respiration rate, blood pressure, and temperature) were part of the comprehensive clinical examination that patients will get. Cultures: Upon admission, pan cultures (blood, sputum, urine, or other probable infection sites) were obtained.
Laboratory Indicators: Complete blood count, albumin levels, lipid profile, cardiac enzymes, liver function tests, and kidney function tests were all be blood draws on the first day of intensive care unit admission.
Blood Gas Analysis: A multi-function blood gas analyzer will be used to do blood gas analysis, which includes measuring lactate levels.
Thyroid Hormone Measurement: Enzyme-linked immunosorbent assay (ELISA) kits are used to test thyroid hormone levels (FT3, FT4, and TSH) from blood samples obtained upon admission and five days thereafter.
Thyroid Function Types: Patients were classified as euthyroid, hyperthyroid, hypothyroid, or nonthyroidal sickness syndrome (NTIS) according to their baseline thyroid hormone levels.
Clinical Follow-Up: Throughout their ICU stay, patients have their clinical status evaluated for any signs of progress or decline.
Scoring Systems: The sequential organ failure assessment score (SOFA) was evaluated every day, and the acute physiology and chronic health evaluation II score (APACHE II) was finished within 24 hours of ICU admission.
Instruments: ECG: Daily monitoring for arrhythmias or ischemic changes and Echocardiography: Baseline assessment and follow-up during the ICU stay.
Outcomes of the study
They used SPSS v26 (IBM Inc., Chicago, IL, USA) for statistical analysis. The normality of the data distribution was assessed using histograms and the Shapiro-Wilks test. An unpaired Student's t-test was used to compare the two groups' quantitative variables, which were expressed as mean and standard deviation (SD). Quantitative data were evaluated using t-tests or ANOVA, while qualitative variables were reported as frequency and percentage (%) and, when applicable, the Chi-square test. Statistical significance was defined as a two-tailed P value < 0>
A flowchart of the study children is shown in Figure 1. Of the 69 critically ill patients with sepsis or septic shock who attended the general ICU at Maadi Military Medical Hospital,13 patients were excluded from the study (5 of them did not meet the inclusion criteria and 2 declined consent), 62 patients consented to participation (Figure 1).
The demographic characteristics of the 62 studied patients show a near-equal gender distribution, with 48.4 percentage males and 51.6 percentagefemales (Table 1). Also, the mean and range of vital signs for the studied patients were presented in table 1.

Figure 1. Flowchart of the studied patients’ groups.
| Studied Patient (n=62) | |||
| N | percentage | ||
| Gender | Male | 30 | 48.4 |
| Female | 32 | 51.6 | |
| Mean ±SD | Range | ||
| Age/year | 52.3 ± 14.5 | 35 – 70 | |
| Height (Cm) | 162.8 ± 9.2 | 156 – 179 | |
| Weight (Kg) | 85.5 ± 11.2 | 54 – 101 | |
| BMI (Kg/m2) | 26.7 ± 7.1 | 22 – 35 | |
| Heart Rate (beat/min.) | 110.08 ± 10.73 | 85 – 120 | |
| Respiratory Rate (Breath/min.) | 22.02 ± 2.92 | 14- 30 | |
| Mean Arterial Blood Pressure (mmHg) | 60.86 ± 9.60 | 55- 70 | |
| Temperature (Co) | 37.01 ± 0.51 | 35.99 - 38.93 | |
Table 1: Demographic Data and Vital Signs of the studied patients.
Among the 62 patients studied, 59.7 percentage were diagnosed with sepsis, while 40.3 percentage were in septic shock. This distribution highlights the severity of the condition within the cohort, with a significant portion progressing from sepsis to the more critical state of septic shock (Figure 2).

Figure 2: Distribution of Sepsis and Septic Shock among Studied Patients.
The severity of illness among the 62 studied patients is reflected by their APACHE and SOFA scores. The mean APACHE score is 35, with a range from 20 to 65, indicating a high level of critical illness, as higher APACHE scores are associated with increased mortality risk. The SOFA score, which measures organ dysfunction, has a mean of 16, ranging from 10 to 22 (Table 2).
| Studied Patients (n=62) | |||
| Mean ±SD | Range | ||
| APACHE Score | 35 ± 7.99 | 20- 65 | |
| SOFA Score | 16 ± 2.89 | 10 - 22 | |
| N | percentage | ||
| Mechanical ventilation | Yes | 25 | 40.3 |
| No | 37 | 59.7 | |
| Mechanical ventilation/hrs. | 49.05 ± 21.91 | 3.20 - 92.50 | |
| ICU | Survive | 31 | 50.0 |
| Non-Survivor | 31 | 50.0 | |
| ICU Length of stay/days | 10.91 ± 4.61 | 0.17 - 20.83 | |
Table 2: Mortality and Outcomes among the studied patients.
In this study, FT3 and FT4 levels were significantly lower among patients with mechanical ventilation (2.94 ± 0.90, 0.87 ± 1.12) compared to patients without mechanical ventilation (5.23 ± 2.03, 1.21 ± 0.65), (p˂0.05). while TSH was not significantly different among patients with and without mechanical ventilation (p=0.429), (Table 3).
| Mechanical Ventilation | Test value | P-value | |||
| Yes (n=25) | No (n=37) | ||||
| FT3 (pg/mL) | Mean ±SD | 2.94 ± 0.90 | 5.23 ± 2.03 | 5.274 | <0> |
| Range | 1.4 – 5.0 | 2.0 – 9.2 | |||
| FT4 (pg/mL) | Mean ±SD | 0.87 ± 1.12 | 1.21 ± 0.65 | 2.045 | 0.047* |
| Range | 0.17 – 2.40 | 0.20 – 3.0 | |||
| TSH (µIU/mL) | Mean ±SD | 0.98 ± 0.62 | 1.12 ± 0.67 | 0.797 | 0.429 |
| Range | 0.17 – 2.0 | 0.17 – 2.30 | |||
Using: t-Independent Sample t-test for Mean ±SD; X2= Chi-Square test, p-value >0.05 is insignificant; *p-value <0>
Table 3: Thyroid hormone levels in patients with and without mechanical ventilation.
In this study, Thyroid hormone levels were analyzed across survivors and non-survivors at two time points (Day 0 and Day 7). Initial FT3 levels showed no significant difference (p=0.198), but by Day 7, non-survivors exhibited significantly higher FT3 levels (p=0.002). FT4 levels followed a similar pattern, with a significant elevation in non-survivors by Day 7 (p=0.010). TSH levels remained comparable between groups at both time points, (Table 4).
| 0 Day | 7 Day | |||||
| Survive (n=31) | Non-Survivor (n=31) | P value | Survive (n=31) | Non-Survivor (n=31) | P value | |
| FT3 (pg/mL) | 2.79(1.1-4.8) | 3.24(1.8-5.0) | 0.198 | 3.91(2.4-9.2) | 2.96(1.4-5.0) | 0.002** |
| FT4 (pg/mL) | 0.97(0.2-2.0) | 1.01(0.2-2.9) | 0.770 | 1.22(0.3-3.0) | 0.81(0.17-2.4) | 0.010** |
| TSH (µIU/mL) | 1.1(0.3-2.0) | 1.02(0.18-4.0) | 0.657 | 1.14(0.3-2.3) | 0.99(0.17-2.0) | 0.365 |
Using: t-Independent Sample t test for Mean ±SD; X2= Chi- Square test, p-value >0.05 is insignificant; *p-value <0>
Table 4: Thyroid hormone levels in ICU survivors and non-survivors.
In our study, thyroid hormone levels correlated significantly with clinical parameters. Lower FT3 and FT4 levels were associated with higher APACHE and SOFA scores, prolonged ICU stays, and increased reliance on mechanical ventilation and CRRT. Negative correlations between FT3 and age, BMI, and organ dysfunction further support the role of thyroid hormones as markers of severity, (Table 5).
| FT3 | FT4 | TSH | ||
| Age | R | -0.150 | -0.110 | -0.093 |
| P-value | 0.038* | 0.091 | 0.132 | |
| Gender | R | 0.050 | 0.020 | 0.056 |
| P-value | 0.210 | 0.326 | 0.294 | |
| BMI | R | -0.145 | -0.125 | 0.030 |
| P-value | 0.041* | 0.074 | 0.388 | |
| Diabetes | R | 0.025 | 0.014 | 0.045 |
| P-value | 0.400 | 0.472 | 0.225 | |
| Hypertension | R | -0.130 | -0.085 | 0.010 |
| P-value | 0.060 | 0.145 | 0.482 | |
| IHD | R | -0.160 | -0.112 | -0.040 |
| P-value | 0.032* | 0.089 | 0.242 | |
| CKD | R | -0.170 | -0.142 | 0.010 |
| P-value | 0.027* | 0.042* | 0.473 | |
| Bed Sores | R | 0.030 | -0.060 | 0025 |
| P-value | 0.370 | 0.282 | 0.406 | |
| Liver Cirrhosis | R | 0.038 | 0.014 | 0.025 |
| P-value | 0.300 | 0.470 | 0.406 | |
| APACHE Score | R | -0.270 | -0.152 | -0.091 |
| P-value | 0.032* | 0.046* | 0.348 | |
| SOFA Score | R | -0.280 | -0.143 | -0.089 |
| P-value | 0.029* | 0.269 | 0.441 | |
| Continuous renal replacement therapy | R | -0.150 | 0.132 | 0.040 |
| P-value | 0.038* | 0.062 | 0.242 | |
| QT interval | R | -0.180 | -0.150 | 0.060 |
| P-value | 0.028* | 0.048* | 0.275 | |
| Duration of vasopressor therapy | R | -0.160 | -0.105 | 0.055 |
| P-value | 0.033* | 0.085 | 0.288 | |
| Mechanical ventilation | R | -0.130 | -0.150 | -0.142 |
| P-value | 0.073 | 0.038* | 0.044* | |
| ICU Length of stay | R | -0.250 | -0.156 | 0.080 |
| P-value | 0.030* | 0.030* | 0.177 | |
Using: r: spearman correlation coefficient, p-value >0.05 is insignificant; *p-value <0>
In this study, there was no significant difference between survivors and no-survivor patients regarding gender (p=0.412). However, most of the survivors aged lower than 52 years (n=24,77.42 percentage) versus non-survivors most of them aged above 52 years old (n=24,77.42 percentage), (p=0.046). Also, most of the survivors had BMI lower than 26.7 kg/m2 (n=22,70.97 percentage) versus non-survivors most of them had BMI ≥26.7 kg/m2 (n=22,70.97), (p=0.0492), (Figure 3).

Figure 3: Comparison between survivors and non-survivors as regards demographic data.
In this study, there was no significant difference between sepsis and septic shock patients regarding FT4 (p=0.164) and TSH (p=0.50). However, FT3
levels were significantly increased among sepsis patients (4.15 ± 1.92) than septic shock patients (3.52 ±2.14), (p=0.011), (Table 6).
| Sepsis (n=37) | Septic shock (n=25) | P-value | ||
| FT3 (pg/mL) | Mean ±SD | 4.15 ± 1.92 | 3.52 ± 2.14 | 0.011* |
| Range | 1.4 – 8.4 | 0.9 – 5.6 | ||
| FT4 (pg/mL) | Mean ±SD | 1.25 ± 0.68 | 0.83 ± 0.54 | 0.164 |
| Range | 0.17 – 3.0 | 0.18 – 2.0 | ||
| TSH (µIU/mL) | Mean ±SD | 1.11 ± 0.65 | 1.00 ± 0.64 | 0.500 |
| Range | 0.17 – 2.3 | 0.17 - 2.0 | ||
Table 6: Comparison of thyroid hormone levels between sepsis and septic.
The prognostic utility of thyroid hormones was further evaluated through ROC curve analysis. FT3 showed excellent predictive value for mortality (AUC: 0.886, p<0 href="file:///C:/Users/DELL/Downloads/%">percentage) and specificity (67.7 percentage). FT4 demonstrated moderate accuracy (AUC: 0.749, p=0.001), while TSH had limited diagnostic value (AUC: 0.572, p=0.331), (Table 7, Figure 4).
| Cut off | AUC | Sensitivity (percentage) | Specificity (percentage) | PPV (percentage) | NPV (percentage) | P-value | |
| FT3 | 2.55 | 0.886 | 93.5 | 67.7 | 97.2 | 80.0 | <0> |
| FT4 | 0.85 | 0.749 | 80.6 | 38.7 | 87.2 | 62.7 | 0.001** |
| TSH | 0.95 | 0.572 | 58.1 | 54.8 | 71.5 | 42.8 | 0.331 |
Table 7: ROC Curve for Thyroid hormones as a predictor of mortality.
The diagnostic performance of FT3, FT4, and TSH as predictors for mortality was evaluated using ROC curve analysis.
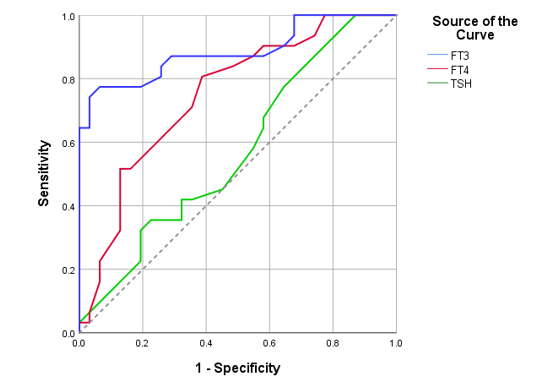
Figure 4: ROC Curve for Thyroid hormones as a predictor of mortality.
As complex clinical diseases with high death rates, sepsis and septic shock continue to present major problems in intensive care units (ICUs) around the world (Langouche et al., 2019). According to Arina and Singer (2021), sepsis occurs when an infection sets off a dysregulated host response that leads to extensive inflammation and organ failure. Significant circulatory, cellular, and metabolic problems accompany the progression to septic shock, which increases the chance of death. For the management and improvement of outcomes in critically sick patients, early detection of the severity of sepsis and an accurate prognosis are essential (Pérsico et al., 2021).
Thyroid hormones' important effects on immunological modulation, metabolic regulation, and cardiovascular function have drawn attention to their significance in the body's reaction to critical disease (Wang et al., 2021). Non-thyroidal illness syndrome (NTIS) is the collective term for the endocrine changes that occur in the body during severe illness, including changes in thyroid hormone levels. Thyroid-stimulating hormone (TSH) levels are frequently stable or repressed in conjunction with decreased levels of free triiodothyronine (FT3) and, in extreme situations, free thyroxine (FT4) in the blood. According to Teixeira et al. (2020), these alterations are believed to be adaptive means of preserving energy in times of extreme stress. Establishing baseline thyroid hormone levels (FT3, FT4, and TSH) in critically sick patients with sepsis and septic shock was the goal of this study to give an early evaluation of endocrine function. It also investigated the connection between thyroid hormone levels and clinical outcomes, such as
mortality rates, acute kidney injury, length of intensive care unit stays, duration of mechanical ventilation, changes in QT intervals (a measure of cardiac repolarization), and the occurrence of complications like bedsores, thromboembolism, and infections. With an average age of 52.3 years, a sample of 62 sepsis patients, virtually evenly split by gender (48.4 percentage male, 51.6 percentage female), included middle-aged to older adults. Their average body mass index (BMI) was 26.7 kg/m2, suggesting that obesity is a common condition associated with poor sepsis outcomes. The prevalence of chronic diseases such as diabetes (24.8 percentage) and hypertension (43.5 percentage) underscore the possible influence of underlying comorbidities on the development of sepsis. The fact that 40.3 percentageof the individuals had septic shock and 59.7 percentage had sepsis highlights the seriousness of the condition and the elevated risk of sequelae in this group. The study emphasized how baseline characteristics including age, weight, and chronic diseases affect sepsis outcomes, which is consistent with findings by Sun et al. (2023). Comorbid conditions such as diabetes and hypertension, together with obesity, might worsen metabolic instability and cardiovascular risks, which can affect the outcome of sepsis and septic shock. Additionally, the high percentage of septic shock (40.3 percentage) in this study is consistent with findings that highlight poor outcomes and systemic complications in intensive care unit patients.
This emphasizes how crucial it is to take metabolic and physiological indicators into account when predicting the severity and mortality of sepsis. Indicative of successful ICU respiratory treatment, blood gas analysis revealed constant respiratory function (average CO₂: 40.07 mmHg, HCO₃: 24.29 mmol/L, SPO₂: 98.62 percentage). Hematological and organ function indicators, such as leukocyte counts and creatinine levels, are crucial for determining the severity of sepsis, according to Sun et al. (2023). These results, together with the study's steady respiratory values, highlight the significance of focused intensive care unit interventions in enhancing respiratory outcomes and controlling organ stress-related problems.
Both survivors and non-survivors had their thyroid hormone levels measured at two different times (Day 0 and Day 7). There was no discernible variation in the first FT3 levels (p=0.198), However, non-survivors' FT3 levels were much greater by Day 7 (p=0.002). FT4 levels showed a similar trend, with non-survivors showing a significant increase by Day 7 (p=0.010). At both time points, the groups' TSH levels were similar. These results imply that the severity of sepsis and mortality risks may be reflected over time by dynamic variations in FT3 and FT4 levels rather than baseline values. Sun et al. (2023) and Angelousi et al. (2011) highlighted the predictive significance of thyroid hormone levels, which corroborated these findings. Poor outcomes are associated with low FT3 and FT4 levels in sepsis patients, especially in cases of severe septic shock. Additionally, Wang et al. (2021) emphasized the link between low FT4 levels and a poor prognosis, confirming the usefulness of thyroid hormones as biomarkers for critical illness.
Also, SOFA and APACHE scores offered important information about the severity of the illness. The SOFA score of 8.02 (SD ±2.89) and the mean APACHE score of 24.20 (SD ±4.44) both pointed to moderate to severe critical illness with substantial organ failure. These scores, which are frequently used to gauge the chance of survival and direct the level of intensive care unit care, were substantially linked to poorer results. In line with these findings, Sun et al. (2023) showed a strong link between higher mortality in septic shock patients and higher APACHE and SOFA scores. These results are consistent with the current study's focus on how useful these scores are for risk stratification and intervention customization.
Also, 17.7 percentage of patients in the analysis of intensive care unit interventions needed continuous renal replacement therapy (CRRT), suggesting severe renal impairment. Some patients had prolonged QT intervals (mean: 420.65 ms, SD ±42.67), which suggested that their hearts were under stress from serious disease or drugs. The length of vasopressor medication varied, indicating varying levels of circulatory instability (mean: 76.98 hours, SD ±26.90). Liu et al. (2021) documented comparable results, emphasizing the correlation between elevated vasopressor reliance in septic shock, longer ICU stays, greater SOFA scores, and low FT3 and FT4 levels. This study confirms that effective management of critical sepsis requires monitoring of cardiovascular, endocrine, and renal parameters.
There was a substantial correlation between thyroid hormone levels and clinical indicators. Higher APACHE and SOFA scores, longer ICU stays, and a greater need for CRRT and mechanical ventilation were correlations with lower FT3 and FT4 levels. Further evidence for the function of thyroid hormones as severity indicators comes from negative associations found between FT3 and age, BMI, and organ dysfunction. These associations are consistent with research by Foks et al. (2019), Sun et al. (2023), and Liu et al. (2021), which showed that lower FT3 and FT4 levels are associated with severe organ dysfunction and increased use of resources in the treatment of sepsis.
ROC curve analysis was used to further assess the prognostic value of thyroid hormones. FT3 demonstrated great sensitivity (93.5 percentage) and specificity (67.7 percentage), as well as excellent predictive value for mortality (AUC: 0.886, p<0 p=0.331), p=0.001).>Bartolović et al. (2024) found that FT3 is a reliable indicator for ICU mortality risk categorization. The results of this study confirm the significance of FT3 in directing clinical judgments for patients with critically sick sepsis, with FT4 acting as a supportive indicator. To sum up, this study emphasizes how important thyroid hormones specifically FT3 and FT4 are in determining the severity of sepsis and forecasting its course. In addition to well-known instruments like APACHE and SOFA ratings, thyroid function markers offer important information for customizing ICU treatments. Given the adaptive yet complex nature of NTIS in critical illness, more study is necessary to examine the potential of thyroid hormone supplementation in improving clinical outcomes for patients in septic shock.
The study's findings demonstrated the predictive significance of thyroid hormone levels, specifically FT3 and FT4, in critically ill patients suffering from sepsis and septic shock. A longer ICU stay, a larger need for mechanical ventilation, increased severity, and a higher risk of death were all highly correlated with lower levels of FT3 and FT4. A particularly useful marker for mortality prediction, FT3's high sensitivity, and specificity suggest that it may be useful in early identification of high-risk individuals. TSH exhibited minimal relevance in evaluating both illness severity and death, despite FT4 likewise exhibiting moderate predictive power. According to these results, tracking FT3 and FT4 levels may help with clinical decision-making and risk classification for patients with sepsis and septic shock, enabling more specialized and prompt therapies to improve outcomes in this susceptible group.
Nil
Nil
Nil