AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2768-2757/162
1OGBUZ "Bratsk Children's City Hospital", Irkutsk region, Bratsk.
2Irkutsk State Medical University, Irkutsk region, Irkutsk.
3State Budgetary Healthcare Institution “Irkutsk State Regional Children’s Clinical Hospital”, Irkutsk Region, Irkutsk.
4 Irkutsk State Medical Academy of Postgraduate Education, branch of RMAPO, Irkutsk Region, Irkutsk.
*Corresponding Author: Ermachenko M.F., OGBUZ
Citation: Ermachenko M.F., Ivanov RA., Popelkov AA., Nomokonov VI., Pavlyuk RP., et al, (2025), New Coronavirus Infection as One of The Factors in The Development of Type 1 Diabetes Mellitus in Children, Journal of Clinical Surgery and Research, 5(6); DOI:10.31579/2768-2757/162
Copyright: © 2025, Ermachenko M.F. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 03 February 2025 | Accepted: 19 February 2025 | Published: 24 February 2025
Keywords: diabetes; covid-19; children
Interaction with district pediatricians and a social worker revealed that most children with repeated hospitalizations to the intensive care unit were brought up in asocial families (drinking or drug-addicted parents). The children were not given due attention, there was a violation of diet and insulin intake, which eventually led to the development of a coma. Emergency notifications about "abuse syndrome" were sent to the parents of these children.
At the time of writing (30.01.2025), 102,607,583 people in the world fell ill with the new coronavirus infection. Since the beginning of the pandemic, the mortality rate was 2.15% (2,214,783 people died). In Russia, since the beginning of the pandemic, 24,877,276 people fell ill, of which 403,360 died, the mortality rate is 1.62% [4]. In different countries, the number of sick children from newborns to 18 years of age ranges from 0.8 to 2.8% [1,2,3,4]. During the COVID-19 pandemic, many large studies have confirmed a direct relationship between the severity of the infectious disease and a history of diabetes. A meta-analysis of 8 studies involving almost 50,000 patients with COVID-19 showed that diabetes mellitus (DM) is the second most common comorbidity after hypertension [5].
According to experts, the high risk of developing infection in patients with diabetes is explained by immune disorders due to hyperglycemia and its acute and chronic consequences. In addition, elevated cytokine levels increase the risk of developing a severe form of infection [6]. Studies by Chinese scientists have found that diabetes mellitus is more common among patients with severe COVID-19 than among patients with a mild form of the disease: 16.2% versus 5.7%, and the prognosis for COV ID-19 in patients with diabetes was worse [7].
According to a number of studies, diabetes is also a risk factor for mortality in patients with COVID-19. A large national sample study showed that the mortality rate of patients with diabetes was significantly higher than that of patients without it: 10% versus 2.5% [6]. The mortality rate of patients without comorbid conditions in China was 0.9%, while in patients with diabetes it reached 7.3% [9]. A study of the clinical characteristics of deaths with COVID-19 revealed that diabetic ketoacidosis is one of the causes of patient mortality [9]. Diabetes mellitus (DM) is a risk factor for the development of severe pneumonia and septic course of viral infection, associated with the development of multiple organ failure and an increased risk of complications and death [8,9].
We noticed that in the city of Bratsk in the period 2019-2024 the number of sick children with newly diagnosed type 1 diabetes increased sharply. During the same period, outbreaks in the form of a pandemic of a new coronavirus infection were observed around the world. We decided to trace the connection between newly diagnosed diabetes and a previous illness of a new coronavirus infection. Many scientists are inclined to believe that COVID -19 attacks the cells of the pancreas, as a result of which it stops producing insulin in the required quantities. Under the influence of the corona virus, the body produces proteins whose work is called the "abnormal immune response." The body fights itself. The COVID-19 virus affects the b-cells of the pancreas, its tissue is a potential target for infection, leading to glucose metabolism disorders. This means that it can trigger the development of type 1 diabetes or cause an increase in sugar levels (decompensation of diabetes if present). It is assumed that the SARS-CoV-2 virus seriously damages the islet cells of the pancreas and contributes to the development of diabetes or its worsening. [9,10,11]
Purpose Of the Study
To analyze the reasons for the increase in the number of patients with newly diagnosed type 1 diabetes mellitus, as well as repeated admissions of such patients with a previously established diagnosis to the anesthesiology and intensive care unit in normal years and during the pandemic of a new coronavirus infection. To trace the possible relationship between a history of a new coronavirus infection and the development of type 1 diabetes mellitus in children.
In the intensive care unit of the OGBUZ "Bratsk Children's City Hospital" for 25 years, in the period from 2000 to 2024, 340 cases of sick children with the diagnosis of: Type 1 diabetes mellitus (DM type 1) aged from 1 year to 18 years were hospitalized. In 321 cases, the diagnosis upon admission was: type 1 diabetes mellitus, diabetic precoma or coma, ketoacidosis and in 19 cases the diagnosis was: type 1 diabetes, hypoglycemic coma. Of the 340 cases of hospitalization: in 138 cases, DM type 1 was diagnosed in children for the first time, and in 202 cases there were repeated hospitalizations.
Total number of patients in intensive care, number of patients with diabetes (abs., %) | Number of hospitalizations of diabetes mellitus newly diagnosed (abs.) | Number of cases of rehospitalization of diabetes (abs.) | |
| 2000 | 285; 7 (2.5%) | 2 | 5 |
| 2001 | 279; 3 (1.1%) | 1 | 2 |
| 2002 | 290; 7 (2.4%) | 3 | 4 |
| 2003 | 184; 4 (2.2%) | 2 | 2 |
| 2004 | 291; 6 (2.1%) | 1 | 5 |
| 2005 | 296; 4 (1.4%) | 2 | 2 |
| 2006 | 344; 4 (1.2%) | 2 | 2 |
| 2007 | 345; 2 (0,6%) | 1 | 1 |
| 2008 | 405; 3 (0,7%) | 2 | 1 |
| 2009 | 323; 4 (1,2%) | 3 | 1 |
| 2010 | 305; 9 (3,0%) | 7 | 2 |
| 2011 | 254; 5 (2,0%) | 3 | 2 |
| 2012 | 252; 6 (2,4%) | 1 | 5 |
| 2013 | 254; 12 (4,7%) | 5 | 7 |
| 2014 | 243;11 (4,5%) | 2 | 9 |
| 2015 | 206;17 (8,3%) | 7 | 10 |
| 2016 | 284; 12 (4,2%) | 2 | 10 |
| 2017 | 300; 16 (5,3%) | 7 | 9 |
| 2018 | 260; 26 (10,0%) | 8 | 18 |
| 2019 | 294; 28 (9,5%) | 8 | 20 |
| 2020 | 220; 22 (10,0%) | 10 | 12 |
| 2021 | 228; 36 (15,7%) | 16 | 20 |
| 2022 | 273; 41 (15,0%) | 17 | 24 |
| 2023 | 226; 24 (10.7%) | 12 | 12 |
| 2024 | 203; 31 (15.3%) | 14 | 17 |
| Total: | 6470; 340 (5.4) | 138 | 202 |
Table 1: The absolute and relative number of patients with type I diabetes treated in the intensive care unit is presented in.
Table 1 type I diabetes in the intensive care unit in comparison with the total number of ICU patients abs., (%).
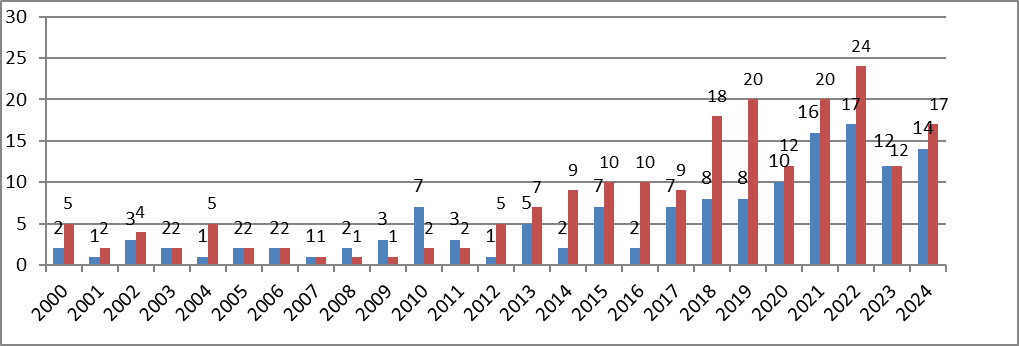
Diagram 1: Cases of hospitalization of patients with type I diabetes (primary/recurrent) years.
Comparative diagram by year of hospitalizations of patients with the diagnosis: Newly diagnosed type I diabetes and re-hospitalized patients with the established diagnosis: type I diabetes (abs.).
Note: patients who were readmitted with a diagnosis of type 1 diabetes are marked in red; patients with a diagnosis of type 1 diabetes, newly diagnosed, are marked in blue.
When analyzing Table 1 and Diagram 1, it was revealed that starting in 2020, the number of patients with newly diagnosed type 1 diabetes mellitus has increased significantly. Over 20 years (2000–2019), the increase in patients with newly diagnosed type 1 diabetes mellitus ranged from 1–8 patients per year (an average of 4 people/year). However, starting in 2020, during the “covid” years, the number of patients with newly diagnosed type 1 diabetes mellitus has increased sharply. The increase in patients in this group ranged from 10–17 patients (an average of 14 people/year). The number of re-hospitalizations with diabetes mellitus over 20 years (2000–2019) ranged from 1–20 cases (an average of 6 cases/year). For the period from 2020–2024. from 12 to 24 cases of re-hospitalization per year (on average 19 cases/year).
| Reasons for hospitalization of patients with diabetes in intensive care units | |
| Reasons for hospitalization | Number of cases, abs. (%) |
| Initial hospitalization: | |
| newly diagnosed diabetes | 138 (40.6%) |
| Rehospitalization: | |
| diet violation | 85(25.1%) |
| untimely insulin injection | 46(13.5%) |
| concomitant diseases | 71(20.8%) |
| Total: | 340 (100%) |
Table 2: Reasons for hospitalization of patients with type I diabetes in intensive care units.
Table 2 shows that the main reason for hospitalization of patients with type I diabetes in the intensive care unit is newly diagnosed type I diabetes with the development of precoma or coma - 138 patients (40.6%). Among repeated hospitalizations to the intensive care unit, dietary violation in patients with type I diabetes was 85 (25.1%), of which 75 patients (88.2%) led to the development of diabetic coma. The history of the development of the disease in these children includes the use of carbohydrates in the form of chocolate, sweets, carbonated drinks . And in 10 patients (11.8%), untimely food intake against the background of insulin injection led to the development of hypoglycemic coma . In 46 patients (13.5%), independent cancellation of insulin led to the development of diabetic coma. In 71 patients (20.8%), concomitant diseases (ARI, flu, pneumonia, covid-19) led to a "breakdown" of compensatory mechanisms against the background of selected insulin therapy and the development of diabetic coma. Our analysis showed that several patients were regularly admitted to the intensive care unit with signs of coma for several years. Over twenty-five years of observation, 19 patients moved to other cities for permanent residence. 29 patients were removed from "D" registration in
the children's clinic due to them reaching 18 years of age and switching to "D" registration in adult clinics. Interaction with district pediatricians and a social worker revealed that most children with repeated hospitalizations to the intensive care unit were brought up in asocial families (drinking or drug-addicted parents). The children were not given due attention, there was a violation of diet and insulin intake, which eventually led to the development of a coma. Emergency notifications about "abuse syndrome" were sent to the parents of these children.
When a patient with suspected diabetes is admitted to the emergency room, the patient is examined by a pediatrician, endocrinologist and resuscitator, a blood sugar test is taken according to cito . Since 2020, a PCR swab for covid-19 or an express test for covid-19 is additionally taken in the emergency room to determine the profile of the department for hospitalizing patients.
Of the 138 patients admitted to the intensive care unit with newly diagnosed diabetes mellitus and in 202 cases in patients with rehospitalization, there were manifestations of diabetic precoma or coma, as well as signs of severe metabolic acidosis.
Year
| Total number of patients with newly diagnosed diabetes and number of patients who underwent ELISA blood testing for immunoglobulins to SARS-CoV-2 | Ig M CP <0> CP from >=0.8 to <1> CP>=1.1 – positive and number of patients (abs. and %) | Ig G <10> >=10 – positive (Min – max values) and number of patients (abs. and %) |
| 2020 | 10(4; 40.0%) | neg. | 16.49 – 716.46 (4) |
| 2021 | 16(8; 50.0%) | 1.92 – 3.94 (2) | 29.08 – 689.79 (6) |
| 2022 | 17(10; 58.8) | 4.15 (1) | 28.76- 449.61 (9) |
| 2023 | 12(5;41.6%) | neg. | 15.38 – 790.79 (5) |
| 2024 | 14(8;57.1%) | 1.26 – 2.98 (1) | 12.45 – 890.35 (7) |
| Total: | 69(35; 49,5%) | 4 (5,8%) | 31 (44,9%) |
Table 3: Number of patients with newly diagnosed diabetes Type I, who underwent ELISA blood testing for immunoglobulins to SARS-CoV-2.
From 2020 to 2024, all patients diagnosed with type I diabetes mellitus underwent PCR testing for SARS-CoV-2 in the emergency department. Detection of antibodies to SARS-CoV-2 is of auxiliary importance for diagnosis of current infection and is essential for assessing the immune response to the current or a previous infection. Solution about testing for antibodies to SARS-CoV-2 was decided by the attending physician individually, based on clinical appropriateness (on average, ELISA blood test for immunoglobulins to SARS-CoV-2, performed in 11.2% of cases in 35 patients). For the period from 2020 to 2024, out of 69 patients with newly diagnosed diabetes, Type I in 14 patients (20.2%), a positive nasopharyngeal swab for PCR analysis for SARS-CoV-2 was noted. And in 35 patients who, as prescribed by a doctor, were tested for antibodies to SARS-CoV-2, a positive Ig test was noted in 4 patients (11.4%). M to SARS-CoV-2 and 31 patients (88.6%) had a positive Ig test G to SARS-CoV-2. Two patients tested positive for Ig M to SARS-CoV-2 and Ig G to SARS-CoV-2. Thus, the analysis of Table 3 shows that mild, moderate or severe COVID-19 infection in children served as a provoking factor in the development of type I diabetes in children in different age groups. Moreover, in some patients, the development of diabetes mellitus occurred in the acute stage of covid-19 (14 patients had a positive PCR test for SARS-CoV-2). In 4 patients, type I diabetes developed in the period from 7 days to 2 months after suffering from covid-19 (this is indicated by an elevated level of Ig M to SARS-CoV-2). In 31 patients, diabetes mellitus developed from 3 weeks to several months after the new coronavirus infection (this is evidenced by an increased level of Ig G to SARS-CoV-2).