AUCTORES
Globalize your Research
case report | DOI: https://doi.org/10.31579/2690-4861/569
Department of Cardiothoracic and Vascular Surgery, University Hospital Mainz, Germany.
*Corresponding Author: Martin Oberhoffer, MD Department of Cardiothoracic and Vascular Surgery University Hospital Mainz Langenbeckstr. 1 D-55131 Mainz.
Citation: Martin Oberhoffer, Ahmed Ghazy, Rayan Chaban, Hendrik Treede, (2024), Successful treatment of severe coronary artery disease using combined coronary artery bypass graft surgery and baroreceptor activation therapy – a case series, International Journal of Clinical Case Reports and Reviews, 25(4); DOI:10.31579/2690-4861/569
Copyright: © 2024, Martin Oberhoffer. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 04 October 2024 | Accepted: 20 November 2024 | Published: 24 April 2025
Keywords: coronary artery bypass graft surgery; baroreflex activation therapy; BAT
Introduction
Baroreflex activation therapy (BAT) is associated with sustained reductions in arterial pressure and good clinical outcomes through electrical stimulation of the carotid sinus, rendering it a proven therapeutic option for patients with arterial hypertension. However, there are several concerns with regard to the procedure particularly when applied as part of a one-stage procedure during conventional cardiac surgery. We herein report on two patients undergoing successful treatment of severe coronary artery disease using combined coronary artery bypass graft (CABG) surgery and BAT.
Case presentation
Despite vasopressor support and application of a general anesthesia cardiac surgery protocol, intraoperative test-activation of the BAT device already resulted in a clear response, which then further translated into substantial and sustained reductions in arterial pressures in the follow-up period. In line with that, administration of antihypertensive drugs could also be reduced sustainably. Bleeding complications were negligible. The combined approach was safe and technically feasible.
Discussion
The presented one-stage procedure therefore represents a promising option for patients with coronary artery disease and pre-existing therapy-refractory arterial hypertension requiring surgery to prevent further end-organ damage.
Baroreflex activation therapy (BAT) represents a proven therapeutic option for patients with arterial hypertension persisting despite a minimum of 8 weeks of oral antihypertensive medication of at least three different classes including a diuretic agent [1]. When BAT implantation is performed in combination with coronary artery bypass grafting (CABG) several concerns might arise including 1. Bleeding risk at the carotid artery access and the device pocket after CABG under cardiopulmonary bypass, 2. Safety issues due to manipulation of the carotid artery, 3. Responsiveness of the carotid sinus reflex under general anesthesia plus vasoactive substances, 4. Increased ICU and hospital stay due to prolonged operative time and 5. Postoperative efficacy of BAT. We herein report on two patients undergoing successful treatment of coronary artery disease and therapy-refractory arterial hypertension using combined CABG and BAT implantation. Informed consent for retrospective evaluation was obtained from both patients.
A 78-year-old male patient with severe coronary 2-vessel disease and therapy- refractory arterial hypertension was refered to our hospital for coronary artery bypass grafting (CABG). His medical history included dialysis dependent renal failure, hyperlipidemia and severe peripheral vascular disease with multiple interventions on his iliac, femoral and renal arteries. Due to his longstanding history of hypertension and episodes of hypertensive crisis despite maximum tolerated antihypertensive medications, surgical myocardial revascularisation and implantation of a BAT system (Barostim neo, CVRx, USA) as a one stage approach was scheduled. CABG was perfomed under cardiac arrest using the LIMA to the LAD and a saphenous vein to the RIVP. After sternal closure the BAT device was implanted via right cervical and subclavicular access. Total operative time was 300 minutes. The preoperative hemoglobin concentration was 8.2 g/dl (dialysis-dependant patient) requiring transfusion of red blood cells (2 units PRC) during cardiopulmonary bypass. Postoperatively the patient was extubated within 6 hours and transferred to the regular ward the next day without any neurologic event or bleeding complication or cervical hematoma. The results of BAT activation on blood pressure during implantation, postoperative activation and in the follow up period are depicted in Figure 1. Antihypertensive medication could be reduced during the 33-month follow-up period (Table 1).
| preoperative | 30 day follow-up (medication reduced) | 33 months follow-up (medication reduced) | |
| RR syst (mmHG) | 160 | 141 | 142 |
| RR diast (mmHg) | 88 | 73 | 79 |
| HR | 78 | 53 | 81 |
Figure 1: Course of heart rate and systolic and/or diastolic blood pressure levels before, during and after combined CABG and BAT implantation.

This case reports on a 72-year-old male, who presented to our hospital with coronary triple-vessel disease. He had undergone multiple percutaneous interventions and his pre-existing co-morbidities included therapy– refractory arterial hypertension under 4-fold antihypertensive medication (plus diuretic agent) and type II diabetes mellitus. Quadruple- CABG was done using both mammarian arteries (Y-graft) to LAD and sequentially to OM1 and OM2 and a saphenous vein to the RCA.
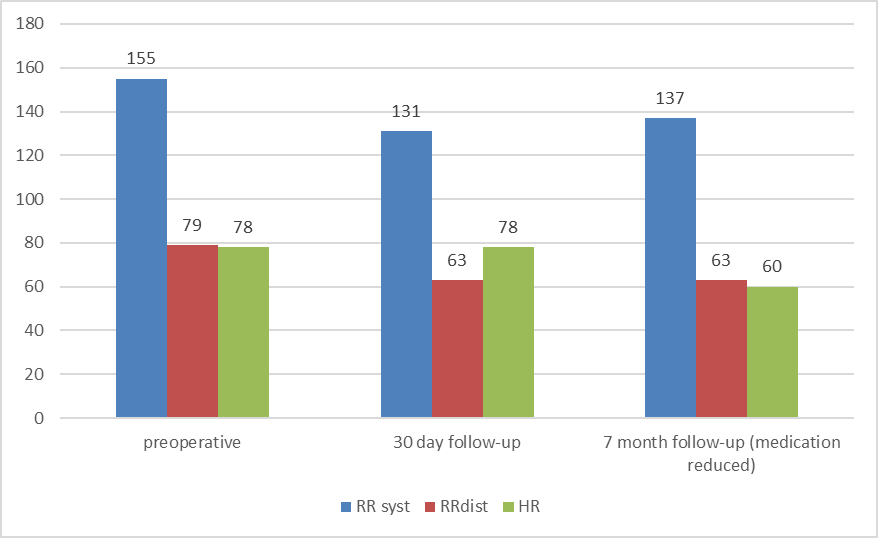
Implantation of the BAT device on the right carotid bulb followed immediately after sternal wound closure. Total operative time was 320 min. No blood transfusion was necessary (preoperative Hb 13.5 g/dl, postoperative Hb 9.8 g/dl). The patient was extubated the same day and transferred to our regular ward on the 1st postoperative day without any complications. The patient was discharged to a rehabilitation facility 12 days after hospital admission. Blood pressure recordings in the follow-up period showed sustained lower levels (Figure 2) while the requirement for antihypertensive medications could be reduced (Table 1).

Figure 2: Course of heart rate and systolic and/or diastolic blood pressure levels before, during and after combined CABG and BAT implantation
| preoperative | 30 day follow-up | 7month follow-up (medication reduced) | |
| RR syst (mmHg) | 155 | 131 | 137 |
| RR diast (mmHg) | 79 | 63 | 63 |
| HR | 78 | 78 | 60 |
Combined CABG and BAT in our patients was safe, feasible and efficient. Although prolonged operative time is associated with a higher incidence of postoperative complications [2, 3] our patients course was uneventful regrading neurologic, bleeding or wound healing complications. Intraoperative BAT activation showed a clear reactivity of the baroreceptor-reflex despite the use of a cardioanesthesia protocol and application of vasoactive substances. [4] Time on ventilation, ICU and hospital stay were comparable to conventional CABG patients. Postoperative BAT activation resulted in a substantial reduction of blood pressure values. During the follow-up period up to 33 months the blood pressure lowering effect sustained. Antihypertensive medication could be reduced in both patients. This one-stage approach represents a promising treatment option for selected patients with coronary artery disease and pre-existing therapy-refractory arterial hypertension.
Statement of Ethics
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The patient’s legal representative has given written informed consent to publish their case.
The authors have no conflicts of interest to declare.
The authors declare no funding relevant to the study.
MO analyzed and interpreted the data, participated in the manuscript preparation, discussed the data/revised the manuscript and provided significant intellectual input to the treatment of the reported patients and the manuscript. All authors have approved the final version of the manuscript. MO is the guarantor of this work.