AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2692-9759/151
Department of Cardiac Rehabilitation, National Medical Center 20 de Noviembre Institute of Social Security and Services for State Workers Mexican Faculty of Medicine La Salle University, Mexico.
*Corresponding Author: Lara-Vargas Jorge A, Department of Cardiac Rehabilitation, National Medical Center 20 de Noviembre Institute of Social Security and Services for State Workers Mexican Faculty of Medicine La Salle University, Mexico.
Citation: Machuca-Loeza Maricruz G, Lara-Vargas Jorge A, Cárdenas-Beltrán Luis C, Diaz-Zepeda Jennifer S, González-Bonilla Mezthly B., et al., (2025), Improvement of Cardiorespiratory Fitness, Ischemic Threshold, And Quality of Life in Patients with Coronary Ectasia After a Cardiac Rehabilitation Program, Cardiology Research and Reports, 7(1); DOI:10.31579/2692-9759/151
Copyright: © 2025, Lara-Vargas Jorge A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 24 December 2024 | Accepted: 06 January 2025 | Published: 16 January 2025
Keywords: atrial fibrillation; acute coronary syndrome; predictive factors
Background and Aim: Coronary ectasia (CE) is a condition found in various types of heart diseases. It is characterized by alterations in coronary blood flow, endothelial dysfunction, arterial thrombosis, ischemia, arrhythmias, and heart failure. It has been shown that cardiac rehabilitation (CR) based on concurrent training has resulted in anti-inflammatory effects at the coronary endothelium level, as well as cardiovascular, pulmonary, and muscular adaptations that increases peak oxygen consumption (VO2 peak). However, this effect is unknown in patients with CE. The aim of this study is to determine the effects of a cardiac rehabilitation program on cardiorespiratory fitness, ischemic threshold, and quality of life in patients with coronary ectasia.
Materials and Methods: A quasi-experimental study was conducted in phase II of the CR program. Patients of both genders, aged over 18 years, with all types of stable heart diseases, cardiac interventions, and the presence of intracardiac devices were included, while patients with contraindications for cardiopulmonary exercise testing or the CR program were excluded.
Results: Nineteen patients with an average age of 64.6 ± 7.7 years were included, with 84% being male. 78% had a history of ischemic heart disease. After the program, a statistically significant gain was observed for VO2 peak (p<0.001), METs-load (p<0.001), oxygen pulse (p=0.005), obtained from a cardiopulmonary test in a BTL CardioPoint-Ergo and Pisto XP model; and health-related quality of life obtained from the SF-36 questionnaire (p=0.003). A non-significant decrease was observed for the VE/VCO2 slope (p=0.412). The presence of ischemic threshold was noted in six patients, of which three showed remissions. No adverse events associated with CR were observed.
Conclusions: Cardiac rehabilitation programs based on concurrent physical training are safe and promote improvements in cardiorespiratory fitness, prognostic ergoespirometric variables, possible ischemic threshold remission, symptom relief, and improve quality of life in patients with coronary ectasia associated with other types of heart disease.
Coronary ectasia (CE) is the diffuse dilation of up to 1.5 times the normal size of the artery, with an incidence of 1.5% to 5%. Classic cardiovascular risk factors are implicated in 50% of cases; however, up to 30% are associated with congenital heart diseases, vasculitis, and valvular diseases [1]. CE has been primarily associated with thrombotic events, especially acute myocardial infarction due to slow coronary flow [2]. Evidence supports the benefits of physical training in patients with ischemic heart disease through cardiac rehabilitation (CR) programs, as well as its effects on the fibrinolytic system and platelet aggregation as part of long-term adaptations in various subgroups of the disease (revascularized, surgical, non-revascularized, and some other populations of non-obstructive coronary disease), but its effects have not been fully elucidated in CE [3]. Damage from ischemic events can be reduced as a chronic adaptation to multiple training sessions through angiogenesis, arterial remodeling, reduction of collagen deposits in arterial walls, and increased production of endothelial nitric oxide (NO) [4].
CR is a therapeutic intervention performed by an interdisciplinary team, based on physical training, control of cardiovascular risk factors, psycho-emotional intervention, nutritional support, and improvement of therapeutic adherence, and is classified as Class I in the comprehensive treatment of patients who have suffered an acute coronary event [5], heart failure [6], pulmonary hypertension [7], among other heart diseases associated with CE. However, there is no evidence on CR programs in this latter group of patients. Keteyian et al. demonstrated improvements in peak oxygen consumption (VO2 peak) in patients who completed a CR program following revascularization surgery or percutaneous coronary intervention, finding that for each 1 MET increased in VO2 peak, there was a reduction of up to 17% in all-cause mortality in men and 15% in women, although the effects of physical training on atherogenesis are insufficient to explain the pathophysiological conditions of CE [8].
Histologically, in this population, there is a higher percentage of the 5A/5A polymorphism of matrix metalloproteinase-3 (MMP-3), as well as higher concentrations of metalloproteinase-2 (MMP-2) and matrix metalloproteinase-9 (MMP-9), which lead to greater lysis of proteoglycans, laminin, fibronectin, and collagen, generating excessive dilation of the vessel wall, loss of elastic components, and replacement of smooth muscle with hyalinized collagen [9] [10]. Coronary ectasia characteristically presents with depletion of the antioxidant glutathione, increased production of intercellular adhesion molecule type 1 (ICAM-1) and vascular endothelial growth factor (VEGF), resulting in increased generation of reactive oxygen species, endothelial dysfunction, decreased production of nitric oxide (NO), vascular stiffness, and coronary arterial complications such as acute myocardial infarction, stable angina, and left ventricular dysfunction [11,12]. Compared to atherosclerotic coronary disease, there are higher rates of urgent revascularization within a year, persistence of angina, and slow flow in this patient population [13,14]. Lo Presti et al. determined in their systematic review the effect of long-term physical training (3 to 24 weeks) on serum concentrations of metalloproteinases in sedentary women and patients with coronary disease, finding that all training programs reduced blood concentrations of MMP-9 and MMP-2. Perhaps, physical training increases plasma Sirtuin 1 levels, an anti-aging gene with relevance to the improvement in lung and heart function in patients with coronary ectasia. [15]. Our hypothesis is based on the capacity of concurrent training to decrease pro-inflammatory markers associated with arterial dilation, such as metalloproteinases, ICAM-1, VEGF and increase Sirtuin 1 in patients with CE [16]. Therefore, the objective of this study is to determine whether the cardiac rehabilitation program can improve cardiorespiratory fitness, ischemic threshold, and health-related quality of life in patients with coronary ectasia.
A quasi-experimental study was conducted in phase II of the CR program. Patients of either gender, aged over 18 years, with CE identified by coronary angiography, either with a history of acute myocardial infarction, with or without surgical or percutaneous revascularization, intervened and non-intervened valvular disease without hemodynamic repercussions, asymptomatic non-obstructive or obstructive hypertrophic cardiomyopathy, presence of intracardiac devices, history of non-sustained supraventricular or ventricular arrhythmias, pulmonary hypertension, congenital heart disease, chronic heart failure, and who completed the CR program were included. Exclusion criteria were pregnant patients, arrhythmias with hemodynamic instability, acute heart failure, acute coronary syndrome in the last 7 days, acute pulmonary thromboembolism, unstable angina, myocarditis, pericarditis, symptomatic left ventricular outflow tract obstruction, aortic dissection, dissecting aortic aneurysm, valvular diseases with hemodynamic repercussions, symptomatic bradycardia, second and third-degree atrioventricular block and uncontrolled hypertension.
Measurement of Ergometric Variables
Upon admission and discharge from phase II of the CR program, cardiopulmonary exercise testing (CPET) with incremental load limited by symptoms (peripheral fatigue, dyspnea, angina, nausea, or patient request) was performed on all patients. Calibration of volumes and gases in a BTL Cardio Point-Ergo and Pisto XP model, with both carbon dioxide and oxygen, was conducted. Prior to the measurement of expired gases, spirometry was performed in a standing position with 3 repetitions for the adequate measurement of volumes and lung capacities. An indirect calorimetry measurement was taken throughout the test. Patients were asked to complete a 4-6 hour fast before the test, and according to interview, medical history, and physical examination, specific protocols on the treadmill were determined for each patient based on their physical capacity (modified Bruce ramp or modified Naughton ramp). A constant measurement of oxygen consumption (VO2), carbon dioxide production (VCO2), oxygen pulse using the formula VO2/HR (VO2/heart rate), and the ventilatory efficiency variable (VE/VCO2) was obtained. The test was considered maximal if at least one of the following criteria was met: RER ≥ 1.15 and/or ≥ 85% of the predicted maximum heart rate for age. The presence of ischemic threshold was evaluated, defined as the appearance of angina (or its equivalent) and/or ST segment depression measured at 80 ms from the J point, having a horizontal or descending slope, in at least 3 consecutive beats across two continuous leads, or the occurrence of angina during incremental exercise. Beyond CPET, physiotherapists of the program assessed physical qualities by measuring strength, balance, flexibility, and coordination, with the short physical fitness test. Once this initial test was concluded, the specialist in cardiac rehabilitation conducted the risk stratification and exercise prescription.
Structure of the Phase II CR Program
After the initial evaluation and risk stratification, a prescription for aerobic and resistance training was established. The concurrent training occurred 3 times a week, with a total program duration of 4 or 6 weeks according to the cardiorespiratory fitness obtained from CPET. Aerobic training sessions included a warm-up phase of 5 minutes, followed by a main phase of moderate intensity lasting 20 minutes at 70% of HRR or at 65% of VO2p, targeting a Borg scale of 12 to 13, and concluding with 5 minutes of cool down. Progression was made based on each training session and patient assessment. For resistance training, an active warm-up phase of 5 minutes was followed by a main phase consisting of 10 to 15 repetitions per muscle group, 3 sets, with a training prescription of 30% of the maximum repetition for the upper body and 40% for the lower body, finishing with flexibility and relaxation exercises during the cool down. Blood pressure was measured before and during the main phase of both training and upon completion of the cool down. Continuous monitoring of heart rate and oxygen saturation was performed. All sessions were supervised by specialists in the field.
Patients were integrated into a virtual group for respiratory muscle therapy sessions conducted by sports physicians and physical therapists, lasting 30 minutes. They also received educational sessions on cardiovascular disease, risk factors, nutritional topics, psycho-emotional health, sexuality, and mindfulness to improve therapeutic adherence in phase II patients and enhance their transition to phase III. Additionally, two nutritional counseling appointments were provided, one at the beginning and one at the end of the program, where body composition was determined by skinfold measurement, nutritional strategies in accordance with the underlying disease were provided, and a meal plan was delivered.
Descriptive analysis of demographic characteristics, comorbidities, type of heart disease, and medications was performed using measures of central tendency (means), absolute values (n), and percentages. CPET variables were categorized as qualitative and quantitative. Qualitative variables were studied with absolute values (n) and percentages. Quantitative variables were analyzed using standard deviation and percentage change. For inferential analysis and comparison of quantitative variable data, the paired Student's t-test was used. Statistical significance was defined as a p-value less than 0.05. The data analysis was conducted using SPSS version V23 (IBM 2020).
Throughout Phase II, 19 patients were recruited, the majority of whom were male (84%), with a mean age of 64.6 ± 7.7 years. 63% of patients received a program lasting 6 weeks, while the rest was 4 weeks. Among comorbidities, 73% presented obesity and hypertension, 68% dyslipidemia, 52% smoking, and 47% diabetes mellitus. 78% of patients had ischemic heart disease, with 52% undergoing percutaneous coronary intervention (PCI); 5% experienced no-reflow phenomenon, and 21% required thrombus aspiration. Two patients (10%) had surgical revascularization. Among the included patients, 47% had heart failure. In terms of structural characteristics assessed by echocardiogram, 73% of all patients had an ejection fraction (EF) ≥ 50%, and 21% had an EF between 31% and 49%. Regarding medications, 94% were being treated with statins, 89% with antiplatelet agents, 63% with beta-blockers, and 31% with oral anticoagulants. The remaining characteristics are presented in Table 1.
Table 1: Demographic characteristics of the population.
| Variable | n=19 |
| Demographic | |
| Age (years) | 64.6±7.7 |
| Gender n (%) | |
| Female n (%) | 3 (15) |
| Male n (%) | 16 (84) |
| Duration of the CR program | |
| 4 weeks n (%) | 12 (63) |
| 6 weeks n (%) | 7 (36) |
| Comorbidties | |
| Obesity n (%) | 14 (73) |
| Arterial hypertension n (%) | 14 (73) |
| Dyslipidemia n (%) | 13 (68) |
| Smoking n (%) | 10 (52) |
| Diabetes n (%) | 9 (47) |
| Types of heartdisease | |
| Ischemic heart disease n (%) | 15 (78) |
| ICP n (%) | 10 (52) |
| Thrombus aspiration n (%) | 4 (21) |
| No-reflow phenomenon n (%) | 1 (5) |
| CRVC n (%) | 2 (10) |
| Chronic Heart Failure n (%) | 9 (47) |
| EF ≥ 50% n (%) | 14 (73) |
| EF 31 a 49% n (%) | 4 (21) |
| EF ≤ 30% n (%) | 1 (5) |
| Others | |
| Tricuspid regurgitation n (%) | 3 (15) |
| Aortic stenosis TAVR n (%) | 2 (10) |
| Mitral regurgitation with mitra clip n (%) | 2 (10) |
| Interatrial septal defect n (%) | 1 (5) |
| Bivalve aortic stenosis n (%) | 1 (5) |
| DAVD n (%) | 2 (10) |
| Medication | |
| Statins n (%) | 18 (94) |
| Antiplatelet agents n (%) | 17 (89) |
| Beta blockers n (%) | 12 (63) |
| Direct oral anticoagulants n (%) | 6 (31) |
| Calcium antagonist n (%) | 5 (26) |
| Isosorbide n (%) | 1 (5) |
CRVC: Coronary Revascularization Surgery. DAVD: Arrhythmogenic Right Ventricular Dysplasia. EF: Left Ventricular Ejection Fraction. PCI: Percutaneous Coronary Intervention. TAVR: Transcatheter Aortic Valve Replacement.
Table 2: Ergometric variables after cardiac rehabilitation
| Variable | Initial mean measurement (SD) | Final mean measurement (SD) | Δ Change (%) | p |
| VO2peak (METs) | 5.4 ± 2.33 | 7.4 ± 2.8 | 46.77% | <0> |
| METs-load | 6.68 ± 3.2 | 10.09 ± 2.8 | 84.67% | <0> |
| VE/VCO2 | 35.77 ± 7.8 | 34.1 ± 6.8 | -1.31% | 0.412 |
| VO2/FC | 12.8 ± 4.3 | 15.2 ± 3.1 | 28.36% | 0.005 |
| HRQOL (%) | 69.8 ± 15 | 78.8 ± 13.2 | 15.36% | 0.003 |
SD: Standard Deviation. Δ Change (%): Percentage of change after the intervention. HRQOL: Health-Related Quality of Life. VO2 peak: Peak Oxygen Consumption. VE/VCO2: Ventilatory Efficiency (minute ventilation/carbon dioxide production). VO2/HR: Oxygen Pulse
In terms of CPET variables, a significant gain in VO2 peak was observed after the CR program (initial mean 5.4 ± 2.33 vs final mean 7.4 ± 2.8; p<0.001), with a mean increase of 46.77%. The greatest gain was observed in METs-load, with an increase of 84.67% (initial mean 6.68 ± 3.2 vs final mean 10.09 ± 2.8; p<0.0001), and a similar trend was seen in oxygen pulse, which had a significant increase of 28.36% (initial mean 12.8 ± 4.3 vs final mean 15.2 ± 3.1; p=0.005). Additionally, significant gains in health-related
quality of life were obtained as measured by the SF-36 questionnaire, with a mean increase of 15.36% after the program (initial mean 69.8 ± 15 vs final mean 78.8 ± 13.2; p = 0.003). However, as shown in Table 2, there was no significant decrease observed in the VE/VCO2 slope (initial mean 35.77 ± 7.8 vs final mean 34.1 ± 6.8; p = 0.412).
Table 3: Behavior of ischemic threshold* when present at any moment of CR program, in patients with CE
| Initial ischemicthreshold* | Final ischemicthreshold | Δ Ischemic load METs (%) | Adverse events |
| 1 | Present | Remitted | Remitted | No |
| 2 | Present | Remitted | Remitted | No |
| 3 | No present | New appearance | 100% | No |
| 4 | Present | Present with displacement | 41.9% | No |
| 5 | Present | Remitted | Remitted | No |
| 6 | No present | New appearance | 100% | No |
ΔMETs-load: Change difference of metabolic units established at load estimated by the treadmill protocol, following the formula = ((METs-load at final CPET)–(METs-load at initial CPET))x100/(METs-load at final CPET)
* Ischemic threshold: Presence of ST segment depression at 80 ms from the J point, with a horizontal and descending slope, in at least 3 consecutive beats across two continuous leads; as well as the clinical threshold defined as angina during exercise at incremental load.
Ischemic threshold was found in 6 of the 19 patients (31%), of which it remitted in 3 of them after CR. Additionally, in 2 patients (10%), the ischemic threshold was only present in the CPET performed at discharge, both achieved with a change difference of 100% in METs load. The persistence of the ischemic threshold at discharge was observed in only 1 patient, with a displacement in METs-load percentage of 41.9%. No adverse events were reported. The remaining characteristics are reported in Table 3.
This is the first study to demonstrate the effects of cardiac rehabilitation in various types of heart disease with coronary ectasia. In this study, we observed that this coronary alteration is still more prevalent in men than in women (17), and the most implicated risk factors were obesity, hypertension and smoking. Forty seven percent of the patients presented diabetes mellitus, which is higher than the 36.4% found by Araiza et al (18).
Although our study included all types of heart disease, we observed that the left ventricular ejection fraction (LVEF) was normal in most cases, compared to the study by Vieyra (19), who reported a decrease of 47% in LVEF in patients with acute myocardial infarction and CE. This may be explained by the gains in ventricular remodeling after CR, although it is not entirely possible to elucidate this effect as not all patients had a post-intervention echocardiogram.
We decided to include patients with heart failure because of CR gains in peak VO2, exercise tolerance, and improvement in health-related quality of life, as described in the CROSS-HF meta-analysis (20), ExTraMATCH-II (21), and Taylor's meta-analysis (22). All admitted patients had at least one indication not specifically associated with CE (chronic coronary syndrome, obesity, heart failure, pulmonary hypertension) due to the difficulties in isolating pure coronary ectasia in our population, as they must receive CR as part of comprehensive treatment; however, the most prevalent history was ischemic heart disease (78%). Of our total population, one patient experienced no-reflow phenomenon, and 4 required thrombus aspiration, findings already described in the meta-analysis by Mir et al., which identified higher rates of thrombus aspiration and no-reflow phenomenon compared to patients with myocardial infarction without CE (23).
In the case of ischemic heart disease, cardiac rehabilitation programs via concurrent training have impacted outcomes such as cardiovascular mortality, with a 26% reduction according to the meta-analysis by Anderson and Oldridge in 2016 (24), which also observed an 18% reduction in the risk of hospitalization due to reinfarction, one of the main priorities to address in patients with CE.
Another condition inherent to CE is the complexity of pharmacological treatment. Since there is no consensus on the definitive treatment for this condition, in our center, 89% of patients received dual antiplatelet therapy, and 31% had direct oral anticoagulants. Some patients discontinued nitrates and other pharmacologic strategies during the training program. This is relevant, considering the fact that CR based on an interdisciplinary program with therapeutic exercise is a fundamental tool to propose as a main component of the optimal medical treatment that should be followed by this group of patients.
One of the main findings of this study was the gains in cardiorespiratory fitness, as we documented an increase in peak VO2 (p<0.001) with a percentage change of 46.77% across all patients, primarily associated with the effects of concurrent training: increased arteriovenous oxygen difference, mitochondrial biogenesis, improved ventricular diameters, stroke volume, and cardiac output (25). In Supplementary data, the dispersion of the gains of the ergoespirometric variables are observed, with improvements even greater than the average obtained for the total population, with exception of VE/VCO2.
The improvement in quality-of-life scores measured by the SF-36 questionnaire is like that reported by Belardinelli in 2000, where the same screening tool was used, showing a bidirectional relationship between improved quality of life and increased tolerance for physical activity, particularly through an increase in physical activity scores and a decrease in symptoms (26). In Figure 3, it can be seen how the gains in our population surpass the average after the program.
Regarding the ischemic threshold, we observed the presence of both clinical and electrical thresholds in 6 of the 19 patients (31%), of which it remitted in 50% of them after CR. It is well known that these effects are produced due to adaptations obtained throughout concurrent training: increased angiogenesis, greater production of erythropoiesis cells, increased nitric oxide production, and decreased metalloproteinases and ICAM-1. (27) In two patients, the ischemic threshold was present only after the program and that is explained by the greater tolerance to the load, which is reflected in the significant improvement in quality of life. Only one patient retained the threshold; however, there was a displacement in the treadmill METs-load of 41.9% more exercise tolerance. Larger phase II programs are needed to produce greater gains in this particular outcome. Long-term cohort studies are needed to verify the outcomes of these patients regarding thrombotic re-occlusions or reinfarctions, to elucidate if patients undergoing CR align with other reports, such as that of Amirzadegan et al. (2021), which demonstrated an increased rate of urgent revascularization in CE patients within a year in patients compared to those without the disease. (HR 2.40; 95% CI: 1.13 to 5.86; P = 0.013) (14).
There are some limitations, methodological biases mainly because of the small sample size, along with the absence of a control group with patients without coronary ectasia, prevents determining if there is a difference between the aforementioned populations and patients with CE, as each patient had more than one associated heart disease. Due to the operational nature of our CR center, programs are short duration, despite being concurrent and with quantification in training volume; in other cohorts or experimental studies, phase II CR programs can last up to 6 months, especially assuming that the best effects on coronary circulation occur at long term. Although our program is educational and interdisciplinary, psycho-emotional care sessions and other specific health care areas were provided in group formats. Neverthelss, there were consistent results in patients included in cardiorrespiratory fitness, quality of life and, ischemic threshold, where we found a potential resolution of symptoms that can lead to a better exercise tolerance in daily life.
Cardiac Rehabilitation programs based on concurrent physical training are safe and promote gains in cardiorrespiratory fitness, prognostic ergoespirometric variables, posible remission of ischemic threshold, symptom improvement, and enhancement of quality of life in patients with coronary ectasia associated with other types of heart disease.
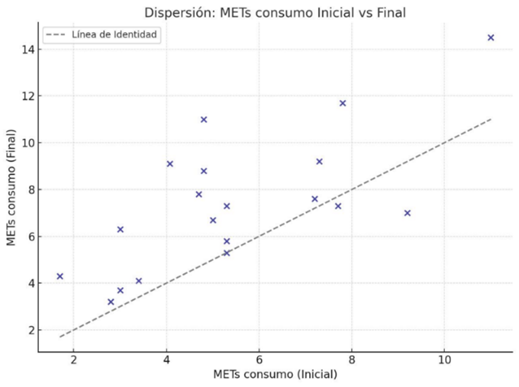
Figure 1: VO2 peak METs at the beginning and at the end of CR
The dispersion of the METs calculated by direct oxygen consumption is presented in a comparative manner between the beginning and the end of the CR program.
Note how the vast majority of the results shows a gain at the end of phase II of the CR program.
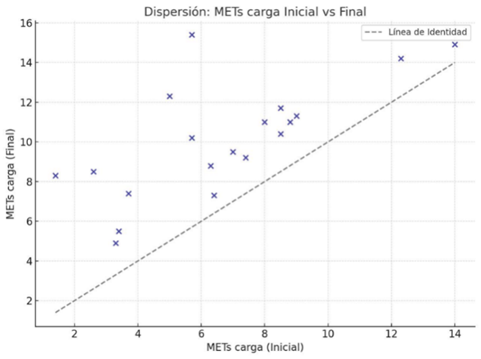
Figure 2: Treadmill METs load at the beginning and at the end of RC
Dispersion of the Treadmill METs load comparing at the beginning and at the end of the CR program. Significant gains above the average for all patients are observed.
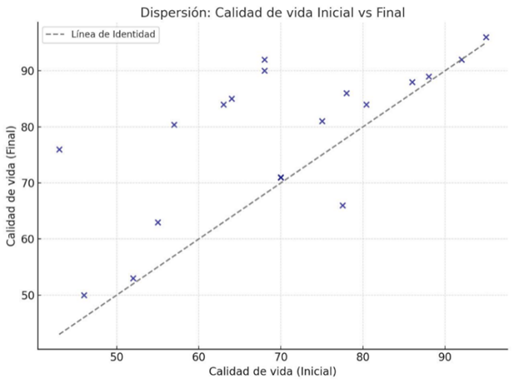
Figure 3: Quality of life at the beginning and end of CR
Dispersion of the health-related quality of life score measured by the SF-36 questionnaire compared at the beginning and at the end of phase II of CR. Significant gains are observed in most patients above the global average.