AUCTORES
Globalize your Research
case report | DOI: https://doi.org/10.31579/2690-1897/253
Ferhat Abbas University. Sétif 1. Faculty of Medicine. Algeria Research Laboratory "Laboratory of Investigation and Specialized Research in Health, Environment and Innovations". Department of General Surgery; Setif University Hospital. Algeria
*Corresponding Author: Ouahab Ilhem, Ferhat Abbas University. Sétif 1. Faculty of Medicine. Algeria Research Laboratory
Citation: Ouahab Ilhem, (2025), Neuroendocrine Tumor of the Terminal Ileum: A Case Report, J, Surgical Case Reports and Images, 8(5); DOI:10.31579/2690-1897/253
Copyright: © 2025, Ouahab Ilhem. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 05 May 2025 | Accepted: 16 May 2025 | Published: 23 May 2025
Keywords: intestinal neuroendocrine tumor; surgical resection; immunohistochemistry
Neuroendocrine tumors are rare. They are increasingly diagnosed thanks to the development of investigative methods. Surgery is the standard treatment. We report the case of a patient who presented with an intestinal neuroendocrine tumor. Abdominal pain and sub-occlusive syndromes were the reason for consultation. The diagnosis of neoplasia was suspect. Surgical resection was the radical treatment. The anatomopathological examination of the surgical specimen confirmed the diagnosis of intestinal neuroendocrine tumor. Currently, the patient is alive without recurrence.
Tumors (NETs) are a group of rare tumors that develop from cells of the neuroendocrine system throughout the body [1]. Formerly called carcinoid tumors, these tumors are neuroendocrine neoplasms that form from the disordered development of cells of the neuroendocrine system . They produce excessive levels of hormone-mimicking substances, resulting in carcinoid syndrome. which includes symptoms specific to the production of these substances [2] . They can be of genetic origin. These tumors are rare, 2 to 5 new cases per year per 100,000 people. Currently, neuroendocrine tumors are increasingly diagnosed due to the development of diagnostic methods and advances in imaging. Neuroendocrine tumors occur in both men and women, generally aged 50 to 60, although they can affect people of any age [3]. The positive diagnosis is based on morphological and immunohistochemical arguments. The risk of progression is determined by the proliferative capacities of the lesion. There are therapeutic weapons that can slow down the disease, in this case targeted therapies using nuclear medicine, which promise good results. The prognosis for neuroendocrine tumors seems better. The objective of this observation is to report the case of a patient who presented with an intestinal neuroendocrine tumor by showing the clinical, paraclinical, anatomopathological, therapeutic and evolutionary aspects by evaluating the interest of immunohistochemistry for the diagnosis of digestive neuroendocrine tumors.
A 43-year-old obese man with no notable history had consulted for abdominal pain that appeared 3 months previously and then repeated sub-occlusive syndromes. The clinical examination was without abnormalities. An abdominal ultrasound supplemented by a CT scan revealed the presence of a mass in the terminal ileum. An ileocolonoscopy objectified a voluminous lesion under the terminal ileal mucosa with an erythematous and erosive mucosa. Biopsies were performed. The results were in favor of a leiomyoma. The patient was operated on where he benefited from an ileocecal resection with immediate restoration of the end-to-side ileocolonic digestive continuity. The postoperative course was uneventful and the patient was discharged on the 5th postoperative day. The pathological examination and immunohistochemistry confirmed the diagnosis of an intestinal neuroendocrine tumor. A whole-body octreoscintigraphy did not reveal any other localizations. The patient is still alive without recurrence.

Figure 1: CT image of the nodule at the terminal ileum.
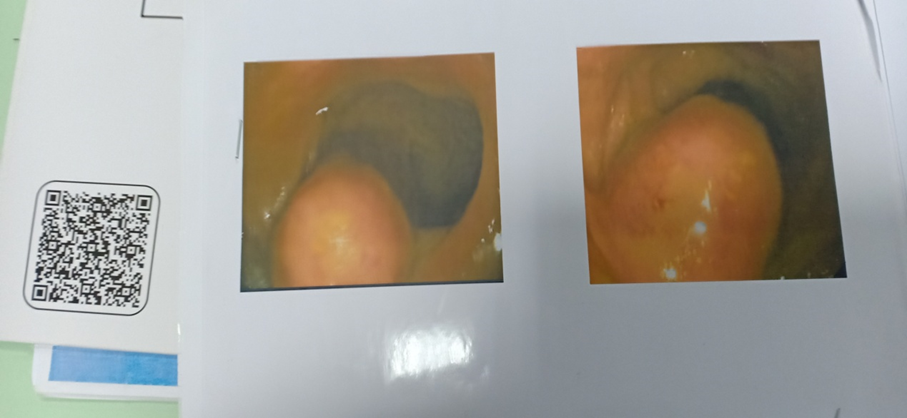
Figure 2: Endoscopic image of the tumor at the ileocecal valve level.
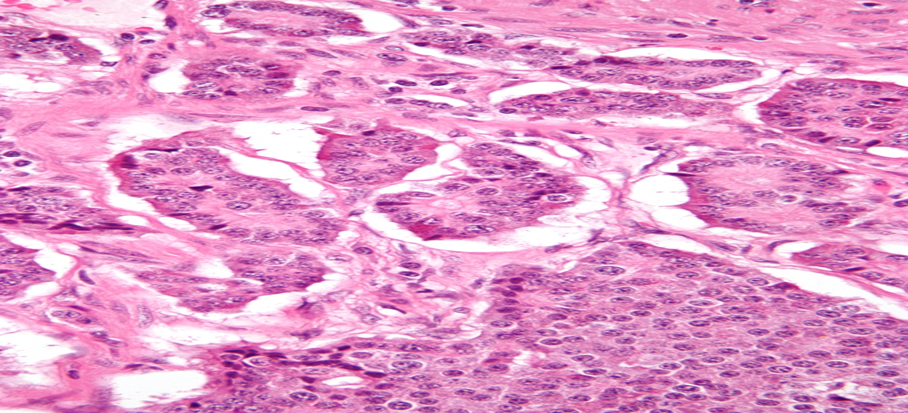
Figure 3: Histological image of a neuroendocrine tumor of the small intestine.
Discussion
Neuroendocrine tumors represent 1 to 2% of all digestive tumors [4]. They constitute a heterogeneous group of neoplastic lesions, which differ from each other in their secretory and functional properties, their pathogenic mechanisms, their clinical presentations, their evolution and their prognosis. The incidence of these tumors is constantly increasing [5]. This can be explained by the development of new specific imaging techniques and by the application of immunohistochemistry (IHC) techniques to confirm the diagnosis of neuroendocrine tumors. Neuroendocrine tumors can occur anywhere in the digestive tract (from the esophagus to the anus), in the pancreas and, exceptionally, in the liver and gallbladder [6]. Neuroendocrine tumors develop in a very variable manner. They can be present for several years without causing the slightest problem [7]. The clinical manifestations of neuroendocrine tumors will be linked to their location, their functional or non-functional nature and their aggressiveness [8]. A neuroendocrine tumor can also be discovered incidentally during an imaging examination. Our patient had abdominal pain with sub-occlusive syndromes that evolved for approximately 3 months. These signs are not very suggestive, as they can exist in many other conditions, particularly benign ones. Only additional examinations can lead to a diagnosis. In our case, the abdominal pain was constant and there were no clinical manifestations related to tumor hormonal secretion. The latter can be varied, such as diarrhea, abdominal cramps, skin flushing, burning in the stomach, etc. The clinical examination was poor since our patient was obese. The clinical examination can objectify various signs related either to a tumor syndrome (abdominal mass, liver metastases, ascites, etc.), or to a hormonal hypersecretion syndrome (skin rash, weight loss, dehydration, etc.) when it exists. The practice of imaging examinations aims to find the initial site of the tumor, to make an extension assessment and to follow the evolution of the tumor. Our patient had benefited from an ultrasound coupled with a CT scan. They showed a mass at the level of the terminal ileum. The CT scan can characterize the tumor and also to make an assessment of the extension of the disease. The anatomopathological examination of a preoperative biopsy had confirmed the neoplasia of the lesion. The treatment was mainly surgical, which included an ileocecal resection removing 2 cm on either side of the tumor. The restoration of digestive continuity was carried out at the same time as surgery by an end-to-side ileocolonic anastomosis. The histological study of the surgical specimen confirmed the diagnosis of the digestive neuroendocrine tumor. Indeed, the histological results were in favor of a well-differentiated G 2 neuroendocrine tumor of the ileum (WHO 2017) with benign follicular hyperplasia of the Payer areas of the ileocecal valve on immunohistochemistry. The anatomopathological examination makes it possible to confirm the diagnosis of neuroendocrine tumor and to determine the histoprognostic factors: Proliferation index (Ki67) and mitotic index [9]. The diagnosis is based on macroscopic, histological, histochemical and immunohistochemical arguments [10]. The neuroendocrine tumor of the small intestine is often small, barely visible, identifiable by palpation of the specimen in the form of a firm nodule embedded in the wall in 1/3 of cases [11]. This was the case for the macroscopic appearance of the lesion in our patient where the tumor was approximately 2 centimeters below the intestinal mucosa. The main prognostic factor for neuroendocrine tumors is the tumor stage. Histological grade and tumor differentiation are major prognostic factors common to neuroendocrine tumors [12]. An endocrinology opinion was requested where a whole-body octreoscintigraphy was performed. It showed no metastasis of the primary lesion. Currently, the patient is in good health.
Neuroendocrine tumors are rare.
The diagnosis is radiopathological. It depends essentially on the histological examination associated with immunohistochemistry. Radical resection of the tumor is the treatment of choice, thus ensuring a good long-term prognosis.
The authors declare no conflicts of interest.