AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2768-2757/163
Department of General Surgery, Graphic Era Institute of Medical Sciences, Dehradun.
*Corresponding Author: J.A. Jayalal., Department of General Surgery, Graphic Era Institute of Medical Sciences, Dehradun.
Citation: J.A. Jayalal, Ajeet Shukla, (2025), Diagnostic Value of Systemic Immune Inflammation Index in Acute Appendicitis: A Prospective Study in A Tertiary Care Teaching Institute, Journal of Clinical Surgery and Research, 6(2); DOI:10.31579/2768-2757/163
Copyright: © 2025, J.A. Jayalal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 06 March 2025 | Accepted: 19 March 2025 | Published: 03 March 2025
Keywords: acute appendicitis; systemic immune inflammation index; alvarado score
Background: Acute appendicitis is a common surgical emergency requiring prompt diagnosis and treatment to prevent complications. The Systemic Immune Inflammation Index (SII) has emerged as a potential diagnostic tool to assess inflammation and stratify cases based on severity.
Objective: This prospective study aimed to evaluate the diagnostic value of SII in differentiating complicated and non-complicated acute appendicitis cases in a tertiary care teaching institute.
Methods: The study included a total of 120 patients diagnosed with acute appendicitis. Based on clinical and surgical findings, we subdivided the cohort into complicated (n = 11) and non-complicated (n = 109) cases. We analyzed parameters such as the Alvarado score, Appendicitis Severity Score (AAS), and peritonitis findings alongside SII values.
Results: Mean Alvarado score (14.5±2.83 vs. 11.40±1.98; p<0.001) and AAS (7.33±1.08 vs. 4.33±1.38; p<0.001) were significantly higher in complicated cases compared to non-complicated ones. Peritonitis findings were also more pronounced in complicated appendicitis (p=0.003). SII demonstrated significant diagnostic utility in differentiating the two groups, with higher values correlating with complicated appendicitis.We also found a link between higher SII values and adverse surgical outcomes. This suggests that SII could help with figuring out which patients with acute appendicitis are at highest risk and making decisions about how to treat them
Conclusion: SIII is a valuable and accessible biomarker for diagnosing acute appendicitis and identifying complicated cases. Its integration with established clinical scoring systems such as the Alvarado score and AAS enhances diagnostic accuracy and supports timely intervention. Further studies are warranted to validate its use in routine clinical practice.
Acute appendicitis (AA) is one of the most common abdominal emergencies worldwide. [1]. The timely diagnosis and management of AA are crucial to prevent complications such as perforation and peritonitis. Understanding the pathophysiology and utilizing effective biomarkers like the SIII can significantly improve patient outcomes, highlighting the need for ongoing research in this area.
Lifetime risk is 8.6% in men and 6.7% in women [2]. This variation in risk underscores the importance of gender-specific considerations in both diagnosis and treatment approaches. Moreover, early recognition of symptoms and prompt surgical intervention remain essential components in reducing morbidity associated with acute appendicitis. [3].
In addition, AA is one of the most common causes of hospitalization in patients admitted to the emergency department with abdominal pain. Clinical diagnosis of AA is often difficult and involves a synthesis of clinical, laboratory, and radiological findings. Finding the right balance in these diagnostic methods is crucial, as misdiagnosis can lead to unnecessary surgeries or delayed treatment. Therefore, ongoing research into more accurate diagnostic tools and strategies tailored to different demographics is vital for improving patient outcomes.
Physical examination findings and inflammation markers can improve the accuracy and reliability of the diagnosis of AA. It is also possible to assess the risk of AA using a variety of scoring systems, including the Alvarado score, RIPASA score, the acute appendicitis score, the adult appendicitis score (AAS), the appendicitis inflammatory response (AIR), and a modified Alvarado score. These scoring systems have been shown to be useful in diagnosing and treating AA. [4,5].
The systemic immune inflammation index (SIII) is a novel systemic inflammatory prognostic indicator associated with outcomes in patients with different tumors.
Studies have shown an association between SIII and many chronic/acute inflammatory diseases [6]. The integration of SIII into routine diagnostic protocols could enhance early detection and allow for more personalized treatment plans. Additionally, further exploration of SIII's role across various populations will be essential to ensure that all patients benefit from advancements in diagnostic accuracy.
SIII is simple to calculate, inexpensive, requires only a complete blood count, and relies on no subjective findings. This will yield more accurate results in diagnosing AA.
This study was a prospective cohort study conducted in the surgical ward of the Government Medical College Hospital, Kanyakumari, from September to November 2024.
The study included a total of 120 patients diagnosed with acute appendicitis who were undergoing appendectomy. Data were collected on various factors, including demographics, clinical presentation, medical history, WBC, platelet count, neutrophil count, SIII values, Alvarado scores, pathological results and postoperative outcomes, to assess the effectiveness of surgical interventions and contribute to improved patient management strategies.
Based on clinical and surgical findings, we subdivided the cohort into complicated (n = 11) and non-complicated (n = 109) cases. The analysis revealed significant differences in postoperative recovery and complication rates between the two groups. Notably, patients with complicated appendicitis exhibited longer hospital stays and a higher incidence of surgical site infections, underscoring the need for tailored management approaches in these cases.
We analyzed parameters such as the Alvarado score, Appendicitis Severity Score (AAS), and peritonitis findings alongside SII values. These metrics provided valuable insights into the correlation between initial assessments and postoperative outcomes. Furthermore, the use of predictive models based on these parameters could enhance preoperative decision-making and ultimately improve patient care.
We calculate Alvarado ratings using diagnostic results from laboratory tests (leukocytosis and left shift), signs (tenderness, rebound tenderness, and increased body temperature), and symptoms (migratory pain, anorexia, nausea, and/or vomiting). We assigned one point to each signal, except for leukocytosis and discomfort, resulting in a total score of 10.
The systemic immune inflammation index (SIII) is a novel systemic inflammatory prognostic indicator associated with outcomes in patients with different tumors.SIII, calculated as [(P×N)/L)], was used to assess the overall immune response. These ratios and counts provide valuable insights into the patient's hematological status and can help guide clinical decisions regarding potential infections or inflammatory conditions.
Mortality evaluation was based on the mortality rates of the patients during hospital stay. We used the ROC curves to determine a cutoff point for sensitivity and specificity calculations.
A total of 120 patients were included in the study. Mean age was 33.47±11.01 years Mean pulse rate was significantly higher and there was no significant difference between other vital parameters. WBC and neutrophil count were significantly higher, and lymphocyte level was significantly here was no significant changes in platelet count
| Parameter | Subparameter | Patient group |
| Age | 33.47±11.01 | |
| Gender | Female | 58 (48.5) |
| Male | 62 (51.2) | |
| Vital parameters | Systolic BP (mmHg) | 126.65±26.47 |
| Diastolic BP (mmHg) | 78.50±16.57 | |
| Pulse (pulse/min) | 94.03±19.71 | |
Table 1: The demographic values.
The laboratory values were calculated and in comparison, with the normal range, the statistically significant calculated. Using the value, the ratios were calculated and tabulated in Table 2.
| PATIENTS | NORMAL | P Value | ||
| Laboratory values | WBC (×109/L) | 13.42±4.57 | 8.72±2.89 | <0> |
| Neutrophil (×109/L) | 7.75±5.41 | 4.10±4.84 | <0> | |
| Lymphocytes (×109/L) | 1.75±0.75 | 2.07±1.04 | 0.004 ** | |
| Platelet (×109/L) | 238.06±68.98 | 254.89±66.18 | 0.032** | |
| Ratios | NLR | 7.72±5.41 | 4.10±4.84 | <0> |
| PLR | 161.27±90.03 | 156.88±113.04 | 0.648** | |
| PNR | 26.13±16.18 | 51.78±24.04 | <0> | |
| LNR | 0.22±0.17 | 0.43±0.265 | <0> | |
| SIII (×109/L) | 1759.62±1263.92 | 979.96±1032.33 | <0> |
Table 2: Laboratories values.
Based on the complication status, we further subdivided the patient group into complicated and non-complicated cases. We evaluated 11 cases of complicated appendicitis and 109 cases of non-complicated appendicitis.
The frequency of both defense findings and rebound findings in the physical examination was significantly higher in complicated appendicitis cases.
WBC and neutrophil counts were significantly higher, and lymphocyte count was significantly lower in complicated appendicitis cases compared with non-complicated cases. These findings suggest that laboratory and clinical evaluations can play a crucial role in differentiating between complicated and non-complicated appendicitis. Consequently, this differentiation may guide more effective treatment strategies and improve patient outcomes.
The patient group was further subdivided as complicated and non-complicated cases based on the complication status. In all, 18 cases were evaluated as complicated appendicitis cases and 132 cases as non-complicated appendicitis cases. Both defense and rebound findings in physical examination were significantly more common in complicated appendicitis cases. WBC and neutrophil count were significantly higher and lymphocyte count was significantly lower in complicated appendicitis cases compared with non-complicated cases. SIII, NLR, and PLR were significantly higher and PNR and LNR were significantly lower in complicated appendicitis cases.
Mean Alvarado score (14.5±2.83 and 11.40±1.98; p<0 p=0.003).>
| Mean Alvarado SCORE | Appendicitis severity score | P value | |
| Complicated (n=11) | 14.6±2.88 | 7.32±1.08 | p<0> |
| Uncomplicated (n=109) | 11.44±1.96 | 4.31±1.39 | p<0> |
Table 3: Complicated vs uncomplicated Appendicitis.
With a cutoff value of 860.23, the ROC analysis showed that SIII had a sensitivity of 82 and a specificity of 68.7% for the diagnosis of AA. Table 4 and Figure 1 also show that a cutoff value of 1792.94 for SIII was able to tell the difference between complicated and non-complicated cases 69.9% of the time and 88.9% of the time. This indicates that SIII could serve as a valuable biomarker in clinical settings, assisting healthcare professionals in distinguishing between the two types of cases. We need to conduct further research to confirm these findings and investigate the possibility of incorporating SIII into standard diagnostic procedures.
| Parameter | Cutoff value | Sensitivity | Specificity | Area under curve (AUC) | 95%CI | |
| Diagnostic value of SIII | 860.23 | 82.0 | 68.7 | 0.764 | 0.709 | |
| SIII for differentiating between complicated vs. non-complicated cases | 1792.94 | 88.9 | 69.9 | 0.826 | 0.744 | |
Table 4: Systemic immune inflammation index receiver operating characteristic analysis results for the diagnosis of acute appendicitis and identifying complications.
ROC: receiver operating characteristic; SIII: systemic immune inflammatory index. Bold indicates statistically significant p-values.
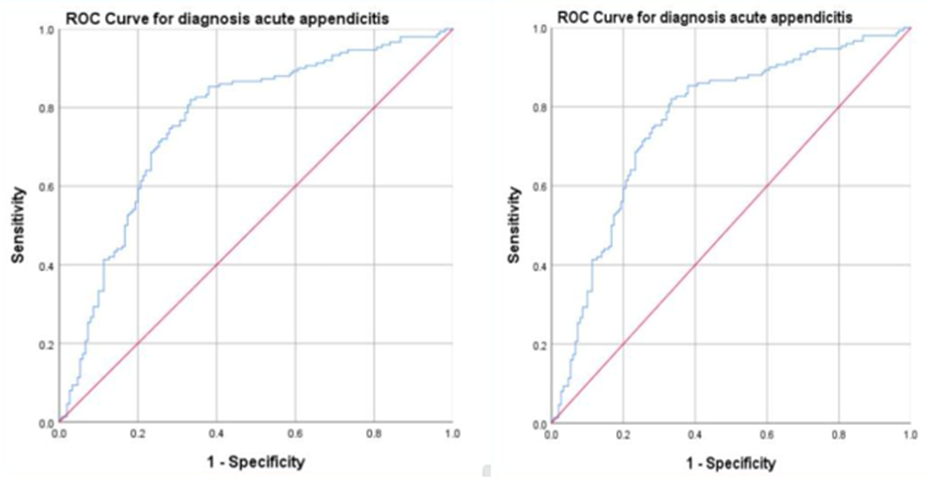
Figure 1: illustrates the systemic immune inflammation index receiver operating characteristic analysis for diagnosing acute appendicitis and identifying associated complications.
Acute appendicitis is one of the leading abdominal emergencies worldwide. It often requires prompt surgical intervention to prevent complications such as perforation or abscess formation. Early diagnosis and treatment are crucial for reducing morbidity and ensuring positive patient outcomes.
In emergency room settings, the diagnosis of AA remains unclear due to tests that prolong the process, are not cost-ineffective, and expose patients to radiation.
Researchers are actively searching for new diagnostic tools to enhance the accuracy, reliability, and cost-effectiveness of the diagnosis of AA. A study by Jayalal JA et al. found that the Appendicitis Inflammatory Score (AIR) and the Alvarado score are effective ways to diagnose appendicitis and give results that are similar to CT or post-op pathological results. [7,8].
Recent studies show that SIII is both an accurate indicator of inflammation and a useful ratio that helps predict the diagnosis and prognosis of many diseases. SIII is a newly designed, simple, and inexpensive index that reflects the balance between inflammatory and immune responses. [9].
The study's results revealed that SIII is a reliable index that can distinguish between complicated and non-complicated AA cases. Leukocyte count is one of the most used diagnostic methods in the diagnosis of AA. However, the leukocyte count has limited sensitivity and specificity.
In our study, the patient group with AA had a higher leukocyte count. Similarly, many diseases use NLR and PLR as auxiliary parameters for diagnosis and prognosis.
In this study, patients with AA had significantly higher NLR, but there was no significant difference in PLR. Furthermore, this study's results suggest that PNR and LNR are useful diagnostic ratios for AA diagnosis.
In contrast to Khairol et al. [10]. this study found higher SIII sensitivity than NLR and the same specificity. Dey et al. [11]. examined AA cases with histopathological diagnoses and discovered misdiagnoses. For this reason, they investigated the correlation between histopathological diagnosis and Alvarado score and found a statistically significant positive correlation.
Canbak et al. [12]. investigated the correlation between Alvarado scores and ultrasonography in the diagnosis of acute appendicitis. They found that their combined use reduced the rates of misdiagnosis and missed diagnosis.
Sousa-Rodrigues et al. [13]. discovered a correlation between the Alvarado score and the macroscopic appearance of the appendix in another study. Only in the advanced stage of AA did they observe this correlation.
Similar to the diagnosis, it is crucial to categorize cases as complicated or noncomplicated beforehand in order to plan the treatment strategy. This is because in complicated cases, not only are the challenges associated with inflamed appendicitis more severe, but the incidence of SSIs is also significantly higher.
Ener K, et al. [14], have reported on the diagnostic power of SIII for AA, specifically its ability to distinguish between complicated and non-complicated AA. In their study, the cutoff value of 860.13 (×109/L) for SIII had 82% sensitivity and 68.7% specificity. And the cutoff value of 1,792.94 (×109/L) had 88.9% sensitivity and 69.9% specificity for differentiating between complicated and non-complicated cases. According to Khairol et al., the sensitivity of SIII surpasses that of NLR, while its specificity remains the same. Our study also shows a correlation with the previously published study by Ener K et al.
The study's results suggest that SIII can aid in the diagnosis of AA and lessen the need for radiation-exposed diagnostic imaging tests like contrast-enhanced abdominal computed tomography. SIII is cost-effective and simple to calculate, and its use with the Alvarado score and AAS will reduce both misdiagnosis and unnecessary operation rates. By integrating SIII with existing diagnostic tools, healthcare providers can enhance patient outcomes while minimizing costs and risks associated with radiation exposure. This innovative approach not only streamlines the diagnostic process but also promotes a more personalized treatment strategy for patients presenting with acute appendicitis.
Self
Nill