AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2578-8965/262
¹ Consultant at Duhok Obstetrics and Gynaecology Teaching Hospital, Kurdistan Region, Dohuk city, Iraq.
² Specialist at Duhok Obstetrics and Gynaecology Teaching Hospital, Kurdistan Region, Dohuk city, Iraq.
³ Consultant at Neonatal Intensive Care Unit/ Hive Paediatrics Teaching Hospital / Kurdistan Region, Dohuk city, Iraq.
*Corresponding Author: Nazdar Raouf, Consultant at Duhok Obstetrics and Gynaecology Teaching Hospital, Kurdistan Region, Dohuk city, Iraq.
Citation: Nazdar Raouf, Amal Abdulhakeem, Hameed Rekani, (2025), Maternal and Neonatal Outcomes in Women Complicated with Previous Complete Rupture of the Unscarred Gravid Uterus, J. Obstetrics Gynecology and Reproductive Sciences, 9(3) DOI:10.31579/2578-8965/262
Copyright: © 2025, Nazdar Raouf. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 05 March 2025 | Accepted: 12 March 2025 | Published: 19 March 2025
Keywords: pregnancy outcome; recurrence rupture; unscarred rupture
Background: Uterine rupture during gestation can be lethal for both the mother and the fetus. Unscarred uterine rupture, however rare, is increasingly prevalent compared to scarred uterine rupture and is associated with heightened maternal and neonatal morbidity.
Objective: The study was design to evaluate the outcomes for mothers and newborns in women complicated with previous complete rupture of the unscarred gravid Uterus.
Methods: A prospective study involving human populations was conducted at the Duhok Obstetrics and Gynaecology Teaching Hospital in Iraqi Kurdistan during a five-year period, from September 2019 to September 2024. Twenty pregnant women with a singleton fetus at ≥28 weeks gestation who had previously experienced a total rupture of the unscarred uterus were included in the study. The study eliminated all cases of uterine dehiscence, abnormal fetus twine pregnancy, previous caesarean delivery, and any surgical procedures performed between rupture repair and the subsequent pregnancy. Every three weeks, women with this history are examined, every woman is admitted to the hospital between weeks 30 and 34 of pregnancy, or sooner if she has uterine contractions prior to receiving a course of corticosteroid medication. At 34 and 36 weeks, elective caesarean deliveries are scheduled. The data was collected from pregnant women included the demographic features, maternal outcomes, neonatal outcomes and characteristics of previous ruptures.
Results: The mean maternal age was (29 ± 4.0), with (60%) having a BMI of <25.0and (40%) having a BMI of ≥25.0. Sixteen cases (80%) of pregnancies ended in delivery between weeks 34 and 36, while 4 cases (20%) ended between weeks 28 and 33. Delivery occurred by elective CD. No maternal deaths, repeated uterine ruptures, or intensive care unit admissions were noted. Twenty babies were born. In 16 cases (80%), the baby's sex was male, and in 4 cases (20%), it was female, fourteen (70%) babies had a pgar score at 5 minutes of seven or higher. Among the 20 women, rupture was more common in posterior wall, previous ruptures resulted in 11 (55%) of perinatal deaths.
Conclusions: Pregnancies following a complete unscarred uterine rupture proceed without significant maternal or fetal complications, upon intensive clinical observation.
Uterine rupture during pregnancy can be fatal for both the mother and the fetus. Women who have previously had a transmyometrial surgical incision usually for a caesarean delivery (CD)are more likely to experience ruptures. Although it is uncommon, unscarred uterine rupture is becoming more common, in comparison to cases of rupture of the scarred uterus, and it is linked to increased significant maternal and newborn morbidity [1].
In countries with limited resources, when timely access to caesarean and instrument-assisted vaginal birth is not often accessible for the management of obstructed labour, the incidence of rupture of the unscarred uterus is higher [2].
Trauma, inherited or acquired myometrial weakness can result in the rupture of an unscarred uterus [3,4]. Dystocia that causes delayed labour, uterotonic medication exposure, placenta accreta, multiparity, multiple gestations, and advanced mother age are all contributing factors [1, 5].
Since intrapartum rupture is an uncommon and unexpected occurrence, a strong index of suspicion is needed to diagnose it in women with an unscarred uterus. During a laparotomy, the diagnosis of uterine rupture is usually determined by visualising total disruption of all uterine layers together with active bleeding. Since fetal heart rate anomalies frequently signal urgent delivery in these individuals, a preoperative provisional diagnosis of rupture is not crucial. However, in certain instances, symptoms could be mild [6,7].
Whether or not uterine rupture is suspected, the majority of patients' decisions to have a caesarean delivery are mostly influenced by an irregular fetal heart rate pattern. The clinical situation's urgency and whether upper abdominal pathology is suspected prior to surgery determine the type of incision and anaesthesia to use [8,9].
Uterine rupture can lead to multiple complications, including severe hemorrhage, bladder laceration, hysterectomy, and perinatal death or morbidity from prematurity. [10,11,12].
The decision to perform hysterectomy or repair the defect is based on a combination of factors, including the patient's desire for future pregnancy, the extent of uterine damage from the rupture, the patient's intraoperative hemodynamic and anesthetic stability, and the skill of the surgeon for repairing a complicated rupture. As with any hysterotomy repair, a two- or three-layer closure with an absorbable suture is a suitable method if the defect is fixed. It is recommend an intraoperative consultation with a skilled urologic surgeon if the cut spreads to the bladder or if there is any suspicion of ureteral harm from the laceration or its treatment [7,13,14].
Recurrent rupture is more likely to occur in a subsequent pregnancy. The place of rupture affects the risk; fundal rupture is probably the site with the highest risk. After the rupture of the unscarred uterus has been repaired, it is recommend that women who wish to become pregnant wait at least 18 months between pregnancies. Recurrent rupture is unpredictable and can happen as early as the second trimester. The majority of obstetricians advise caesarean birth and time the delivery before labour begins in an effort to lower the risk of repeated rupture. There is disagreement on the best time to deliver. [15-17].
A prospective study involving human populations was conducted at the Duhok Obstetrics and Gynaecology Teaching Hospital in Iraqi Kurdistan during a five-year period, from September 2019 to September 2024. This study was authorised by the Duhok Obstetrics and Gynecology Teaching Hospital's Committee for Scientific Research. Every participant provided written informed permission.
The study comprised twenty pregnant women with a singleton fetus at or beyond 28 weeks gestation who had previously suffered a complete rupture of an unscarred uterus. The study eliminated all cases of uterine dehiscence, abnormal fetus twine pregnancy, previous caesarean delivery, and any surgical procedures performed between rupture repair and the subsequent pregnancy.
The rupture of all layers of the uterine wall, including the serosa and amniotic membranes, was referred to as complete rupture. Every three weeks, women with this history are examined, and ultrasound is used to check the integrity of the lower segment, placental position, and fetal growth. Every woman is admitted to the hospital between weeks 30 and 34 of pregnancy, or sooner if she has uterine contractions prior to receiving a course of corticosteroid medication for fetal maturation. At 34 and 36 weeks, elective caesarean deliveries are scheduled if there are no complications.
The data was collected from pregnant women included the demographic features, maternal outcomes, neonatal outcomes and characteristics of previous ruptures.
Demographic features included maternal age, pre-pregnancy body mass index (BMI) (kg/m2), parity, antenatal care and inter-delivery interval (IDI), which is defined by the period between consecutive live births.
Maternal outcomes were measured by grouping the gestational age at delivery into weeks 28–33 and 34–36, classifying the urgency of CD into elective and emergency CD, peripartum hysterectomy, ruptured uterus, morbidly adherent placenta, maternal admission to the intensive care unit (ICU), and maternal death.
The number of newborns, sex, birth weight, Apgar scores, stillbirth, early neonatal mortality, and NICU admission status were among the neonatal outcomes that were measured.
The location of the rupture, the gestational age at rupture, the timing of diagnosis (during CD or after delivery), and the existence of neonatal death were all characteristics of prior ruptures.
Current versions of the software program (SPSS) were used to collect and statistically analysed the data. Nominal variables were interpreted as number and percentage (%), while quantitative variables were expressed as mean ± standard deviation.
The study included twenty pregnant women with a previous history of complete rupture of the unscarred uterus between September 2019 and September 2024.
Table 1 provides an overview of the demographic characteristics of pregnant woman with previous complete rupture of the gravid unscarred Uterus. The mean maternal age was (29 ± 4.0), with 12 cases (60%) having a BMI of <25.0and 8 cases (40%) having a BMI of ≥25.0. woman with previous complete rupture of the unscarred Uterus was noted more in multiparous women (95%) and only one primiparous case was referred from the ruler area due to labourdystoscia, Nineteen cases (95%) had their antenatal care. Seventeen cases (85%) they had IDI of ≥4 years.
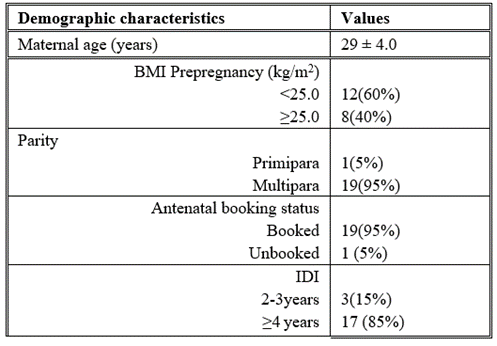
Table 1: Demographic characteristics of pregnant woman with previous complete rupture of the unscarred Gravid uterus (no.20)
Quantitative variables presented as mean ± SD, nominal variables as number (percent).
Table 2 provides the maternal outcomes among pregnant woman with previous complete rupture of the gravid unscarred uterus. Sixteen cases (80%) of pregnancies ended in delivery between weeks 34 and 36, while 4 cases (20%) ended between weeks 28 and 33. Delivery occurred by elective CD in 15 cases (75%) and by emergency CD in 5 cases (25%).In one case, the placenta was percreta a peripartum hysterectomy was performed , and the patients were given two pints of blood. No maternal deaths, repeated uterine ruptures, or intensive care unit admissions were noted.
| Maternal outcomes | Values |
Gestational age at delivery 34–36weeks 28–33weeks |
16 (80%) 4 (20%) |
Urgency of CD Emergency CD Elective CD |
5(25%) 15(75%) |
| Morbidly adherent placenta | 1 (5%) |
| Rupture uterus | 0(0%) |
| Peripartum hysterctomy | 1 (5%) |
| Admission to ICU | 0(0%) |
| Maternal death | 0(0%) |
Table 2: Maternal outcomes among pregnant woman with previous complete rupture of the unscarred Gravid Uterus. (no.20) nominal variables as number (percent).
Table 3 Summarises the neonatal outcomes among pregnant woman with previous complete rupture of the gravid unscarred uterus. Twenty babies were born. In 16 cases (80%), the baby's sex was male, and in 4 cases (20%), it was female. The newborn's weight ranged from 1.4 to 2.2 kg; in 7 cases (35%), it was between 2.3 and 3,0 kg, in 13cases (65%), fourteen (70%) babies had a pgar score at 5 minutes of seven or higher, whereas six (30%) babies had a score between two and six. Additionally, 4 cases (20%) were admitted to the neonatal intensive care unit (NICU). while no cases of stillbirth and early neonatal death had been reported.
| Neonatal Outcomes | Values |
| Numbers of newborn | 20 |
Sex Male Female |
16(80%) 4(20%) |
Birth weight 1.4-2.2kg 2.3-3.0kg |
7 (35 %) 13 (65 %) |
Apgar score at 5 minute ≥7 2-6 |
14 (70%) 6(30%) |
| NICU admission | 4(20%) |
Table 3: neonatal outcomes among pregnant woman with previous complete rupture of the unscarred Gravid uterus (no.20). Nominal variables as number (percent).
Table 4 provides the characteristics of previous complete rupture of the gravid unscarred uterus. Among the 20 women, rupture was more common in posterior wall (35%). In one case (5%) the previous ruptures occurred at 36–37 weeks while in 8(40%) cases ruptures occurred at 37–38 weeks and in 11 cases (55%) ruptures was at 39–40 weeks. In 8 cases (40%) rupture detected during CD, while in 12 cases (60%) was before the delivery. Previous ruptures resulted in 11 (55%) of perinatal deaths.
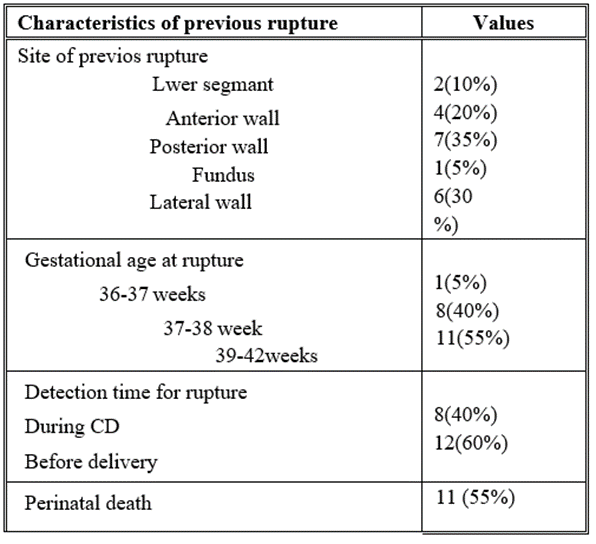
Table 4: provides the characteristics of previous complete rupture of the Gravid unscarred uterus(no.20). Nominal variables as number (percent).
Uterine rupture is a potentially life-threatening condition for the mother and the fetus and can be managed through hysterectomy as well as repair but the patients frequently show interest in getting pregnant again [18,19].
In this study ruptures was common in multiparty as it is a well-described risk factor to malpresentation and unstable lie, similar finding was reported in one study [20].
Our study's results are encouraging regarding the progression of pregnancies; following a complete rupture, there were no subsequent ruptures; nevertheless, one case of placenta percreta led to peripartum hsterctomy, no maternal death, and favorable neonatal outcomes. One study that examined 20 patients observed a 5% scar dehiscence rate, no recurrences, and no severe maternal morbidity [21]. Another study examined the results of seven continuing pregnancies following uterine rupture over a ten-year period. They found that there were eight live born, no hysterectomies, and no recurrences of uterine rupture [22]. According to other research, 12 pregnancies following a full rupture of the uterus resulted in a recurrence of the rupture and infant death [23].
This study found that the placenta accrete syndrome risk rate was5% somewhat more than the (2.3%) placenta accrete rate following the previous four CDs (2.3%) [24].
The current study demonstrated that timing the delivery at an earlier gestational age was important to reduce risk of rupture [16]. While a Beirut study involving 24 pregnancies found no significant difference in the mean or median gestational age between pregnancies in which rupture occurred and those in which it did not, but according to one study, the majority of recurrent ruptures happened after 36 weeks [25].
There was administration of corticosteroids to all women for reducing complication of respiratory distress. In one study there was assessment of lung maturity or administration of corticosteroid if CS was planned before 37 weeks [24].
Our research revealed that the mode of delivery was CD in all cases. In one study reported cesarean in 43 cases, they had 4 recurrent ruptures; all occurred in vaginal deliveries [16].
Strengths and limitations
Our study's main advantages are that it was conducted at tertiary centers in Duhok City, which received cases for follow-up with an experienced obstetrician. One must take into account the two limitations of this study. Firstly, there was not enough sample size. Secondly, no control group was included in our study.
Pregnancies following a complete unscarred uterine rupture proceed without significant maternal or fetal complications, upon intensive clinical observation, elective CD prior to labour between weeks 34 and 36, and preceded by administration of corticosteroid for pulmonary maturity.
'Not applicable' for that section
Acknowledgments: We would like to thank everyone involved in the collection and interpretation of the data.
Authors' contributions: 'Not applicable' for that section
Funding: There was no source of funding for this research
Availability of data and material: 'Not applicable' for that section
Ethics approval and consent to participate: The ethical approval from the local ethics and scientific committee was obtained. The written informed consent of all the participants was obtained.
Consent for publication: 'Not applicable' for that section
Competing interests: There are no conflicts of interest to declare