AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2768-2757/110
North Manchester General Hospital, Department of Urology, Delaunays Road, Manchester, M8 5RB, United Kingdom.
*Corresponding Author: Anthony Kodzo-Grey Venyo, North Manchester General Hospital, Department of Urology, Delaunays Road, Manchester, M8 5RB, United Kingdom.
Citation: Grey Venyo AK, (2024), P63 Expressing Adenocarcinoma of The Prostate Gland, A Rare Neoplasm Which Tends to Pose Diagnostic Dilemma Sometimes: Review and Update, Journal of Clinical Surgery and Research, 5(4); DOI:10.31579/2768-2757/110
Copyright: © 2024, Anthony Kodzo-Grey Venyo. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 05 April 2024 | Accepted: 25 April 2024 | Published: 01 May 2024
Keywords: p63 expressing prostate cancer; prostate biopsy; histopathology examination; immunohistochemistry staining; ultrasound scan; computed tomography scan; magnetic resonance imaging scan; diagnostic dilemma; biological behaviour; further studies
It has been documented that prostate cancer is the world's leading cause of cancer and also the second commonest cancer in men which does tend to pose challenges in its diagnosis. It has been iterated that immunohistochemistry studies utilising tumour markers like high molecular weight cytokeratin, p63 aid in the diagnosis of prostate cancer. It has been known for some time that the absence of immunohistochemistry staining of prostate lesion for p63 and high molecular weight cytokeratin and presence of p504s in the biopsies indicate malignant lesions. Nevertheless, it had also been pointed out as well as documented that some rare cases of adenocarcinoma of prostate variants do demonstrate evidence of the tumour cells exhibiting p63 immunohistochemistry staining and this does pose a diagnostic dilemma that may make the unfamiliar pathologist mis-diagnose such a malignant tumour as a benign prostate lesion. p63-positive adenocarcinoma of the prostate gland is a major diagnostic pitfall. There is a danger of interpreting malignant glands as benign and arriving at a false-negative diagnosis. This can be prevented by the understanding of the pattern of immunohistochemistry staining expression related to this variant of prostate cancer. The major points that favour the diagnosis of carcinoma in these cases include: non-basal p63 staining and negative HWMCK and positive p504s staining. The biological behaviour of this particular rare variant of prostatic carcinoma is not certain and requires to be studied further into more detail. Considering the rarity of p63 expressing prostate cancers and the fact that most clinicians including pathologists, urologists, and oncologists would not have encountered a case of p63 expressing prostate cancer before in order to update all clinicians regarding this rare tumour, the ensuing article has been extensively written and divided into two parts: (A) Overview which has discussed general overview aspects of p63 expressing neoplasms and (B) Miscellaneous Narrations and Discussions from Some Case Reports, Case Series, and Studies Related to Primary p63 Expressing Adenocarcinomas of the Prostate Gland. A high-index of suspicion as well as knowledge of the histopathology examination features as well as immunohistochemistry examination features of this rare tumour is required from all clinicians. Knowledge of the treatment options, biological behaviour as well as outcome following treatment of the tumour has been extensively discussed as updating information. The update has clearly pointed out that further studies are required to determine the role of p63 overexpression in prognostication.
It has been iterated that with regard to men, carcinoma of the prostate gland represents the second most common cancer, after lung cancer. [1] It had also been documented that carcinoma of the prostate gland is also the world's leading cause of cancer [1] as well as that carcinoma of prostate gland is associated with advanced age, genetics factor smokers, obese individuals, and due to endogenous factors. [2] Prostate-specific antigen (PSA) levels are essential in elderly patients to identify the risk of prostate cancer. Though it is not very specific, high levels are concomitant with prostate cancer. Diagnosis of prostate cancer purely on the foundation of the clinical and morphological features is difficult. Here comes the role of the tumour markers and immunohistochemical markers. [3] Immunohistochemical markers such as p63, high molecular weight cytokeratin (HMWCK), and p504s aid in the appropriate diagnosis of prostatic cancers.
p63, an analogue of p53, is a tumour suppressor gene which encodes for isotypes which either act as p53-dominant negatives or transactivate p53 reporter genes, whose presence aids apoptosis and reduces the progression of cancer. [4] It comprises 15 exons and codes for 6 different mRNA isoforms which have a common DNA-binding domain. [3] [5] p63 is required for nourishing a basal-cell population, maintaining a prostate epithelial stem cell population, and is also essential for prostate development. [4] Markers like p53 and p63 are expressed on the nuclei of the normal basal cells. Usually, adenocarcinomas are devoid of basal cells, whereas benign lesions are encircled by the same. Hence, prostate adenocarcinoma can be differentiated from benign prostate lesions and hyperplasia by the absence of p63 staining in the basal cells in prostate carcinoma. Hence, p63 and HMWCK, and basal-cell immunohistochemistry markers turn out to be beneficial to distinguish benign and malignant conditions. [6] [7] Yet, there are few adenocarcinomas which retain the basal cells and have partial p63 and HMWCK staining, and there are a small number of Benign prostatic hyperplasia (BPH) and adenocarcinoma mimickers which don't express the basal-cell makers. [7]. Considering that p63 expressing adenocarcinomas of the prostate gland are rare, it would be envisaged that majority of clinicians working globally including Urologists, Oncologists, and pathologists may so far not have encountered this type of kidney neoplasm before. In view of this the ensuing article on primary p63 expressing carcinoma of the prostate gland has been written in two parts: (A) Overview which has discussed general overview aspects of p63 expressing neoplasms and (B) Miscellaneous Narrations and Discussions from Some Case Reports, Case Series, and Studies Related to Primary p63 Expressing Adenocarcinomas of the Prostate Gland.
To review and update the literature on primary p53 expressing carcinomas of the kidney.
Internet data bases were searched including: Google; Google Scholar; Yahoo; and PUBMED. The search words that were used included: p63 expressing adenocarcinoma of prostate; p63 expressing prostatic cancer; p63 expressing primary malignant neoplasm of prostate gland; and p63 expressing primary prostatic malignant neoplasm. Forty-four (44) references were identified which were used to write the article which has been divided into two parts: (A) Overview which has discussed general overview aspects of p63 expressing neoplasms and (B) Miscellaneous Narrations and Discussions from Some Case Reports, Case Series, and Studies Related to Primary p63 Expressing Adenocarcinomas of the Prostate Gland.
A] Overview [8]
Definition / general statement [8]
Essential features [8]
The essential features of p63 expressing prostate cancer tumours had been summated as follows: [8] [9] [10]
Epidemiology
Laboratory tests [8]
Prognostic factors
The factors of prognostication, had been summated as follows: [8]
Microscopic (histologic) description
The microscopy histopathology examination features of p63 expressing prostate cancer had been summated as follows: [8]
Immunohistochemistry staining
The immunohistochemistry staining features of p63 expressing prostate cancers had been summated as follows: [8]
Positive stains
Negative stains
The negative immunohistochemistry staining features of p63 expressing prostate cancers had been summated as follows: [8]
Molecular / cytogenetics description
The molecular and cytogenetics study features of p63 expressing carcinoma of the prostate gland had been summated as follows: [8]
Differential diagnoses
The differential diagnoses of p63 expressing prostate cancer had been summated as including the ensuing: [8]
[B] Miscellaneous and Discussions from Some Case Reports, Case Series, And Studies Related to P63 Immunonogistochemistry Expressing Carcinoma of The Prostate Gland
Osunkoya et al. [9] stated that aberrant diffuse immunohistochemistry expression of p63 in prostate carcinoma cells is a rare and poorly understood phenomenon.
Osunkoya et al. [9] studied 19 cases of prostate cancer with aberrant diffuse expression of p63 which were diagnosed based upon pathology examination of specimens of prostate needle biopsy and they reviewed the subsequent radical prostatectomies in 6 cases. They reported on 19 out of 21 cases, and they reported that 100perecentage of the cancer nuclei had stained intensely for p63, with 70perecentage staining in the remaining 2 cases. Two additional radical prostatectomies with aberrant p63 staining with no needle biopsies available for review were also analysed by
Osunkoya et al. [9]. On the hematoxylin and eosin-stained slides, 19 out of 21 cases that amounted to 90.5% of the cases had demonstrated a distinctive morphology composed predominantly of glands, nests, and cords with atrophic cytoplasm, hyperchromatic nuclei, and visible nucleoli. Osunkoya et al. [9] also reported the following results:
Giannico et al. [10] stated that prostatic adenocarcinoma with aberrant diffuse expression of p63 (p63-PCa) had been a recently described variant of adenocarcinoma of prostate gland. Giannico et al. [10] undertook a study to investigate the clinical and pathological features of p63-PCa at radical prostatectomy (RP). Giannico et al. [10] reviewed 21 cases of p63-PCa diagnosed based upon needle biopsy at subsequent RP. Giannico et al. [10] undertook immunohistochemical analysis for PIN4 and Ki-67 in all RP cases. Giannico et al. [10] reported the following results:
Giannico et al. [10] summated that they had recommended that these tumours should not be assigned a Gleason score and their favourable findings at RP should be noted.
Baydar et al. [11] iterated that prostate carcinomas exhibiting aberrant diffuse-nuclear p63 expression were extremely rare, and there was only 1 article in the literature reporting a series of 21 such cases by the time of publication of their article in 2011. Baydar et al. [11] iterated that they had documented an additional case of p63-positive prostatic adenocarcinoma in a 60-year-old man, whose diagnosis was difficult. They reported that the patient was found to have an elevated serum prostate-specific antigen (PSA) level at a general health check-up and he was then referred to the hospital. His serum PSA was 4.2 ng/mL. He underwent digital rectal examination and transrectal ultrasound scan which did not demonstrate a lesion. He underwent trans-rectal needle biopsy of the prostate gland and pathology examination of the biopsy specimens identified atypical, small prostatic glands which were suspected for adenocarcinoma at 2 cores. Nevertheless, immunohistochemistry staining studies of the biopsy specimens had demonstrated nuclear p63 expression within the suspicious glands. Repeat biopsy of the prostate lesion upon pathology examination had demonstrated only high-grade prostatic intraepithelial neoplasia. In the third transrectal biopsy, finding of the same atypical glands demonstrating perineural invasion had facilitated the diagnosis of malignancy. The patient underwent a radical prostatectomy. Five different small tumour foci were identified within the prostate after pathological evaluation, one of which was p63 positive staining and the others p63 negative staining. The largest of the classic p63-negative tumours had shown a TMPRSS2-ERG translocation by fluorescent in situ hybridization while the p63-positive tumour did not. Baydar et al. [11] had iterated that this subtype (p63-positive prostate adenocarcinoma) should be listed among the recognized rare variants of adenocarcinoma of the prostate gland.
Khalid et al. [12] stated the following:
Khalid et al. [12] reported a 76-year-old Chinese man, who had attended the clinic with a manifestation of swelling over his right buccal mucosa with on and off pain and numbness at his right chin in December 2017. His symptoms had commenced two months preceding his attendance at the clinic. It was found upon his examination that clinically his buccal mucosa was smooth, and a well-defined firm mass could be palpated over his normal overlying buccal mucosa (see Figure 1). He was completely edentulous with no restriction of his mouth opening.

Figure 1: Intraoral photograph showing smooth, well-defined, firm mass over the right buccal mucosa with normal overlying mucosa. Reproduced from: [12] Under the Creative Commons Attribution License.
The patient was documented to be a known case of end-stage prostate cancer. He was initially diagnosed with adenocarcinoma of the prostate gland in June 2014 via pathology examination of specimens of his trans-urethral resection of his prostate (TURP) gland. The Gleason score of his prostate cancer was 4+5 = 9, and his serum prostate-specific antigen (PSA) was high (65 ng/mL). he had an isotope bone scan in July 2014 which had demonstrated multiple bone metastases involving his left 4th rib, 4th lumbar spine, sacrum, and left pubic bone but which had not involved his mandible. He was treated with androgen deprivation therapy (Lucrin) until December 2015, and his treatment was followed by seven months of antineoplastic agents (Abiraterone acetate) from December 2016 to July 2017 due to his persistent high baseline of serum PSA value >100 ng/mL. His prostate cancer disease had progressed and the patient was treated with non-steroidal antiandrogen (Enzalutamide) from July 2017. His serum PSA value did not respond to the treatment he had. By October 2017, his serum PSA level was 120 ng/mL, which had coincided with his first clinical symptom of numb chin syndrome. He underwent a cone-beam computed tomography (CBCT) scan which had demonstrated erosion of bone within the anterior part of his ascending ramus and retromolar region (see Figure 2). An incisional biopsy of the lesion was then undertaken for pathology examination.

Figure 2: CBCT image showing erosion of bone at the anterior part of right ramus of mandible and retromolar region. Reproduced from: [12] Under the Creative Commons Attribution License.
Pathology examination of the haematoxylin and eosin (H&E) slides of his biopsied lesion demonstrated tumour islands that consisted of central cells with hypo-chromatic and vacuolated nuclei, pale eosinophilic cytoplasm, and this had exhibited pleomorphism. The peripheral basal tumour cells were found upon pathology examination to be spindle-shaped and appeared hyperchromatic (see Figure 3), with areas of extensive comedonecrosis visualised. The central tumour cells had exhibited immunohistochemistry staining positivity for PSA (see Figure 4A) and cytokeratin (CK; weak). The peripheral basal tumour cells were noted to have exhibited immunohistochemistry staining positivity for PSA, CK (weak), and p63 (scattered) (see Figure 4B). Both the central tumour cells and the basal tumour cells had exhibited negative staining for CK7 and CK20. Considering the H&E and immunohistochemistry manifestation of the case, a diagnosis of adenocarcinoma metastasis from the prostate was reported.

Figure 3: Photomicrograph shows a tumour island consisting of central round cells and peripheral spindle (magnification x100, stain A&E). Reproduced from: [12] Under the Creative Commons Attribution License.

Figure 4: Photomicrographs showing (A) immunopositive cytoplasmic staining of tumour cells with PSA (magnification x100) and (B) scattered immunopositive staining of tumour cells with p63 (magnification x100). Reproduced from: [12] Under the Creative Commons Attribution License.
The attending oncologist was informed of the metastatic finding. Following this, the patient underwent a computed tomography (CT) scan and isotope bone scan (see Figure 5A and 5B) which demonstrated
multiple bone metastases to his sternum, ribs, ilium, femur, and vertebrae as well as his mandible. Subsequently, patient received chemotherapy treatment. Nevertheless, three months later, unfortunately, the patient died as a sequel of hi tumour.

Figure 5: Bone scan images (A) anteroposterior view and (B) posteroanterior view showing multiple distant bone metastases to the mandible, sternum, ribs, ilium, femur and vertebrae. Reproduced from: [12] under the Creative Commons Attribution License.
Khalid et al. [12] made the ensuing educative summative iterations:
Khalid et al. [12] made the ensuing conclusions:
Ferronika et al. [13] stated the following:
Ferronika et al. [13] reported that they had utilised a cross-sectional study during two years between 2009 and 2010, and they had investigated a total of 79 paraffin embedded tissues of benign prostatic hyperplasia, PIN prostatic intraepithelial neoplasia, low and high Gleason score prostate cancer by means of immunohistochemistry staining studies. Ferronika et al. [13] also analysed the associations between cytoplasmic p63 and ALDH1A1, as well as with pathological diagnosis, by undertaking Chi-Square test using SPSS 15.0. Links of both markers with cell proliferation rate (KI-67) and apoptotic rate (cleaved caspase 3) were also analyzed by Kruskal-Wallis test. Ferronika et al. [13] summated their results as follows:
Dhillon et al. [14] stated the following:
Fonseca-Alves et al. [38] reported that in their study, p63 immunohistochemistry staining expression was investigated in 90 canine PCs and 20 normal prostate tissues (NT). Fonseca-Alves et al. [38] also reported that the p63 expression pattern in luminal or basal cells was confirmed in a selected group of 26 PCs and 20 NT by immunohistochemistry and/or Western blotting assays. They had compared eleven canine PC samples aberrantly expressing p63 (p63+) in secretory cells with 15 p63 negative (p63-) cases in the context of several molecular markers (high molecular weight cytokeratin-HMWC, CK8/18, CK5, AR, PSA, chromogranin, NKX3.1, PTEN, AKT and C-MYC). Fonseca-Alves et al. [38] summarised their results as follows:
Fonseca-Alves et al. [38] made the ensuing conclusions:
Wu et al. [6] reported a case of adenocarcinoma of prostate gland that showed diffuse aberrant p63 expression within the secretory cells and they reviewed the literature and differential diagnosis. Wu et al. [6] made the ensuing iterations:
Tan et al. [5] described a rare group of prostate adenocarcinomas that had exhibited an aberrant expression of p63, a protein strongly which is expressed in prostatic basal cells and absent from usual-type acinar prostate cancers. Tan et al. [5] stated the following:
Tan et al. [5] made the following conclusions:
Torres et al. [39] stated the following:
Torres et al. [39] compared a total of 8 p63-expressing prostate carcinomas at radical prostatectomy to 358 usual-type adenocarcinomas by gene expression profiling performed on formalin fixed paraffin embedded tumour tissue using Affymetrix 1.0 ST microarrays. Correlation between differentially expressed genes and TP63 expression was performed in 5239 prostate adenocarcinomas available in the Decipher GRID. For validation, ETS2 in situ hybridization was undertaken on 19 p63-expressing prostate carcinomas and 30 usual-type adenocarcinomas arrayed on tissue microarrays (TMA). Torres et al. [39] summarised the results as follows:
Lokesha et al. [1] iterated the following:
Lokesha et al. [1] reported an 87-year-old, diabetic, as well as a known hypertensive gentleman who had manifested with incomplete voiding, increased urinary urgency, and frequency of micturition, together with bilateral pitting type of oedema which was confined to his feet and dull and deep generalized pain within his lower abdomen which appeared following his voiding of urine. The result of his serum PSA level had significantly increased to 213.3 ng/ml. Upon digital rectal examination, a Grade 3 prostate enlargement and hard prostate were felt. He underwent trans-rectal prostate biopsies which were obtained for histopathology examination. Pathology examination of his prostate biopsy tissue cores demonstrated a tumour which had comprised of back-to-back arranged small glands without basal-cell layer. The epithelial lining had demonstrated enlarged hyperchromatic nuclei with prominent nucleoli (see figure 6 and 6 b).
Figure 6: (a and b) Hematoxylin and eosin staining of the prostatic tissue exhibiting tumour composed of back-to-back arranged small glands without basal cell layer and epithelial lining showing enlarged hyperchromatic nuclei with nucleoli [200 × magnification] Reproduced from [1] under the Creative Commons Attribution License.
Immunohistochemistry staining study analysis was undertaken to evaluate the biopsy for the presence of basal cells with HMWCK and p63. A positive tumour marker p504s was also undertaken.
To the surprise of the authors, the nuclei of the tumour cells had exhibited positivity with p63 causing confusion [see figures 7 a and b]. The HMWCK study demonstrated negative staining within the cancerous glands [see figure 8] and p504s was diffusely and strongly positive [see figures 9 a and b].

Figure 7: (a and b) Photograph of the prostatic tissue [1b showing a magnified image] where nuclei of the tumour cells demonstrate p63 positivity [immunohistochemistry, 100 × magnification].

Figure 8: Glands of the tumour cells demonstrating negativity for high molecular weight cytokeratin [100 × magnification].
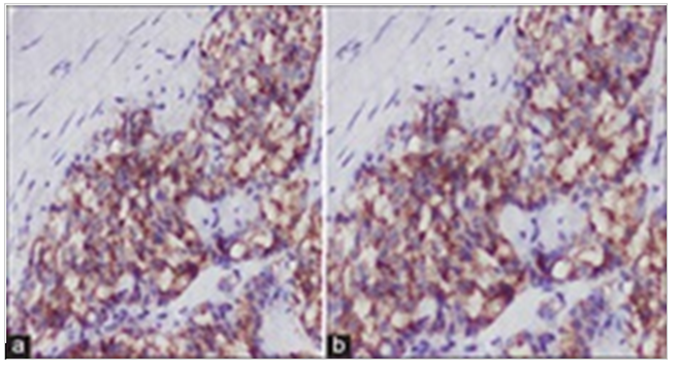
Figure 9: (a and b) Glands of the tumour cells [4b showing a magnified image] showing diffuse positivity for p504s molecular marker [100 × magnification].
Lokesha et al. [1] stated that upon review of literature, it was evident that a rare variant of adenocarcinoma of the prostate gland called p63-positive prostatic carcinoma could exhibit p63 overexpression within the nuclei of the malignant glands. They also found out upon review of the literature that this tumour entity could be distinguished from benign glands by the
fact that the expression of p63 is not basal in nature and the glands had exhibited negative reaction with HMWCK. A positive p504s staining also supports the malignant diagnosis. Lokesha et al. [1] iterated that in concordance with the immunohistochemical and histopathological findings, the case was confirmed to be a diagnosed case of p63-positive adenocarcinoma of prostate gland. The patient was managed mainly by means of chemotherapy, injection pamorelin (11.25 mg, intramuscular), tablet finast, tablet silodac, and tablet tabi for a month. Currently, the patient at the time of publication of his case had been undergoing regular follow-up assessments and he was asymptomatic.
Lokesha et al. [1] made the ensuing educative discussions:
Lokesha et al. [1] made the ensuing conclusions:
- Nil
Acknowledgements to:
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.

Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!

"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.

Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.

Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.

Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.
