AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2578-8965/259
Health Sciences University Istanbul Physical Therapy and Rehabilitation Training and Research Hospital, Bahçelievler/ Istanbul, Turkey.
*Corresponding Author: Bilge Aslan, Health Sciences University Istanbul Physical Therapy and Rehabilitation Training and Research Hospital, Bahçelievler/ Istanbul, Turkey.
Citation: Bilge Aslan, (2025), Our Experience Anesthetic and Surgical Approach of Debulking Procedures in Ovarian Cancer, J. Obstetrics Gynecology and Reproductive Sciences, 9(2) DOI:10.31579/2578-8965/259
Copyright: © 2025, Bilge Aslan. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 31 January 2025 | Accepted: 05 February 2025 | Published: 13 February 2025
Keywords: anesthesia; complications; ovarian ca; mortality; debulking operation
Objective: We aimed to determine the rescue approach of anesthesiologists and discussed operations of debulking procedures in Ovarian Cancer (CA) and survey, in this study.
Background: Most patients with ovarian cancer usually relapse during the first 5 years. Overall life expectancy is less than 50 % for 5 years, depending on the stage of the disease. Therefore, we follow the patients with an interval of 3-4 months for 5 years after the end of the operative treatment. Recurrent ovarian cancer diseases have the chance to be treated with surgery and different chemotherapy protocols.
Materiel and Methods: This clinical study aimed to evaluate the approaches to cytoreductive surgery in our reference center. We only included studies that defined optimal cytoreduction as surgery leading to residual tumors with a maximum diameter of any threshold up to 2 cm. Patients of 2008 - 2018 operated from cytoreductive over carcinoma were retrospectively evaluated. This study includes perioperative clinical management, preoperative approach, fluid and blood management, prevention, and treatment of major complications in women of 2187 seconder operated ovarian CA.
Results: Postoperative hyponatremia and anemia were detected. The fact that Ca 125 does not return to the target value after surgery supports the idea that surgery alone is insufficient in ovarian cancers. However, when the tumor burden decreases, the value of Ca 125 in the blood also decreases.
Conclusion: In our study, we showed with statistical analysis the importance of monitoring the debulking operations in preoperative, intraoperative and postoperative periods and the effect of the procedures on the mortality.
Anesthesiologists play an important role in the selection of patients for gynecological cytoreductive surgery, as well as in long-term surgical procedures, with significant loss of fluid or blood, or both, in the delivery of safe anesthesia and postoperative care in these long surgical procedures. Guidelines for these procedures have been provided professionally for clinical anesthesia with numerous sections [1].
Epithelial ovarian cancer (EOC) is the sixth most common cancer in women and the second most common malignancy of the female genital tract after endometrial cancer. In the United States, the EOC is diagnosed in approximately 22.000 women each year, with 15.000 women dying of illness. It is estimated that more than 200.000 women worldwide develop ovarian cancer each year and approximately 100.000 die from the disease. A woman who develops an EOC has a lifetime risk of one in 70. EOC can be seen in women younger than 15 years, but the average age is 56 [2,3]. Primary gynecologic cytoreductive surgery remains the standard and preferred approach for women with advanced ovarian CA and peritoneal cancer and is performed by experienced gynecological oncologists in a fully equipped hospital. Every effort should be made to completely resolve all visible peritoneal and retroperitoneal diseases as much as possible. This requires cooperation with more experienced surgeons, especially for intensive upper abdomen and perihepatic diseases. Gynecological oncologists should continue to advance their expertise and training in radical abdominal and retroperitoneal surgery, and adapt the surgical techniques and approaches routinely used by other surgical oncologists to obtain the best approach and skills necessary for gynecological cytoreductive surgical malignant lesions of the ovaries. It includes primary lesions arising from normal structures within the ovary and secondary lesions in cancers occurring anywhere in the body. Primary lesions include epithelial ovarian carcinoma (70% of all ovarian malignancies), germ cell tumors, sex cord-stromal tumors, and other rare types. Ovarian metastases are relatively common, with the most common being the endometrium, breast, colon, stomach, and cervix. The origin of ovarian carcinomas is controversial [4-7]. The risk of ovarian cancer is associated with a common variant of the mismatch repair gene, the promoter sequence of MLH1. In our study, the 5-year survival rate was 30% in patients undergoing cytoreductive and debulking operations. We aimed to evaluate the anesthetic and surgical management, in this study.
After the approval of the Ankara City Hospital Gynecology Local Ethics Committee (17.08.19, Decision no: 2), patients who underwent debulking operation due to ovarian CA between 01.01.2008 and 30.12.2018 were retrospectively evaluated. Demographic data of the patients and type of surgery, duration of surgery, perioperative hemodynamic data, ephedrine, vasopressor, crystalloid, or colloid consumption were collected (Table 1). Besides, perioperative Erythrocyte Suspension usage (ES), fresh frozen plasma (TDP) need, platelet suspension (PS) consumption, preoperative and postoperative hemoglobin (Hb), platelet counts, Alanine Transaminase (ALT) and Aspartate Aminotransferase (AST), Creatine (Cr), Ca 125 and Ca 19-9 values were recorded. Percentages of central venous catheters and intraarterial monitorization were evaluated. Different treatment methods were used for intraoperative bleeding. The duration of hospitalization was evaluated. In our study, we also examined intraoperative, postoperative treatment methods and results.
The data were entered in the EXCEL file and transferred to IBM SPSS.23 program and evaluated by statistical analysis. Before the statistical analysis, checks were made on the absence of data entry errors and whether the parameters were within the expected range. Normality assumptions of continuous variables were examined by skewness and kurtosis (Skewness and Kurtosis) coefficients and Kolmogorov Smirnov test, and whether excessive and outlier values were calculated by calculating z values and using the boxplot method. Wilcoxon signed ranks test (Wilcoxon signed-ranks test) was used to determine whether there was a significant difference between some laboratory parameters before and after surgery, and p <0>
| Age (years) | 50 ± 12 (30-80) |
| Height (cm) | 160 ± 8 (150-170) |
| Weight (kg) | 80 ± 15 (50-100) |
| Operation time(minute) | 240 ± 30 (64-280) |
| Time of anesthesia (min.) | 190 ± 20 (74-300) |
| 〖Pressure〗_systolic (mmHg) | 125 (±12) (60-120) |
| 〖Pressure〗_diastolic (mmHg) | 60 (±15) (40-80) |
Heart  (beats/min) (beats/min) | 110 (±12) (70-160) |
Heart  (beats/min) (beats/min) | 80 (± 16) (45-125) |
| Patients developing hypotension (n,%) | 1530.9 (70%) |
| Patients used ephedrine (n,%) | 656.1 (30%) |
| Ephedrine (mg) | 250.2 (±10) (0-40) |
| Patients used erythrocyte suspension (n,%) | 874.8 (40%) |
| Erythrocyte suspension (U) | 4 (±2) |
| Patients used fresh frozen plasma (n,%) | 656.1 (30%) |
| Fresh frozen plasma (U) | 4 (±1) |
| Crystalloid (ml) | 3000 (± 500) |
| Colloid (ml) | 1000 (± 200) |
Lowest hermoglobin (g.(g. )) )) | 9.2(±3.5) (8-13.5) |
| Intraoperative i.v dopamine or noradrenaline support | 10 % (218.7) |
Table 1: Demographic and intraoperative values.
According to the Wilcoxon signed-rank test results, the preoperative whole blood hemogram values (Median = 10.10) were statistically significantly higher than the postoperative (Median = 9.90) (Z = -2,886; p =, 004). According to the Wilcoxon signed-rank test results, the preoperative AST values (Median = 18.00) of the patients were found statistically significantly lower than the postoperative (Median= 19.00) (Z = -2.965; p = 0.003). According to the Wilcoxon signed-rank test results, there was no statistically significant difference between patients preoperative ALT values and postoperative values (Z = -1,516; p = 0.130). According to the Wilcoxon signed rank test results, the preoperative CA 19-9 values (Median= 5.54) were statistically significantly higher than the postoperative (Median = 5.50) (Z = -45.990; p < 0.001). According to the Wilcoxon signed-rank test result, the patient Na values before the operation (Median= 138.00) were found statistically significantly lower than the postoperative (Median = 139.00) (Z = -8.334; p< 0.001). According to the Wilcoxon signed-rank test results, the patients preoperative Potassium (K) values (Median= 3.89) were found to be statistically significantly higher than the postoperative (Median = 3.86) (Z = -2.598; p = 0.009). According to the Wilcoxon signed rank test results, the preoperative Ca 125 values (Median = 22.20) were found to be statistically significantly higher than the postoperative (Median = 21.00) (Z = -20.888; p< 0.001) (Table2, Figure 1). These findings obtained according to the Wilcoxon signed rank test result are shown in Table 2.
The study includes 2187 patients who were diagnosed with ovarian cancer patients who underwent debulking and cytoreductive operation in Gynecology Oncology Clinic of Zekai Tahir Burak Training and Research Hospital. The day of hospitalization varies between minimum 2 and maximum 6 days, while the average duration of hospitalization was found to be 3.42 standard deviation of 1.29 days (Table 3). Postoperatively, hospital stay and frequency percentages are given in Table 3. The length of hospital stay of patients varies between 2 days (34.2%) and 6 days (7.5%), and the length of hospital stay is usually 4 days (25.6% = 559 patients). Ca 125 values in mucinous, mixed type tumors and stage III + IV tumors were statistically significantly higher in blood than other tumor types and stage I+III over cancer (Table 4).
| Mean.±Standart Deviation | Median (Min. - Mak.) | z | P value | |
| Hb (gr/dL) | -2.886 | 0.004 | ||
| Before the operation | 10.12±1,88 | 10.10 (4.10-15.80) | ||
| After the operation | 9.99±1.31 | 9.90 (5.90-14.40) | ||
| AST | -2.965 | 0.003 | ||
| Before the operation | 23.14±21.11 | 18.00 (5.00-262.00) | ||
| After the operation | 23.00±20.62 | 19.00 (4.00-446.00) | ||
| ALT | -1.516 | 0.130 | ||
| Before the operation | 15.77±18.00 | 11.00 (2.00-181.00) | ||
| After the operation | 15.75±16.09 | 11.00 (2.00-191.00) | ||
| CA 19-9 | -45.990 | <0> | ||
| Before the operation | 5.42±1.43 | 5.54 (0.50-22.00) | ||
| After the operation | 5.37±1.40 | 5.50 (0.50-22.00) | ||
| Na | -8.341 | <0> | ||
| Before the operation | 137.52±7.84 | 138.00 (42.00-200.00) | ||
| After the operation | 138.69±3.48 | 139.00 (122.00-155.00) | ||
| K | -2.598 | 0.009 | ||
| Before the operation | 3.89±.49 | 3.89 (2.45-6.43) | ||
| After the operation | 3.87±.50 | 3.86 (2.30-6.21) | ||
| Ca125 | -20.889 | <0> | ||
| Before the operation | 148.44±314.37 | 22.20 (5.90-2000.00) | ||
| After the operation | 52.73±95.75 | 21.00 (5.90-950.00) |
Table 2: Comparison of Laboratory Parameters of Patients Before and After the Operation
| Duration of Hospital Stay (Days) | Frequency | Percentage (%) |
| 2 | 748 | 34.2 |
| 3 | 412 | 18.8 |
| 4 | 559 | 25.6 |
| 5 | 305 | 13.9 |
| 6 | 163 | 7.5 |
| Total | 2187 | 100.0 |
Table 3: Frequency and Percentage of the Patients According to Duration of Hospital Stay
| Ca 125 | P | ||
| Age group | Under 40 age | 539±390 | 0.120 |
| Above 40 age | 950±450 | ||
| Tumor type | Mucinous type (15%) | 325±230 | 0.005* |
| Serous type (70%) | 458±400 | ||
| Mix type (5%) | 400±320 | 0.003** | |
| Stage | I+III | 318±300 | 0.0001*** |
| III+IV | 1645±950 |
Table 4: Evaluation of age, stage, tumor type according to Ca 125 in maling + borderline group.
The cancer with the highest mortality among all gynecological cancers is ovarian cancer. Generally, they are classified as benign, borderline and malign according to their histological and biological activities. Sex cord-stromal tumors in the ovary are usually hormonal active (85%) [7,9]. Ovarian neoplasms remain asymptomatic for appropriate periods. Patients have ambiguous or nonspecific complaints. Although the size of residual tumor masses after surgery has been shown to be an important prognostic factor for advanced ovarian cancer, it is unclear whether it is the surgical procedure that is directly responsible for the superior outcome that is associated with less residual disease.
In clinical data, especially when the disease progresses, it can be diagnosed by acid fluid or tissue sample. Symptoms of admission are chronic and progressive compression of the pelvic structures. Most of the patients had abdominal distension, heartburn, acid swelling, nausea due to intestinal obstruction [3,10-12]. In our study, the rate of distention and acid was 80%. Ovarian cancer is the leading cause of gynecological cancer death in the United Kingdom, which causes about 11 deaths per day in the UK [13]. Lack of disease-specific symptoms during early illness makes diagnosis difficult and most women are diagnosed at an advanced stage of cancer spreading beyond the ovaries. Diagnosis at an earlier stage (Stage 1) has a better prognosis with more than 90% of patients surviving 5 years after diagnosis. To follow recurrent ovarian cancer and the re-operation decision requires great responsibility and attention. Tumor reduction procedures are very risky and complex. We have to develop strategies that can lead to early detection of ovarian cancer. There is some evidence to suggest that serial serum sampling (annual or quarterly) and selective transvaginal ultrasound screening (TVS) and selective transvaginal ultrasound screening (TVS) are a screening strategy [14,15]. In our study, we followed up our patients every 6 months with TVS and by looking at tumor markers in the blood. It is very important to monitor cytoreduction operations in preoperative, intraoperative, and postoperative periods.
There are signs of spread metastasis, such as vomiting. Patients present with malnutrition, low serum albumin, transferrin levels, and weight loss, although the abdominal environment increases. During the operation, hemodynamic changes of the patient should be monitored, fluid-electrolyte, blood, and blood product needs should be met and blood sugar monitoring should be done meticulously and carefully. Invasive arteries and central venous procedures are usually necessary for this follow-up. In large surgical cases, we should monitor electrolyte changes well and reinforce them if necessary [10,11]. In our study, postoperative hyponatremia was common. 10 patients who did not improve in the intensive care unit were given 6 % NaCl supplementation intravenously. Albumin supplementation was done in 100 patients (2.2 %). Each patient received an average of 4 ES and 4 TDP during the operation. Preoperative blood product preparation should be done well and blood bank should be contacted preoperatively.
CA 125 may be more useful in conjunction with one or more other tumor biomarkers. Additional markers could play a role if, when used with CA 125, they identify some carcinomas missed by CA 125 (i.e., they improve sensitivity), rule out false positives (i.e., improve specificity), or can detect the same cancers earlier [5,15]. Ca 125 serum values in ovarian carcinomas are highest in serous and mixed adenocarcinomas, moderate in endometrioid and clear cell carcinomas, and lowest in mucinous carcinomas. Ca 125 values are an important prognostic factor in epithelial ovarian tumors [6,15]. MJ et al. in a study conducted of CA 125 and Ca 19-9 serum levels in borderline ovarian tumors, reported that Ca19-9 was more significant in borderline tumors than Ca125 [8,15]. Ovarian cancers are the highest mortality in gynecological cancers. Also, the first symptoms are often not specific, but spreading (60%) to the pelvic and abdominal spaces was observed. A special emphasis, as it is often diagnosed at an advanced stage carries [15]. Bast et. al [16] identified CA-125 of ovarian cancer patients and since then CA-125 had been many studies investigating prognostic value. Chi et al. emphasized the relationship between preoperative CA-125 levels and optimal surgery. In this study, 43 patients (78%) of total 55 patients had undergoing suboptimal surgery, CA-125 level 500 U / ml and above, specificity was found to be 73% (17). CA 19-9 should be included if someone chooses to use serum markers in the follow-up of muesli borderline ovarian tumors. The measurement of serum tumor markers in the follow-up of patients with borderline ovarian tumors leads to early detection of recurrence in only a very small proportion of patients and the clinical value of early detection of recurrence is important for early treatment (Figure 1). CA 19-9 should be included if someone chooses to use serum markers in the follow-up of muesli borderline ovarian tumors. The measurement of serum tumor markers in the follow-up of patients with borderline ovarian tumors leads to early detection of recurrence in only a very small proportion of patients and the clinical value of early detection of recurrence is important for early treatment. Other a study was reported limit 500 U / ml as CA-125 value 62% sensitivity, 83% specificity in their studies [18]. Memarzadeh et. al reported, only CA-125 values using, in optimal surgery performed the sensitivity of CA-125 58% in predicting that it cannot be specificity 54%, positive predictive value 78%, negative predictive the value was found to be 31% and alone it is advocated that CA-125 value is not enough [18,19]. Research in recent years, CA-125 values shows that it goes to the correlation with tumor load.
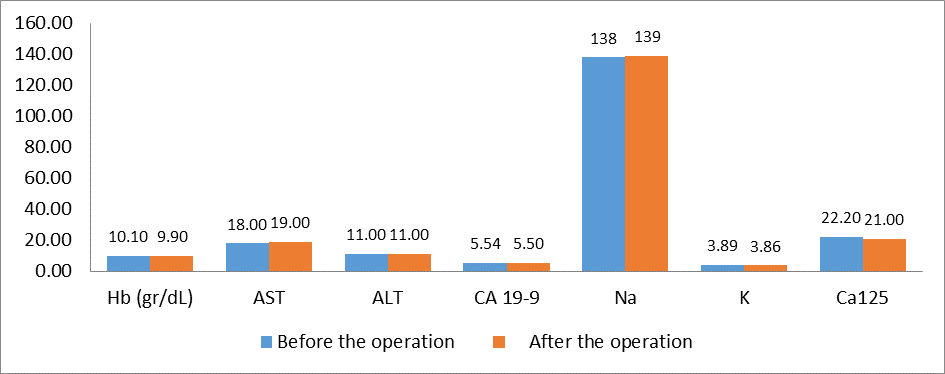
Figure 1: Median Values of Laboratory Parameters of Patients Before and After the Operation
During primary surgery for advanced stage epithelial ovarian cancer all attempts should be made to achieve complete cytoreduction. When this is not achievable, the surgical goal should be optimal (< 1 cm) residual disease. Due to the high risk of bias in the current evidence, randomized controlled trials should be performed to determine whether it is the surgical intervention or patient-related and disease-related factors that are associated with the improved survival in these groups of women. The findings of this review that women with residual disease < 1 cm still do better than women with residual disease > 1 cm should prompt the surgical community to retain this category and consider re-defining it as 'near optimal' cytoreduction, reserving the term 'suboptimal' cytoreduction to cases where the residual disease is > 1 cm (optimal/near optimal/suboptimal instead of complete/optimal/suboptimal) [18,20].
A Cochrane review did not identify any studies that compared the effectiveness and safety of secondary surgical cytoreduction to chemotherapy alone for women with recurrent epithelial ovarian cancer (20). In our study, 80 % of our patients had preoperative or postoperative adjuvant chemotherapy.
In our study, when the preoperative CA-125 value was taken as 300 U / ml limit, sensitivity was 80% and selectivity was 60% in predicting whether there would be suboptimal surgery. In addition, no significant result could be obtained between age, histopathological type and surgical type of CA-125 decrease after the operation. Optimal cytoreduction is one of the most prognostic factors in ovarian cancers. First, Griffiths et al. showed the success of cytoreductive surgery, which was demonstrated by, has been demonstrated many times over the following years [21,22]. For this reason, many authors advocate maximal effort for optimal cytoreduction.
The standard management of primary ovarian cancer is optimal cytoreductive surgery followed by platinum-based chemotherapy. Most women with primary ovarian cancer achieve remission on this combination therapy. For women achieving clinical remission after completion of initial treatment, most (60%) with advanced epithelial ovarian cancer will ultimately develop recurrent disease. However, the standard treatment of women with recurrent ovarian cancer remains poorly defined. Surgery for recurrent ovarian cancer has been suggested to be associated with increased overall survival [23].
A retrospective study evaluated the prognostic significance of the serum CA125 level after 6 cycles of systemic adjuvant chemotherapy. The median progression-free survival was 26, 14, and 10 months, and the median overall survival was 105, 42, and 37 months in group I (< 10 U/ml), group II (10-21 U/ml), and group III (> 21 U/ml) respectively [24]. One study determined whether CA125 is an independent predictor of overall survival (OS) in patients with surgically defined disease status at the end of primary therapy prior to intraperitoneal (IP) consolidation chemotherapy. When considered as a continuous variable, CA125 was a predictor of OS. Using the median CA125 level as a cut-off, OS was increased in patients with CA125 ≤ 12 U/ml (median 5.8 years) compared with > 12 (3.7 years) [25, 26]. CA125 is the gold standard tumor marker in ovarian cancer. Serum level of CA125 is used to monitor response to chemotherapy, relapse, and disease progression in ovarian cancer patients. Thus, it is reasonable to investigate whether CA125 may have utility as a prognostic indicator as well in ovarian cancer [26]. Intra - abdominal chemotherapeutic perfusion with 0.9% isotonic makes temporary significant hyponatremia and metabolic acidosis [27]. In our study, our patients were previously diagnosed with Over Ca and they completed chemotherapy programs because they were opened for the second time due to the tumor debulking operation.
Multidisciplinary teamwork is very important in ovarian cancer treatment. It should be kept in mind that the approach of anesthesiologists in the preoperative, intraoperative perioperative and postoperative periods is life-saving in patients who will undergo gynecologic-oncologic cytoreductive surgery.