AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2578-8868/379
National Brain Aneurysm & Tumor Center, Twin Cities, MN, USA
*Corresponding Author: Eric S. Nussbaum, National Brain Aneurysm & Tumor Center, Twin Cities, MN, USA.
Citation: Josef T. Nussbaum, Tariq M. Janjua, James K. Goddard, Eric S. Nussbaum, (2025), Tentorial Dural Arteriovenous Fistula Causing Severe Cervico-Medullary Venous Hypertension Mimicking Transverse Myelitis, J. Neuroscience and Neurological Surgery, 17(5); DOI:10.31579/2578-8868/379
Copyright: © 2025, Eric S. Nussbaum. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Received: 12 May 2025 | Accepted: 27 May 2025 | Published: 29 May 2025
Keywords: artery; arteriovenous fistula; brain; transverse myelitis; venous hypertension
Dural arteriovenous (AV) fistulae are uncommon lesions that can result in venous hypertension causing neurological dysfunction. We present the case of a young man who developed rapidly progressive, severe neurological symptoms resulting from a complex tentorial dural AV fistula initially mistaken for transverse myelitis. He was treated with intravenous steroid infusion and plasmapheresis and was discharged to a rehabilitation facility but returned to our hospital three weeks later with severe quadriparesis and difficulty breathing. Diagnostic angiography revealed a complex tentorial dural AV fistula involving the petrosal vein. The patient underwent microsurgical disconnection of the fistula and made an excellent subsequent recovery. Dural AV fistula represents a potentially reversible cause of neurological dysfunction. Imaging findings may be non-specific resulting in misdiagnosis; thus, a high index of suspicion for this pathological entity is important to allow for timely diagnosis and treatment. The diagnostic importance of catheter angiography is highlighted. Early treatment is associated with the best outcomes, but even patients with profound deficit may improve substantially, emphasizing the value of treatment despite advanced neurological deficit.
Dural arteriovenous (AV) fistulae are uncommon lesions that can result in venous hypertension leading to intracerebral hemorrhage or neurological dysfunction. [1-8] Patients with symptoms resulting from venous hypertension can present with non-specific neurological findings potentially complicating diagnosis. [9-10] We describe a young man who presented with rapidly progressing, severe neurological deficit which localized to the cervical spinal cord, some distance away from the site of the fistula which involved the tentorium. Magnetic resonance (MR) imaging abnormalities resulted in an initial incorrect diagnosis of and treatment for transverse myelitis (TM). After the patient worsened despite treatment for TM, catheter angiography revealed the true pathology, and the patient underwent microsurgical treatment of his fistula which ultimately resulted in an excellent neurological recovery. The diagnostic challenges associated with dural AV fistulae are discussed, and the potential reversibility of even severe neurological dysfunction in this setting is highlighted.
A 39-year-old man was evaluated at an outside hospital for progressive lower extremity numbness and weakness followed by upper extremity clumsiness. An MRI scan of the cervical spine demonstrated T2 signal change within the spinal cord involving the cervicomedullary junction (Figure 1A). A presumptive diagnosis of TM was made. Brain MR imaging revealed an incidental AV malformation of the occipital lobe, clearly not related to the patient’s symptoms. Lumbar puncture was unremarkable. The patient was started on steroids and underwent multiple rounds of plasmapheresis. He was sent to a rehabilitation facility.
One month later, the patient was admitted to our hospital with significant worsening of both upper and lower extremity function. He had a sensory level in the high thoracic region, was unable to void spontaneously, and was experiencing new respiratory difficulties. MRI demonstrated worsening of the signal changes within the spinal cord at the cervicomedullary junction (Figure 1B) but also showed increasingly prominent abnormal flow voids compatible with enlarged veins surrounding the brainstem and spinal cord (Figure 1C).
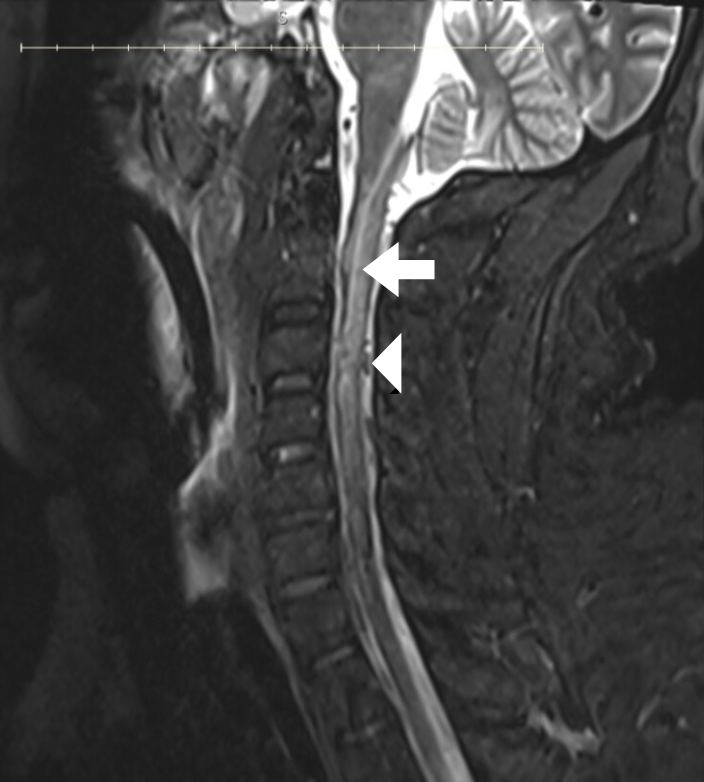
Figure 1A: Sagittal T2-weighted MR image of the cervical spine demonstrates abnormal signal change within the spinal cord (white arrow) extending from the cervicomedullary junction to the C6 level. There is some suggestion of prominent vessels (white arrowhead) dorsal to the spinal cord as well.
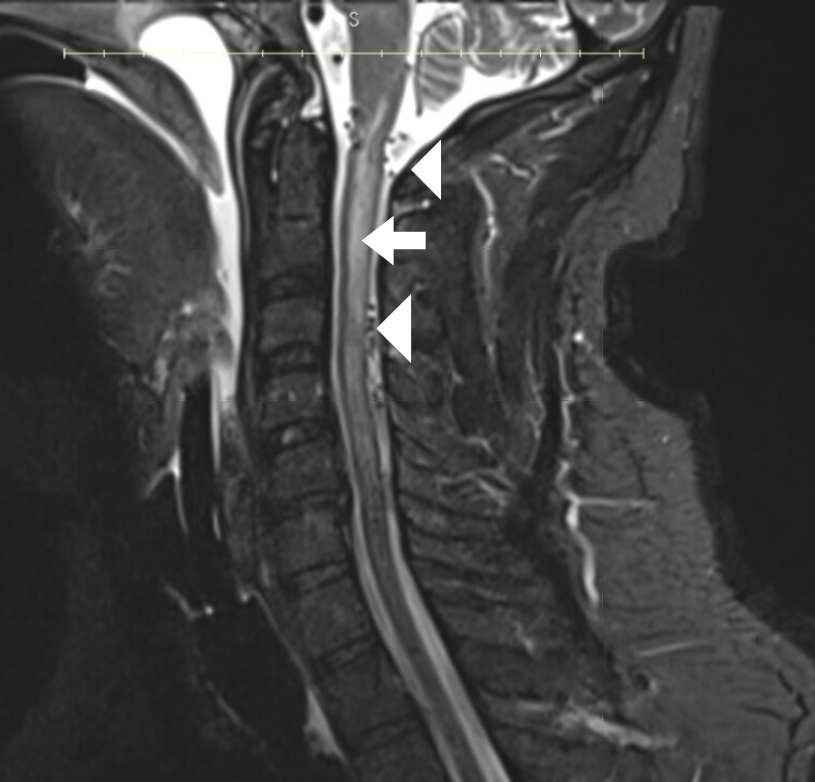
Figure. 1B: Comparable sagittal MR image obtained at the time of readmission after clinical worsening shows progression of the abnormal signal within the spinal cord (white arrow) which is more homogeneous as well as increased prominence of abnormal vessels dorsal to the cervical spinal cord and also surrounding the cervicomedullary junction (arrowheads).
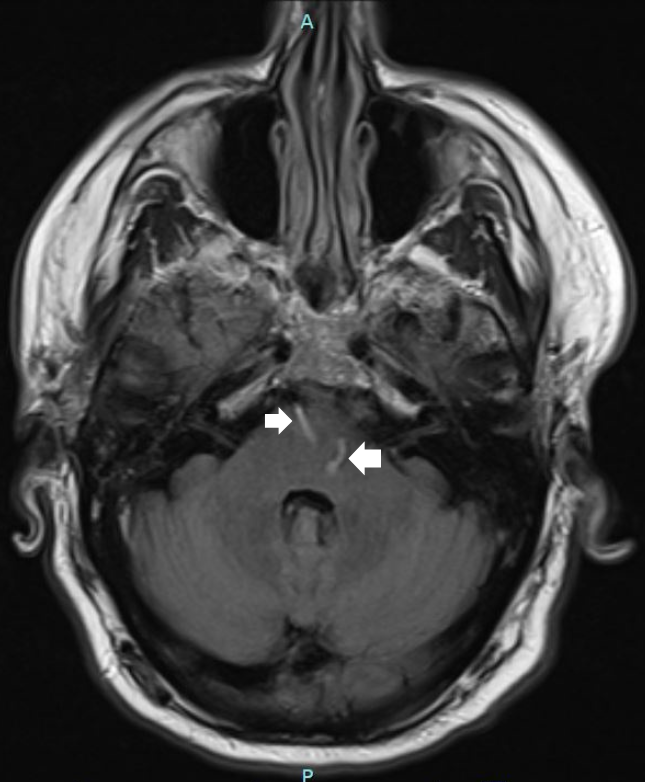
Figure 1C: Axial T-1 weighted MR image shows prominent veins (arrows) traversing the brainstem suggesting sluggish venous flow within the posterior fossa venous system.
An emergency diagnostic angiogram was performed revealing two distinct dural AV fistulae. The previously noted, supratentorial AV fistula involving the medial occipital lobe was seen and was felt to be an incidental finding, not contributing to the cervical spinal cord venous engorgement. In addition, a complex tentorial dural AV fistula with drainage through a dilated petrosal vein was identified, resulting in dramatic arterialization of the posterior fossa venous system (Figure 2) extending down to involve the cervicomedullary venous plexus. This second lesion was felt to be the cause of the patient’s existing neurological issues. Based on the presence of spinal perimedullary venous drainage, this fistula technically qualified as a Cognard-Merland Grade V lesion. [2]
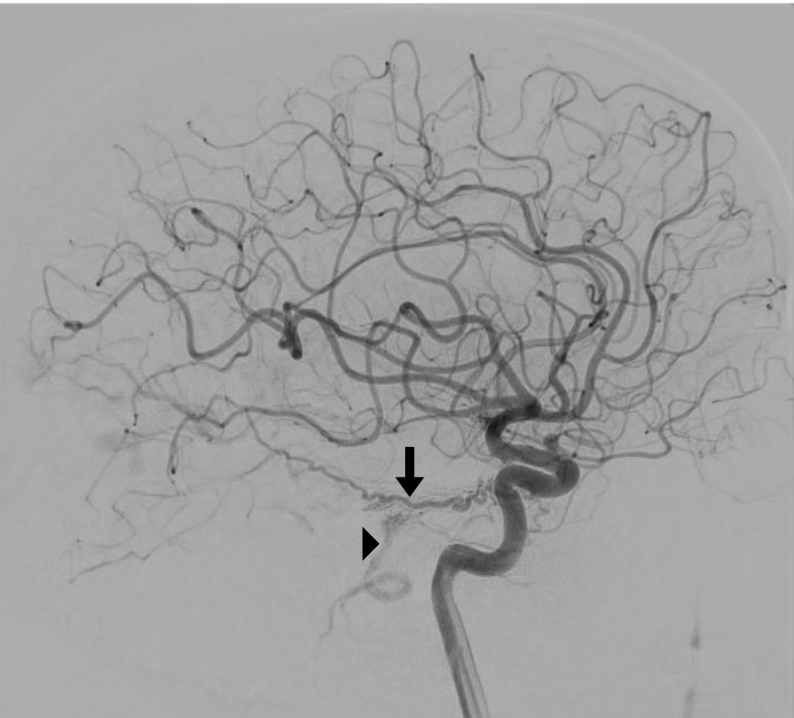
Figure 2. Lateral angiographic image of the internal carotid artery shows a dramatically dilated and tortuous tentorial artery (arrow) with the arrow indicating the site of the fistulous connection with the superior petrosal vein. An arrowhead points to the arterialized petrosal vein filling in “retrograde” fashion inferiorly towards the cervical spinal cord.
Based on the patient’s anatomy, the symptomatic lesion was not felt to be amenable to endovascular treatment, and microsurgical disconnection of the fistula was recommended. The patient was brought to the operating room on an emergency basis. He was placed in the three-quarter prone position and underwent a lateral suboccipital approach with disconnection of the fistula by sacrifice of the dilated and arterialized petrosal vein (Figures 3A and 3B). An intraoperative angiogram revealed obliteration of the AV fistula (Figure 4).
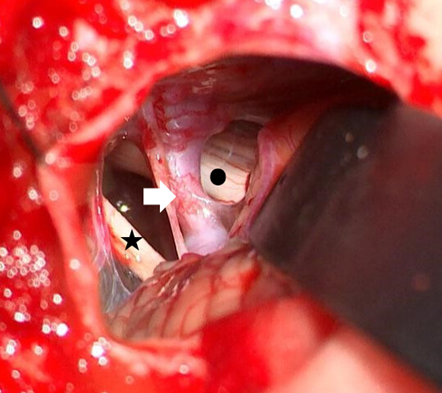
Figure 3A: Intraoperative photomicrograph shows the suboccipital craniotomy with a retractor on the cerebellum. The arterialized and dilated petrosal vein (white arrow), the VII-VIIIth nerve complex (star) inferiorly, and the fifth nerve (black dot) deep and superior to the vein are well visualized.
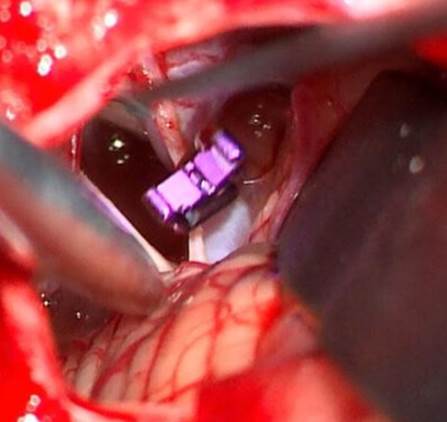
Figure 3b: Operative photomicrograph demonstrates an aneurysm clip which has been used to occlude the petrosal vein, interrupting the AV fistula.
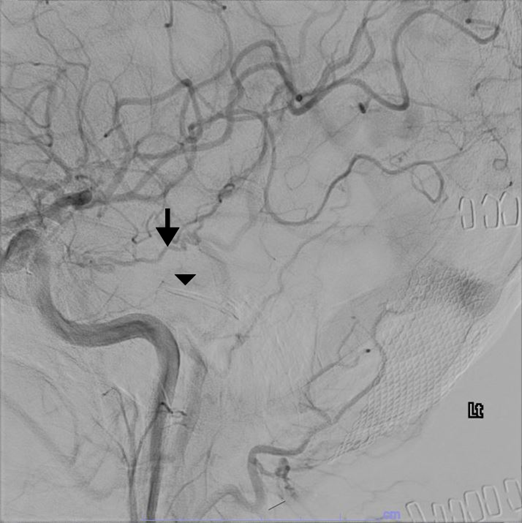
Figure 4: Intraoperative arteriographic image of the internal carotid artery shows immediate decreased filling of the tentorial artery (arrow) with the subtracted image of an aneurysm clip (arrowhead) which has been used to interrupt the AV fistula
The patient awoke with immediate improvement in his upper and lower extremity weakness and numbness. Over the ensuing month, he regained the ability to ambulate and void spontaneously. Cervical MRI scan approximately 6 weeks after surgery showed nearly complete resolution of the cervical cord edema as well as the abnormal venous flow voids around the brainstem and cervical spinal cord (Figure 5). At the time of three-month follow-up, he was ambulating well and his sensation was almost normal. Mild urinary symptoms persisted. His incidental supratentorial dural AV fistula was treated endovascularly without incident.
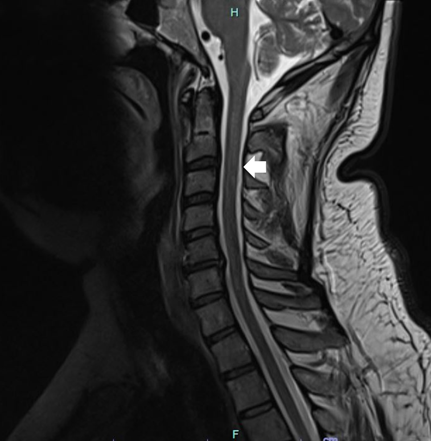
Figure 5: Postoperative sagittal T2-weighted MR image obtained six weeks after surgery demonstrates resolution of the abnormal signal within the spinal cord and absence of the previously visualized prominent venous channels around the cervical spinal cord and medulla (arrow).
Dural arteriovenous (AV) fistulae represent abnormal connections between the arterial and venous systems of the brain with the fistulae being located between the layers of the dura. [1-8]. The cause for dural AV fistula is not known, although prior dural sinus thrombosis, trauma, infection, radiation, or craniotomy have been identified as possible causes [1-8,11]. In most cases, no predisposing factor is found, although there may be an elevated risk in patients with conditions leading to a hypercoagulable state [12]. The finding of multiple concurrent dural AV fistulae in our patient suggests a possible relationship between the lesions. Dural AV fistulae are generally thought of as acquired lesions; however, the occurrence of multiple lesions in one patient occurs in 6-9% of cases. [12] In these instances, there may be a genetic predisposition, an underlying clotting disorder, or the lesions may share a common abnormal venous drainage pathway contributing to their development. [13,14]
Cranial dural AV fistulae can be divided based on whether or not they have recruited cortical venous drainage [1-16]. Lesions that do not have cortical venous drainage are considered “benign” and carry a low risk of hemorrhage or neurological dysfunction [15,16]. They can create pulsatile tinnitus and sometimes require treatment for symptomatic relief. In contrast, those lesions that drain through cortical veins are more dangerous and present a risk of intracerebral hemorrhage [15,16]. Alternatively, they can create a situation of venous hypertension with associated neurologic dysfunction as occurred in our case.
The treatment of dural AV fistulae can include observation, open microsurgery, endovascular therapy, or stereotactic radiosurgery. At times, these modalities are combined to offer the best outcome in complex cases [3-8, 11,15-19]. In our patient, there was no endovascular option based on the local anatomy, and microsurgical interruption of the fistula was chosen in the hopes of immediately normalizing the intracranial and intraspinal venous pressure. After surgery, the patient’s symptoms improved significantly within twenty-four hours.
In our case, the patient was initially misdiagnosed with transverse myelitis (TM), a focal inflammation of the spinal cord which generally leads to a symmetrical distribution of impairment affecting motor, sensory, and autonomic function. [20] Although typically idiopathic, TM can result as a postviral immune response or may ultimately prove to be the initial manifestation of an auto immune disorder such as multiple sclerosis. [21] Our patient underwent a standard treatment course for TM which generally involves high dose corticosteroids followed by plasmapheresis in the event of a poor clinical response. [22] Our patient’s progressive symptoms despite treatment resulted in his admission to our center where the diagnosis of dural AV fistula was made.
The immune-mediated inflammation of the spinal cord in TM yields non-specific radiographic findings, and TM is therefore considered a diagnosis of exclusion. [20] Similar imaging findings may be present in a wide array of disorders including multiple sclerosis, neuromyelitis optica, spinal cord infarction, and dural AV fistula. [21,23] Interestingly, dural AV fistula are often under-recognized despite being a leading cause of treatable progressive myelopathy in older adults. [23-24] Autoimmune paraneoplastic syndromes, although less frequent, may also present with longitudinally extensive cord lesions and can also be mistaken for TM. [25] While vascular etiologies such as dural AV fistula are frequently misdiagnosed, they should remain a high-priority consideration, especially in atypical or worsening cases
In our patient, initial imaging depicted a central T2 hyperintense lesion that was longitudinally extensive at the cervicomedullary junction without significant mass effect. The cervical location and central position were congruent with a TM diagnosis, and the absence of mass suggested inflammation as a likely explanation. [21] Nevertheless, retrospective review of the MR imaging displayed the subtle presence of abnormal flow voids which represented early evidence of underlying venous congestion.
Because neurological and imaging findings may be non-specific in these patients, a high index of suspicion must be maintained to facilitate timely diagnosis and treatment of dural AV fistula. As a result, such fistulae have been misdiagnosed as stroke, encephalitis, demyelinating disease, dementia, Parkinson’s, and multiple other degenerative neurological conditions. [9,10,26,27] In particular, dural AV fistulae can result in brainstem and spinal cord venous congestion producing a myelopathic picture, as in our patient. [28-33] The presence of any dilated veins, even remote from the site of a typical dural AV fistula should raise suspicion for this possible diagnosis. Although MRI/MRA have improved significantly, diagnostic catheter angiography remains the gold standard and is necessary to confirm the diagnosis and to plan treatment in patients with dural AV fistula.
Although prompt treatment carries the best chance for a favorable outcome, and patients with severe preoperative deficits may not recover as well as those with a short duration of less severe symptoms, it is important to remember that venous hypertension, even longstanding, can improve quickly and dramatically with interruption of the fistula. Treatment is therefore recommended in almost all such cases, and meaningful improvement is possible, even in patients with longstanding and sometimes severe symptoms.
Dural AV fistula represents a potentially reversible cause of neurological dysfunction. Imaging findings may be non-specific resulting in initial misdiagnosis; thus, a high index of suspicion for this pathological entity is important to allow for timely diagnosis and treatment. The diagnostic importance of catheter angiography is highlighted. Early treatment is associated with the best outcomes, but even patients with profound deficit may improve substantially, emphasizing the value of treatment despite advanced neurological deficit.
The authors report no conflicts of interest.
Patient permission was obtained, and IRB approval was granted for the current study.
All data are available upon further request.