AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2692-9759/146
Department of Cardiology, University Hospital Center IBN ROCHD, Casablanca, Morocco.
*Corresponding Author: Obeidat Saleh, Department of Cardiology, University Hospital Center IBN ROCHD, Casablanca, Morocco.
Citation: Obeidat Saleh, Boucetta A, Siyam H, Nouamou I, Haboub M, Habbal R, (2024), Reversible Sinoatrial Block in a Patient on Bradycardic Calcium Channel Blockers in the Context of Hyperkalemia and Acute Renal Failure, Cardiology Research and Reports, 6(7); DOI:10.31579/2692-9759/146
Copyright: © 2024, Obeidat Saleh. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 02 December 2024 | Accepted: 09 December 2024 | Published: 17 December 2024
Keywords: sinoatrial bloc; calcium channel blockers; hyperkalemia; rhythmology; case report
Introduction: Sinoatrial block (SAB) is a rare cardiac conduction abnormality that can occur in the context of electrolyte disturbances, acute renal failure (ARF), and medication side effects.
Case presentation: This report describes the case of a patient on verapamil with hyperkalemia due to acute renal failure (ARF), who developed a reversible sinoatrial block (SAB) after correction of the abnormalities and discontinuation of the medication.
Discussion: Hyperkalemia played a key role in exacerbating the bradycardia induced by verapamil, while acute renal failure contributed to the accumulation of the drug. Prompt management, including measures to lower potassium levels and adjust antihypertensive therapy, enabled complete recovery without the need for cardiac pacing.
Conclusion: This case highlights the importance of closely monitoring electrolytes and treatments in patients with renal failure or similar risk factors.
Sinoatrial block (SAB) is a disorder of the sinoatrial node, which regulates the heart's rhythm by generating electrical impulses that trigger heart contractions. While often linked to primary heart conditions, SAB can also be triggered by external factors, including medications such as calcium channel blockers (CCBs) [1]. These drugs, especially bradycardic forms like verapamil and diltiazem, are commonly used to treat hypertension and arrhythmias but can affect cardiac conduction, leading to SAB.
CCBs work by inhibiting calcium influx into cardiac cells, which slows sinoatrial node activity, potentially resulting in bradycardia or even cardiac arrest [2]. The risk is higher in patients with conditions like acute renal failure, which disrupts drug elimination and electrolyte balance, particularly potassium. Hyperkalemia, caused by impaired renal potassium excretion, can worsen cardiac arrhythmias, especially in combination with CCBs. This creates a dangerous cycle, where bradycardia and hyperkalemia together significantly impair cardiac function and can threaten the patient's life expectancy [3].
This clinical case explores the impact of CCBs on cardiac conduction in a patient with acute renal failure, highlighting how hyperkalemia can exacerbate the effects of these medications, leading to sinoatrial block. The presentation and management of this complex situation provide an opportunity to discuss the underlying pathophysiological mechanisms, current therapeutic strategies, and key lessons for the clinical management of such cases.
A 64-year-old male patient presents to the emergency department with a medical history notable for chronic hypertension, type 2 diabetes, and recently diagnosed acute renal failure (ARF). He has been on treatment for several years for his hypertension, including a bradycardic calcium channel blocker (verapamil), and was recently hospitalized for decompensation of his acute renal failure, secondary to severe dehydration and moderate sepsis.
Upon arrival at the emergency department, the patient complains of dizziness, mild chest pain, and a feeling of fatigue that began earlier in the morning. He has significant bradycardia, with a heart rate measured at 40 beats per minute. He is also disoriented, but without complete loss of consciousness. An electrocardiogram (ECG) performed at admission shows a sinoatrial block (SAB) with severe bradycardia.
His medical history includes hypertension diagnosed 5 years ago, effectively treated with verapamil and an angiotensin-converting enzyme (ACE) inhibitor, type 2 diabetes controlled with metformin and insulin, with well-regulated blood glucose levels, and recently diagnosed acute renal failure of multifactorial origin (dehydration due to prolonged diarrhea and moderate sepsis). The acute renal failure required intravenous fluid therapy and close monitoring of renal function. He had no history of structural heart disease but does have a tendency towards orthostatic hypotension.
The patient was conscious but agitated. His vital signs are as follows: heart rate: 40 bpm, blood pressure: 95/60 mm Hg, oxygen saturation: 98% on room air, temperature: 37.4°C (slight fever).
On physical examination, he is mildly dehydrated, with dry mucous membranes and low blood pressure, but without signs of overt shock. There are no signs of acute respiratory distress or peripheral edema. The patient does not have severe chest pain but complains of mild dizziness, especially when standing.
The admission ECG shows a third-degree sinoatrial block with absent P waves and a junctional escape rhythm (Figure 1).
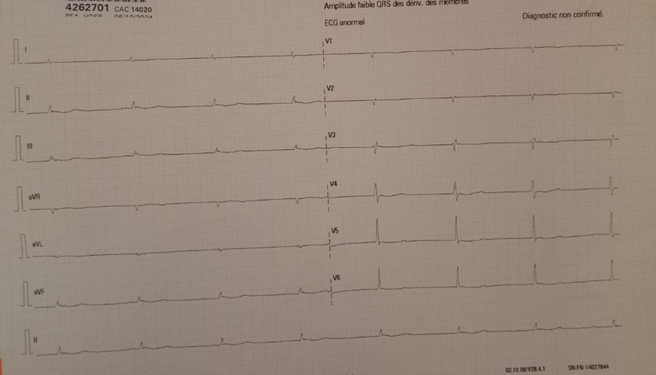
Figure 1: ECG shows a third-degree sinoatrial block
The blood tests reveal serum potassium: 6 mmol/L (hyperkalemia), serum creatinine: 218 µmol/l (indicating acute renal failure), blood urea nitrogen: 42 mg/dL.
The presence of severe hyperkalemia is particularly concerning, as it may further compromise cardiac conduction, especially in combination with the bradycardic effects of verapamil.
The patient is admitted to the intensive care unit due to the severity of his clinical presentation, particularly the severe bradycardia and hyperkalemia, which require close monitoring and prompt intervention. The main objective is to stabilize the patient, prevent potential cardiac complications, and promptly adjust the management of the associated acute renal failure (ARF).
The patient is placed under continuous monitoring with cardiac surveillance to track the progression of bradycardia and other conduction abnormalities. An electrocardiogram (ECG) is performed every hour to detect any changes in heart rhythm, such as the development of additional blocks or ventricular arrhythmias.
Due to the initial low heart rate and sinoatrial block, a temporary external pacemaker is inserted to ensure an adequate heart rate and reduce the risk of syncope or severe complications.
Hyperkalemia is corrected by the administration of intravenous sodium bicarbonate, calcium gluconate, and potassium exchange resin (Kayexalate) to lower the serum potassium levels.
Verapamil is immediately discontinued, and an assessment is made regarding the indication for alternative treatments for hypertension. A cautious diuretic treatment is administered to help eliminate excess potassium while avoiding further renal overload.
The patient's acute renal failure requires close monitoring of renal function. The patient also receives intravenous rehydration with saline fluids to maintain adequate urine output and promote the elimination of toxins. Renal parameters (creatinine, urea, urine output) are monitored every 6 hours.
Over the first 24 hours, the patient shows signs of gradual improvement. His heart rate increases progressively, reaching 50 to 55 bpm, although the sinoatrial block persists. The external pacemaker continues to maintain the heart rate at an optimal level.
The patient remains hemodynamically stable, with a mean blood pressure of 95/60 mmHg. His dizziness gradually subsides, and he becomes more alert. However, he still complains of general malaise and muscle weakness, likely due to the hyperkalemia and the effects of the treatments administered.
Continuous monitoring shows a slight reduction in the intensity of the sinoatrial block, but moderate bradycardia persists due to the residual effect of verapamil and hyperkalemia.
After 24 hours, the serum potassium is measured at 5.0 mmol/L, which remains elevated but more controlled. After 48 hours, it reaches 4.2 mmol/L, within normal limits. The creatinine level remains elevated during the first few days but shows a downward trend, reaching 166 µmol/l at 48 hours. Urine output is stable, although still relatively low. Dialysis is not required during the first 48 hours, as the patient's renal function shows signs of recovery.
Over the course of 72 hours, the patient's potassium levels normalized with medical intervention. The bradycardia resolved, and the patient’s heart rate increased to normal levels without requiring pacing. After stabilization, renal function showed gradual improvement, and the patient was eventually discharged with a referral to nephrology for long-term management of his kidney disease.
The resolution of the sinoatrial block after 72 hours reinforces the idea that the primary cause was hyperkalemia and the effect of verapamil. It is unlikely that further episodes of sinoatrial block will occur if renal function continues to improve.
The sinoatrial node (SA node), as the heart's primary pacemaker, relies on precise ionic exchanges, particularly involving calcium and potassium, for generating and conducting impulses [4].
Sinoatrial block (SAB) is a rare but clinically significant condition affecting cardiac conduction. It occurs when impulses generated by the sinoatrial (SA) node fail to propagate effectively to the atrial myocardium. SAB is classified into three degrees based on the severity of conduction delay or failure [1].
In this case, the pathophysiology of SAB is multifactorial, involving drug toxicity from calcium channel blockers (CCBs), hyperkalemia, and the underlying acute renal failure (ARF).
CCBs, particularly non-dihydropyridines such as verapamil and diltiazem, exert their therapeutic effects by inhibiting L-type calcium channels. These channels are integral to the depolarization process in SA nodal cells, where calcium influx generates the action potential responsible for initiating heartbeats [5]. By decreasing calcium influx, CCBs reduce automaticity and slow conduction within the SA node.
While beneficial for conditions like hypertension and atrial tachyarrhythmias, the bradycardic effects of CCBs can be pronounced in patients with baseline conduction system vulnerabilities, such as fibrosis or ischemia. Moreover, the risk of SAB is amplified in scenarios where drug clearance is impaired, as in this case of ARF.
Simultaneously, hyperkalemia amplifies the conduction impairment by altering the resting membrane potential of cardiac cells. Elevated serum potassium reduces the electrochemical gradient, causing partial depolarization and impaired impulse generation [6]. The synergistic interaction of CCBs and hyperkalemia increases the risk of sinoatrial block, particularly in the setting of ARF, where drug clearance is reduced, and electrolyte disturbances are more profound.
Hyperkalemia, a hallmark of ARF, has a well-recognized role in conduction abnormalities, including sinoatrial block. Potassium is critical for maintaining the resting membrane potential of cardiac cells. Elevated serum potassium levels diminish the excitability of the myocardium by reducing the difference between the resting and threshold potentials. This leads to impaired propagation of impulses through the SA node, slower initiation of impulses due to partial depolarization of pacemaker cells and prolonged repolarization phases and conduction delays [7].
In this case, the patient’s hyperkalemia was sufficient to exacerbate the bradycardic effects of verapamil, contributing to the observed sinoatrial block.
Patients with sinoatrial block secondary to verapamil treatment and hyperkalemia may experience severe symptoms due to the resulting severe bradycardia. These symptoms include dizziness, syncope, signs of heart failure, and even cardiac arrest in severe cases.
A third-degree sinoatrial block looks very similar to a sinus arrest. However, a sinus arrest is caused by a failure to form impulses. A third-degree block is caused by failure to conduct them. The rhythm is irregular and either normal or slow. It is followed by a long pause that is not a multiple of the P-R interval. The pause ends with a P wave, instead of a junctional escape beat the way a sinus arrest would [8].
Management of SAB in this context necessitates a multifaceted approach, immediate stabilization of hyperkalemia, Intravenous calcium gluconate, insulin with dextrose, and sodium bicarbonate were effectively used to stabilize the cardiac membrane and lower serum potassium. In severe cases, emergent dialysis may be necessary to rapidly correct hyperkalemia [9].
discontinuation of the offending agent, withholding verapamil eliminated a key contributing factor to the bradycardia, allowing for spontaneous recovery of sinoatrial node function. temporary pacing may be indicated in cases of persistent bradycardia or hemodynamic instability [10].
Addressing the underlying ARF and optimizing antihypertensive therapy to avoid recurrence were critical for preventing future episodes.
The prognosis of SAB depends on timely identification and correction of reversible factors. In this patient, normalization of potassium levels and discontinuation of verapamil led to full recovery without the need for permanent pacing. However, this case highlights the need for close monitoring of renal function and electrolyte levels in patients on CCBs, particularly in the presence of predisposing factors like ARF [11,12].
This case underscores several important clinical principles. Regular evaluation of drug regimens is crucial in patients with impaired renal function to prevent toxicity. Vigilant monitoring and prompt correction of hyperkalemia are essential to avoid life-threatening arrhythmias. Adjusting pharmacological strategies based on the patient’s renal and metabolic status can prevent adverse outcomes.
Further research is needed to explore the dose-dependent effects of calcium channel blockers (CCBs) in patients with renal insufficiency, the role of new potassium-lowering therapies in managing hyperkalemia-related arrhythmias, and strategies to identify high-risk patients prone to developing sinoatrial block (SAB) in the context of polypharmacy.
This case highlights the importance of promptly identifying reversible causes of sinoatrial block, particularly hyperkalemia and drug toxicity. Discontinuing verapamil and rapidly correcting electrolyte abnormalities led to complete resolution without the need for permanent cardiac pacing. It also emphasizes the need to adjust treatments according to renal function to avoid complications. Finally, close monitoring of electrolytes and medications is essential to prevent arrhythmias in high-risk patients.