AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2690-8808/251
1 Unit of Thoracic Surgery, Azienda USL di Reggio Emilia – IRCCS.
2 Unit of Thoracic Surgery, Azienda Policlinico-Universitaria di Modena.
*Corresponding Author: Cristian Rapicetta, Unit of Thoracic Surgery, Azienda USL di Reggio Emilia – IRCCS.
Citation: Cristian Rapicetta, Alessandro Marchioni, Tommaso Ricchetti, Alberto Matricardi, Elena Carrese, et al, (2025), Endobronchial Valve as Salvage Lung-Sparing Treatment of Prolonged Air Leak Following Laser Assisted Metastasectomy, J, Clinical Case Reports and Studies, 6(4); DOI:10.31579/2690-8808/251
Copyright: ©, 2025, Cristian Rapicetta. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 20 March 2025 | Accepted: 07 April 2025 | Published: 22 April 2025
Keywords: metastasectomy; emphysematous lung; lung LASER; endobronchial one-way valves (EBV)
In the recent years employment of LASER for resection of lung metastasis demonstrated to be a valid surgical option to avoid major anatomical lung resections.
First experimental studies performed in the swine model [1] showed that at histological evaluation in the 0.5-cm quadrants laying distant from the “center” of the LASER application, the tissue presented with cell vacuolization and membrane destruction, while not signs of thermal damage was observed at 1-cm quadrants.
These data have several implications for daily clinical application; firstly, lung areas that are distant more than 1 cm apart do not entail the risk of heat accumulation; secondly, while resecting lung metastases that are closer than 1 cm to each other, the surgeon should either wait 3 to 5 minutes for spontaneous tissue cooling before resecting the next metastasis to avoid applying the second LASER shot on a surface of pulmonary parenchyma already interested and potentially damaged by the first application; finally, the microscopic (not detectable) residual neoplastic cells (spreading from the metastatic lesion to the adjacent “healthy” parenchyma) could potentially be eradicated until 1 cm far from resected area.
Therefore, LASER resection are considered radical even when a closer margin of resection (< 1 mm) is found at histological examination of specimen. Moreover, through the high temperature reached in the tissue (>700°C), LASER has an excellent sealing ability of small vessels and bronchi until 3-4 mm, minimizing the risk of intraoperative and postoperative bleeding and air leakage.
Conversely, when such complications occur, especially delayed air leakage from bronchopleural fistula (BPF), treatments may be very challenging since scar tissue could prevent healing. Therefore, surgical intervention, pleurodesis, and prolonged chest tube drainage have several disadvantages in these patients. Many attempts have been made to treat BPF through flexible bronchoscopy by submucosal injection of acrilic glue.
Endobronchial one-way valves (EBV), originally designed for lung volume reduction in pulmonary emphysema, represent an emerging option for treatment of BPF. Insertion of EBV have less trauma, relatively short operation time, better safety than surgical intervention and is more likely to be accepted by patients.
In this paper we describe two case of delayed and prolonged air leak after LASER resection which finally received a successful treatment through placement of endobronchial valves.
A 55-yrs old patient with long history of IV stage thyroid cancer was scheduled for redo-metastesectomy of right lung after careful functional and oncological evaluation. A right lower lobectomy for large recurrent hilar metastasis and LASER assisted resection of a paramediastinal metastasis of right upper lobe and other two lesion of middle lobe was performed. Laser device used was Neodimium (Nd:YAG) 1,318 nm (LIMAX-120, Gebrüder Martin GmbH & Co. KG, Tuttlingen, Germany) equipped with innovative characteristics (power up to 120 W; cut-line temperature up to 700°C). Postoperative course was uneventful until 5th day, when air leak and pneumothorax was observed (Figure.1). Due to increasing amount of air leakage and complete residual lung collapse (Figure.2), surgical repair was tempted. Intraoperatively BPF was found in right upper lobe. Direct suture, fibrin glue and pleural drape failed to stop air leak. Lung collapse prevented also blood patch. Therefore EBV were inserted first in upper segmental bronchus of right upper lobe (Figure.3) and, in a second-stage procedure, in middle lobe. Air leak stopped within 5 days, allowing to remove pleural drainages after 15 days. Despite the amount of lung parenchyma resected and the number of EBV inserted no significant residual pleural space was observed at follow-up (Figure.4).
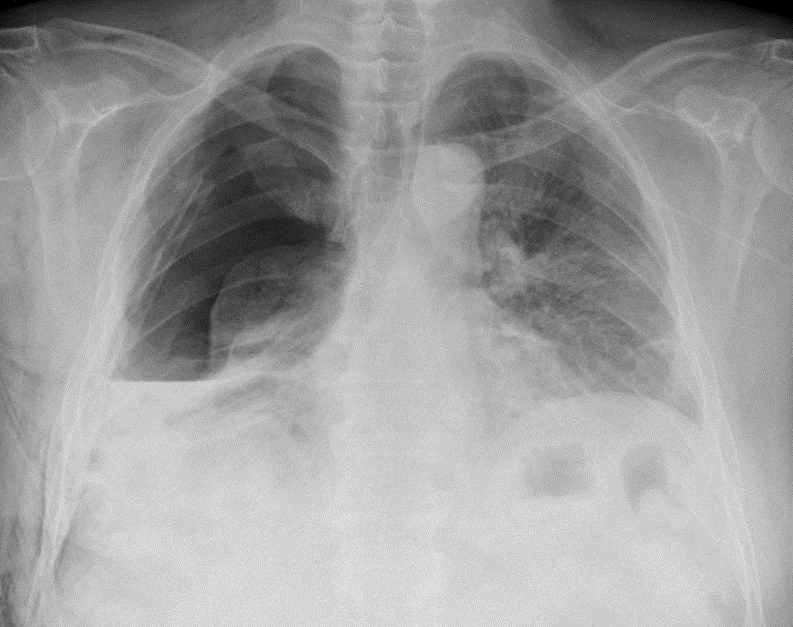
Figure 1: large hydro-pneumotorax despite large-bore chest tube and suction

Figure 2: CT-scan showing large pneumothorax, pleural thickening and small BPF of RUL communicating with residual pleural space
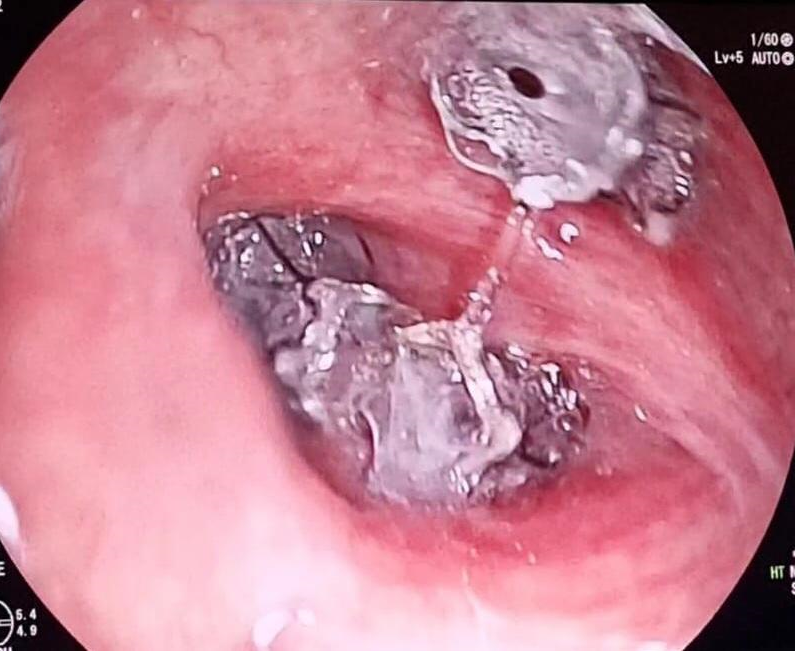
Figure 3: complete RUL exclusion with EBV placed in each of 3 segmental bronchi
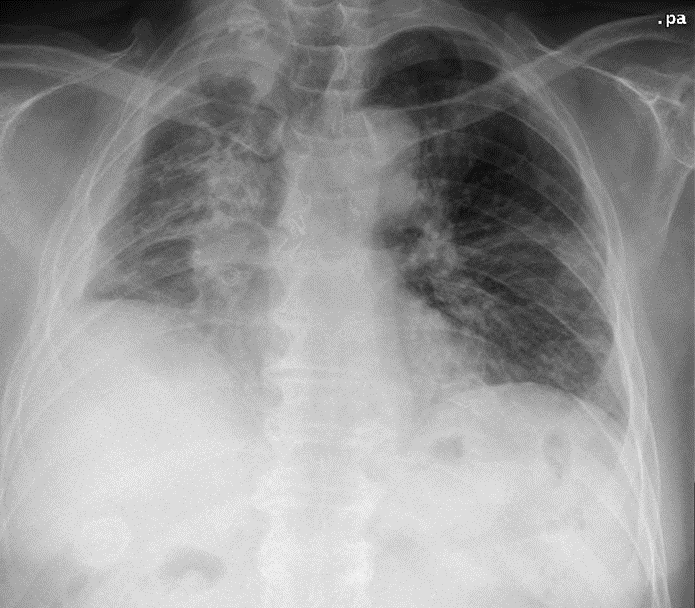
Figure 4: long-term result at 12 months follow-up (after 12 months?)
A 54-yrs old patient with medical history of previously resected bladder urothelial tumour underwent LASER assisted resection of 1.3 cm nodular lesion in right lower lobe. Resection was performed by LASER Limax 120. Postoperative course was uneventful with discharge on 5th postoperative day. At 6 months follow-up chest CT-scan moderate right pneumothorax was observed necessitating chest-tube insertion. A small area of subpleural cavitation with thickened walls in the area of previous LASER resection was observed at chest CT scan (Figure.5). After 6 days, with apparently no air leakage, chest-tube was removed but the patients experienced early recurrent pneumothorax at 1-week chest X-rays. Considering the radiological findings, the timing and the kind of air leak, EBV placement was considered as the first option. EBV was inserted in segmental apical bronchus of right lower lobe (Figure. 6), leading to cessation of air leak and chest tube removal within 1 week. No recurrences and no significant pulmonary atelectasis were reported (Figure. 7).
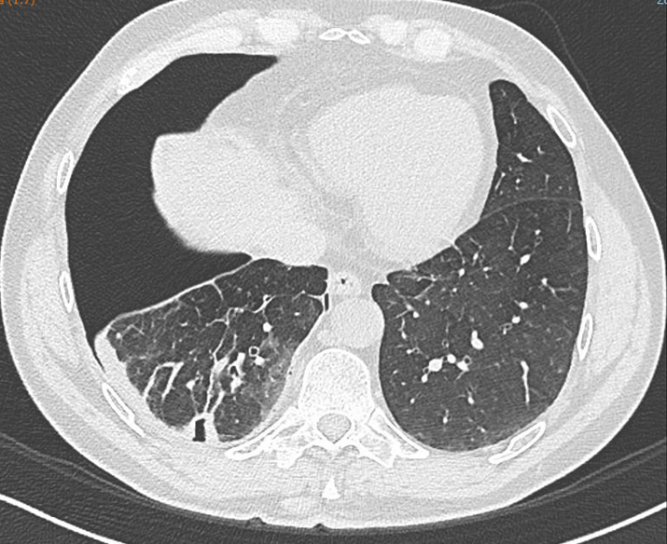
Figure 5: Chest CT-scan demonstrating (demonstrates) right pneumothorax with pleural thickening and dense scar tissue surrounding pulmonary breach in the area of resected metastasis

Figure 6: EBV placed in two segmental bronchi of basal pyramid of RLL
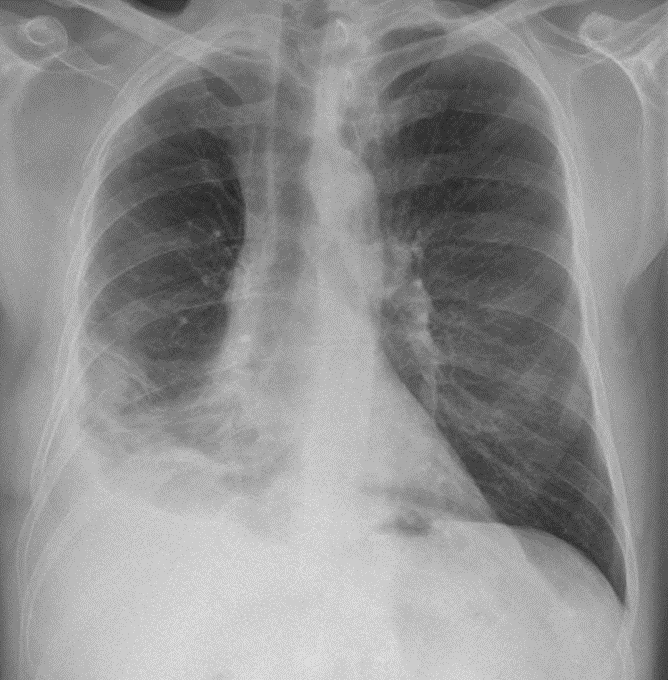
Figure 7: 6 months result prior to EBV removal
Air leak is the most common postoperative complication after lung surgery and it is defined prolonged (PAL) when persisting 5 or more days after intervention. The incidence varies from 10% (Society of Thoracic Surgeons (STS) General Thoracic Surgery Database (GTSD)) to 25% in other reports [2,3]. PAL significantly affects postoperative outcome (pain, ateletactasis, pneumonia, venous thromboembolism), increases in-hospital lenght of stay and consenquently costs by an average 30% [4,5,6,7]. Moreover, PAL also is associated with increased in-hospital mortality, with 3.4 times greater risk of death than those without (95% confidence interval [CI], 1.9–6.2) [4].
Air leak originates from an alveolar-pleural fistula or a broncho-pleural fistula (BPF): the first is defined as a communication between the alveoli of the pulmonary parenchyma distal to a segmental bronchus with the pleural space, conversely, broncho-pleural fistula is when the communication exists between main stem, lobar of sublobar bronchus [8]. BPF is less common than alveolar-pleural fistula, with an incidence less or equal to 1
EBV represents a valid and safe therapeutic option in complex APF or BPF when some factors (scar tissue surrounding air leak site, residual pleural space, previous extended lung resection, pleural thickening and pulmonary coartaction) may prevent success of surgical (re)intervention or in patients unfit for surgery. Infectious diseases, atelectasis, respiratory failure and migration are not frequent complications [16].