AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2578-8965/260
1University of Ndjamena, Faculty of Human Health Sciences, Chad.
2University Hospital Center for Mother and Child, Chad.
3Adam Barka University, Abéché, Faculty of Human Health Sciences, Chad.
4China Friendship University Hospital Center, Chad.
*Corresponding Author: Gabkika Bray Madoué, University of Ndjamena, Faculty of Human Health Sciences, University Hospital Center for Mother and Child, Chad.
Citation: Mahamat A. Chene, Gabkika B. Madoué, Némian M, Hawaye Cherif. M, Brahim Deyé, et al, (2025), Epidemiology of Molar Pregnancy in N’djamena Chadian-Chinese Friendship University Hospital, J. Obstetrics Gynecology and Reproductive Sciences, 9(2) DOI:10.31579/2578-8965/260
Copyright: © 2025, Gabkika Bray Madoué. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 14 February 2025 | Accepted: 21 February 2025 | Published: 28 February 2025
Keywords: molar pregnancy; monitoring; prognosis; CHU-ATC; Ndjamena and prognosis
Introduction: Hydatidiform mole or molar pregnancy is a cystic degeneration of the chorionic villi associated with tumor proliferation of the trophoblast. The aim of this study was to describe the epidemiological aspects of hydatidiform mole pregnancy at the Chad-China Friendship Hospital.
Patients and Method: This was a descriptive study with prospective data collection over a period of two (2) years in the gynecology and obstetrics department N’Djamena Chadian Chinese friendship university hospital (NCCFUH). The study population consisted of all patients admitted to the gynecological-obstetric emergency. All patients admitted for a molar pregnancy and consenting patients were included in the study. Data were collected using a pre-established data sheet containing all the variables. Patients were retained and followed throughout the study period. The variables were sociodemographic, clinical, paraclinical and prognostic. Data were entered using Excel and analyzed using SPSS version 26.
Results: The frequency of molar pregnancies was 0.85%. The most common age group was 15 to 20. The mean age was 25.15 years, with extremes of 15 and 40 years. The women were married (97%), housewives (80%), grand multi-gestational women (35%), mostly from urban areas (72%), half of whose spouses were shopkeepers (50%) and whose socio-economic level was average (67%). The reason for consultation was mainly metrorrhagia (57.5%), with a history of miscarriage in 42% of cases and contraception in 73% of cases. Rhesus [O+] and [A+] blood groups accounted for 37.5% and 20% of cases respectively.
Conclusion: Hydatidiform mole is a relatively common condition.
Hydatidiform mole (HM) is defined as partial or total hydropic degeneration of the chorionic villi with more or less marked proliferation of trophoblastic cells. It is characterized by excessive secretion of chorionic gonadotropic hormone, the β-subunit of which is an important diagnostic and post-treatment monitoring method [1]. These moles appear as a result of the abnormal development of trophoblastic tissue. The incidence of GTD is influenced by ethnic origin and risk factors include age, family history, parity, personal history of hydatidiform mole and history of miscarriage [2].
Molar pregnancy is the most common trophoblastic disease. It has an incidence of 1-2/1000 in Europe and Asia [3]. Recent reports from the Republic of Korea and Japan show that the incidence of hydatidiform mole has become as low as in Europe or the United States [4].
In Marrakech University Hospital, the incidence is 4.34% of all pregnancies recorded over five years [5]. It represents a public health problem in developing countries due to its relatively high frequency. The existence of a specific biological marker, gonadotropic chorionic hormone (HCG), in addition to ultrasound imaging and histological examination, makes it possible to diagnose, monitor and establish an effective and appropriate treatment protocol for molar pregnancy [6].
Once the diagnosis of complete or partial mole has been made using the clinical, ultrasound and biological triad, and after assessment of the patient's general and hemodynamic condition using the pre-treatment work-up, uterine evacuation by aspiration is the central stage and the key to treatment of molar pregnancy [7]. This molar pregnancy, which is classed as a gestational trophoblastic disease according to World Health Organization (WHO) criteria dating from 2003, is associated with a clinical presentation, a morphological appearance, genetic data and biological behavior, the combination of which enables optimal diagnosis [8]. This diagnosis must be as accurate as possible, given the psychological consequences for patients faced with terminating a pathological pregnancy or being diagnosed with a tumor, and the various treatment and follow-up options that this entails [8].
In Chad, few studies have been carried out on the monitoring of molar pregnancy, which is why we initiated this work, the aim of which is to study the epidemiological aspects of molar pregnancy.
This was a descriptive study with prospective data collection over a period of 24 months, from 1 January 2022 to 30 December 2024, which took place in the gynecology-obstetrics department of N’Djamena Chadian Chinese friendship university hospital (NCCFUH).. The study population consisted of all patients admitted to the gynecological-obstetric emergency department. All pregnant women admitted for a molar pregnancy were included in the study, as were patients whose diagnosis of molar pregnancy was confirmed by histology and who consented to take part in the study. Data were collected using a pre-established data sheet containing all the variables. The data collection technique was direct interview with the patients and data from the clinical records. We followed the patients during their admission and continued the follow-up after discharge.
Studied variables were socio-demographic, including age, marital status, level of education, occupation, socio-economic level and place of origin. We used Word and EXCEL 2013 software for data entry and analyzed the data using SPSS version 26 software.
During the study period, we recorded 80 cases of molar pregnancy out of a total of 9408 admissions to obstetrics and gynecology, i.e. a frequency of 0.85%.
Age The most common age group was 15 to 20, with a rate of 35%. The average age was 23.5 years +/- 25.15 years, ranging from 15 to 40 years.
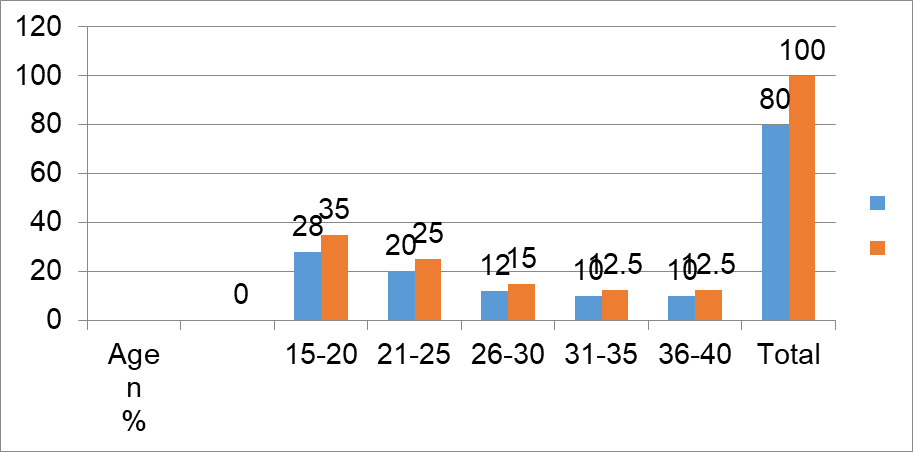
Figure 1: age group
Origin and marital status
72% of patients were from urban areas and 97% were married. Only 3% were divorced.
Profession
| Profession | n | % |
| housewife | 64 | 80 |
| Civil servant | 4 | 5 |
| pupil | 6 | 7.5 |
| Student | 2 | 2.5 |
| Trader | 4 | 5 |
| Total | 80 | 100 |
Table I: profession
The housewife had represented 80%.
Admission mode
Self-referred patients were the most common, accounting for 72% of cases, compared with 28% referred by peripheral care structures.
Reason for admission
| Reason of admission | n | % |
| Metrorrhagia | 46 | 57.5 |
| Pelvic pain | 24 | 30.0 |
| Nausea Vomiting | 2 | 2.5 |
| Ultrasound molar pregnancy | 8 | 10.0 |
| Total | 80 | 100,0 |
Table II: reason of admission
Metrorrhagia was the main reason for admission (57.5%), followed by pelvic pain (30%).
Consultation time
In 62.7%, patients were seen between 3 days and 2 weeks after the beginning of the symptomatology
Husband socioeconomic status
In half the cases, the spouses were shopkeepers (50%). In 67% of cases, the patients had an average socio-economic level.
Socio economic status
| Socio economic status | n | % |
| low | 24 | 30 |
| medium | 54 | 67 ?5 |
| high | 2 | 2.5 |
| Total | 80 | 100 |
The socioeconomic status was medium in 67.5% and low 30%.
History
We noted that the patients with a history of miscarriage represented in 42% and 73% had used contraception method. Grand multiparous were accounted for 51%.
Rhesus [O+] and [A+] blood groups accounted for 37.5% and 20% of cases respectively.
We recorded 80 cases of mole pregnancy out of a total of 9408 pregnancies, i.e. a frequency of 0.85%. This frequency is comparable to that of Mbala in Kinshasa in 2017, which recorded a frequency of 0.13%, i.e. 1 mole for 743 pregnancies [9]. This higher frequency can be explained by the fact that the incidence of pregnancy varies from one region to another and from one era to another. Nevertheless, there is a predominance of mole in developing countries, linked for most authors to nutritional factors and poor socio-economic conditions [10]. For some authors, the nutritional factors that explain the occurrence of a mole pregnancy are linked to a deficiency in vitamin A (which plays an important role in the smooth progress of meiosis) and/or folates (vitamin B9), which are necessary for protein and DNA synthesis [10]. These deleterious factors are thought to come into play at the time of conception [10].
With regard to age, we observed in this study that patients were aged between 15 and 40 years, with a peak between 15 and 20 years, representing a rate of 35%. Our results are comparable to those of Mahaman in Morocco in 2016, who found in his study a peak frequency between 21 and 25 years of age [11]. This result is inferior to that of Guido in Mali on the epidemiological-clinical and prognostic study of molar pregnancy in 2021, who found an average age of 32.4+/-10.6 years, with extremes of 16 and 48 years. The 15-20 and 45-50 age groups were the most represented (18%) [12]. The young age in this series is thought to be related to cultural factors such as marriage among adolescents. Marriage at a young age, and especially early sexuality, opens the way to numerous pathologies.
In terms of socio-economic status, 97% of the patients in this series were married, the majority of them housewives (80%). The spouses were shopkeepers in 50% of cases. Generally speaking, most of our patients had an average socio-economic level (67%). The same observation was made by Sacko in Mali in his study entitled molar pregnancy in 2010 [13] and Mahaman in Morocco in 2016 in his study on the epidemiological, clinical and therapeutic aspects [11], who reported that housewives predominated in 86.6% and 97% of cases respectively. They are housewives in 45.65% of cases, with a low income (less than $2 per day) in 39.13% of cases and with a medium income (between $2 and $25 per day) in 15.21% of cases in a study conducted in MADAGASCAR by JJC Rajaonarison et al in 2015 on the management of hydatidiform moles [14].
Nutritional factors are considered by some authors as factors favoring the onset of trophoblastic diseases. Reduced doses of carotene, vitamin A, proteins and animal fats seem to increase the risk of mole [11].
Generally speaking, a low or average socio-economic level associated with malnutrition increases the risk of mole [11]. These factors could explain the disparity in the frequency of molar pregnancy between developing and industrialized countries.
In terms of parity, multiparous women were the most affected, accounting for 55% of cases in this study. This result is closer to that of AMADOU in Mali, who carried out a clinical, therapeutic and anatomopathological study of molar pregnancy in 2023, which found a frequency of multiparity in 62% of cases [15], and higher than that of Mahamane [11], who noted 45% of multiparous
The increased risk of molar pregnancy is almost constantly reported and is explained by maternal age and the history of multiparous women [16].
Previous spontaneous abortion: According to the literature, the risk is multiplied by 2 to 3. In a study conducted by JOHANA et al in 2022, the risk for the two histopathology subgroups (MHC and MHP) was higher in women reporting spontaneous miscarriages [17]. Compared with women who had never miscarried, the estimated ratios (as relative risk estimators) were 3.1 and 1.9, respectively, for complete mole and partial mole for two or more miscarriages [17]. In our study we found 58% of cases with a history of miscarriage, compared with Mahaman MM in Mai in 2016 who reported 24% of abortions and 1% of molar pregnancies [11]. And Sacko in Mali in 2010 reported a history of abortion in 26.9% of cases [13].
All authors agree the submission of this paper