AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/2639-4162/227
1 Department of Surgery, Surgery Service II, Faculty of Medicine, Central University of Venezuela, University Hospital of Caracas, Caracas, Venezuela
2 Luis Razetti School, Faculty of Medicine, Central University of Venezuela, Caracas, Venezuela.
*Corresponding Author: Argelis Sofia Linares, Department of Surgery, Surgery Service II, Faculty of Medicine, Central University of Venezuela, University Hospital of Caracas, Venezuela.
Citation: Miguel V. Palermo, Argelis S. Linares, Hermógenes Malavé, Daniela Nieto, José L. M. Pompili, (2024), Conn Syndrome Origins. About A Case, J. General Medicine and Clinical Practice, 7(19); DOI:10.31579/2639-4162/227
Copyright: © 2024, Argelis Sofia Linares. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 23 September 2024 | Accepted: 13 November 2024 | Published: 20 November 2024
Keywords: primary hyperaldosteronism and surgery; conn syndrome; aldosterone; case report; hypersecretory adenoma
Background: Jerome W. Conn, was a medical researcher known for his recognition of a disorder he termed "primary aldosteronism" caused by an aldosterone-hypersecreting adrenal tumor, one of the few severe hypertensive diseases that can be completely cured by surgical removal of the adrenal tumor. We present a female patient with primary hyperaldosteronism, who underwent laparoscopic adrenalectomy and found a hypersecretory adenoma.
Objectives: Describe primary aldosteronism through a historical account of the life of Jerome W. Conn. Methods: Through a retrospective, multicenter study.
Results: a systematic search was carried out in MEDLINE, Cochrane, PubMed, Google Scholar, from 1936 to 2023, obtaining 2681 results, of which 114 studies were included.
Conclusion: The historical perspective and learning the lessons of the past are essential for medical practice, it is because we all have the need to find heroes like Jerome Conn who inspire us to support the fight against the disease. A clinical case was presented, whose initial clinical suspicion was based on a female patient with arterial hypertension and refractory hypokalemia, after surgical removal a complete cure of arterial hypertension and hypokalemia was obtained. Conn syndrome is a commonly overlooked disease; timely diagnosis is important to reduce the risk of cardiovascular complications in affected patients.

Figure 1. Jerome W. Conn, freehand drawing made by one of the authors.
Was a research physician who was born in Manhattan and graduated from Rutgers University in 1928. He received his MD from the University of Michigan in 1932, where he remained for virtually his entire career. He headed the Division of Endocrinology and Metabolism from 1943 to 1973. He became Distinguished Professor of LH Newburgh University in 1968 and retired in 1973 [1]. For starters, he is credited with recognizing a disorder called potassium-wasting nephritis, a serious kidney disease that had long baffled endocrinologists. Dr. Conn, then at the University of Michigan Medical School in Ann Arbor, found the hormonal disorder causing the disease in 1953. He called it "primary aldosteronism," now also known as Conn syndrome, caused by an adrenal gland tumor that secretes excessive amounts of the hormone aldosterone [1, 2]. Regarding its prevalence, it is unknown in the general population; in referred hypertensive populations it is estimated between 6 and 13%, of which 1.5 to 5% present unilateral primary adrenal hyperplasia. Taking referral biases into account, the prevalence of surgically correctable primary aldosteronism is probably less than 1.5% in the hypertensive population and less than 0.3% in the general adult population [2]. Therefore, a clinical case of a female patient is presented, whose initial clinical suspicion was given by findings such as HTN and refractory hypokalemia, diagnosed by laboratories as aldosterone in blood and contrast-enhanced tomography concluding as primary hyperaldosteronism.
A 39-year-old female patient with a history of obesity since childhood, high blood pressure for 10 years in the context of headache associated with hypertensive crisis, reports onset of current illness 10 months ago characterized by repeated episodes of syncope, at which time an echocardiogram where signs of eccentric ventricular hypertrophy are observed and electrocardiogram that reported complex ventricular tachycardia, in view of exacerbating clinical signs due to syncope associated with palpitations, diaphoresis, tonic-clonic seizure with ocular retroversion, plus evidence in the electrocardiographic trace of pulseless polymorphic helical ventricular tachycardia who responds to defibrillation and placement of a temporary pacemaker, was admitted to the cardiology unit of the University Hospital of Caracas. After this event, the patient presented with paraclinical potassium levels at 2.2 mEq/L, correction of potassium figures and removal of the pacemaker began, thus showing that despite the restoration of potassium it remained at figures 2.70 and 2.8 sustained, with a partial response to treatment. Imaging studies are requested, contrast-enhanced tomography of the abdomen and pelvis where an image of nodular appearance is observed in the left adrenal gland, with defined edges, hypodense in the soft tissue range (20 HU), which enhances with the administration of contrast (70 HU). It measures 20 x 15 mm in diameter, (Figure. 2).
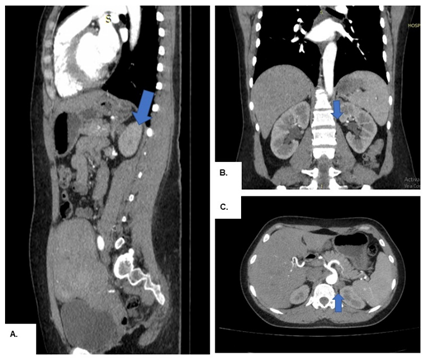
Figure 2. Contrast-enhanced tomography of the abdomen and pelvis showing (blue arrow) a nodular lesion in the upper pole of the left kidney, in its different projections: A. Sagittal. B. Coronal. C. Axial.
Laboratory studies were carried out that reported: Aldosterone 47 ng/Dl, rest of paraclinicals within normal limits. On physical examination, the patient was in fair general condition, BP 130/80 MMHG HR: 55 BPM RR 16 RPM BMI 27.91 KG/M2, symmetrical chest, apex not visible, palpable in the 5th intercostal space of a sustained nature, noises Normophonetic rhythmic cardiac sounds, no murmurs heard, abdominal evaluation within normal limits.
Treatment
Patient is prepared for surgery and taken to the operating table, where laparoscopic left transabdominal adrenalectomy is performed (Fig. 3),
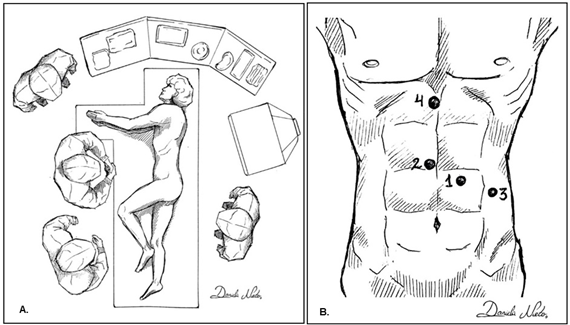
Figure 3: Laparoscopic Transabdominal Adrenalectomy, lateral approach performed on the patient. A. Location of the patient and the surgical team B. Arrangement of the trocars. Freehand drawing made by one of the authors.
which revealed: a Left adrenal gland measuring 8 x 6 cm with adenoma in the superficial cortex measuring 3x2 cm (Figure. 4A).
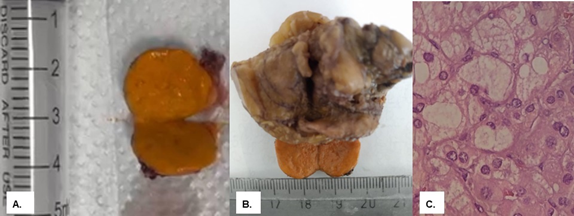
Figure 4: A. Hypersecretory adenoma after enucleation in surgical resection B. Macroscopic piece of left adrenal gland with adenoma in the upper pole.
C. Microscopic view of neoplastic lesion, histologically benign.
Sample is sent to pathological anatomy, concluded: Non-neoplastic adrenal gland of usual configuration, mature adipose tissue, small remnants of adenomatous lesion, nodular structure, benign neoplastic lesion, basically constituted by two types of cell populations: one with basophilic cytoplasm cells plus or less homogeneous suggestive of Aldosteronoma (Fig. 4B-C).
With a satisfactory clinical evolution, the patient was discharged 24 hours postoperatively. Strict controls of blood pressure figures are maintained where a favorable response is observed, achieving figures of 120/80mmHg without antihypertensive treatment one year after surgery.
A retrospective, multicenter study was carried out through a systematic search in MEDLINE, Embase, Cochrane, Pubmed and Google Scholar, both Spanish and English, from 1992 to 2023, using the following search terms “Conn, Jerome syndrome W. Conn, Primary Hyperaldostenorism and Surgery, case reports”, limiting the search to published articles, obtaining 2681 results. Inclusion criteria: Studies in English and Spanish that described historical aspects about Jerome W. Conn and clinical case reports with diagnoses of primary hyperaldostenorism with indication and cure through surgical removal of adrenal adenoma were included. Exclusion criteria: Studies that did not describe historical aspects about Jerome W. Conn were excluded. Studies and case reports that did not incorporate surgical excision or surgery as the first-line treatment were also excluded.
2681 studies were identified, of which, after reviewing the title, abstract and keywords, 2567 did not meet the inclusion criteria or met the exclusion criteria. Of the 114 included studies, 32 conducted a literature review regarding historical aspects and 82 case reports.
Conn graduated from the University of Michigan Medical School in 1932 with honors and as a member of the Alpha Omega Honor Society. He first did an internship in surgery, but after a year he moved on to internal medicine. His wife joined the division at the same time and they collaborated on important studies on the relationship between obesity and non-insulin-dependent diabetes. Conn joined the division as a member in 1935 and became assistant professor of internal medicine in 1938 (3).
During his highly productive career at Michigan, Conn authored 284 scientific articles and book chapters; but the most impressive product of his long leadership of the Michigan Division of Endocrinology and Metabolism Research Unit was the large number of bright young people who began their research careers in his division. He tirelessly supported their development as independent researchers and fostered their research careers. Conn received many honors and was a member of twelve national professional societies [1, 4]. Conn's group was one of the first to clearly recognize the relationship between obesity and adult-onset diabetes. They did this by showing the resumption of normal carbohydrate tolerance after achieving normal weight in twenty of twenty-one patients. This was quite an achievement in view of the difficulty of obese patients in achieving a normal weight through dietary restrictions [5, 6].
During World War II, in 1943, Conn took charge of the Division of Endocrinology and Metabolism. Because acclimatization to tropical heat was a major military concern in the South Pacific, he undertook a series of investigations into the regulation of sweat salt loss in conscientious objectors exposed to elevated heat and humidity. Conn established that acclimatization involved a rapid reduction in renal, sweat, and salivary excretion of sodium [7]. The Department of the Army had provided funding to Conn and the University of Michigan to study the effect of the Pacific theater environment on soldiers' physical adaptation. Conn conducted balance studies in normal subjects living in a warm, humid laboratory environment for long periods in an attempt to define the nature of the body's adaptation to heat stress. This adaptation appeared to involve sodium conservation through a yet-to-be-discovered salt retention factor. Conn stated in 1949 that “in chronic stress of the type employed in these experiments, the evidence for a continuous increase in the activity of salt-retaining steroids is clear” (8). In 1950, he said that “changes in the sodium and chloride concentration of thermal sweat collected under standard conditions parallel changes in the activity of the adrenal cortex with respect to the production of steroids acting as deoxycorticosterone” [6]. This steroid was later isolated and characterized by Simpson and Tait as the mineralocorticoid aldosterone [9]. The ability to observe changes in the activity of salt-active corticosteroids was valuable in elucidating the role of salt-active corticosteroids in a wide variety of clinical conditions: nephrosis, congestive heart failure, essential hypertension, and premenstrual edema. In fact, aldosterone concentration was found to be abnormally high in the urine of nephritic patients with edema and in patients with heart failure or decompensated liver cirrhosis [10].
Conn recognized that increased sodium-retaining steroid activity was not the primary cause but rather a consequence of the pathophysiology of the edematous conditions and classified them as “secondary aldosteronism.” In contrast, he suggested that "primary aldosteronism was not associated with edema and that, in its pure state, it manifests itself as an interesting symptom complex and a fascinating abnormality of electrolyte metabolism" [8].
The index case described by Jerome Conn involved a 34-year-old woman with a 7-year history of intermittent muscle spasms, weakness, and paralysis; increased blood pressure (180 to 190 mm Hg systolic) for 4 years, polyuria and nocturia for many years. The physical examination revealed Chvostek and Trousseau signs, without edema, and blood pressure of 176/104 mmHg. The patient's laboratory values included a low serum potassium of 1.6 to 2.5 mEq/L and an alkaline serum reading of pH 7.62. She had alkaline urine, fixed specific gravity unresponsive to pitresin, and normal 17-hydroxysteroid and 17-ketosteroid values. Conn's diagnosis was that the combination of metabolic alkalosis with hypokalemia and tetany suggested excessive activity of the salt-retaining corticosteroid aldosterone. David HP Streeten, working in Conn's lab at the time, created a bioassay to determine salt-binding corticosteroid activity in urine and found that the activity in the patient's urine was 50 to 100 times greater than that of the normal adults, supporting Conn's presumptive diagnosis [11, 12]. Conn predicted that the prevalence of AP would be between 10 and 20% among hypertensive patients. However, several authors rejected Conn's hypothesis and, until the 1990s, AP was considered a rare disorder, representing less than 1% of all hypertensive patients [13].
Within this framework of ideas, in the clinical case presented, the diagnostic suspicion of a patient with diagnoses of arterial hypertension and refractory hypokalemia is raised, studies were requested that reported aldosterone 47 ng/Dl, with a contrast-enhanced tomography of the abdomen and pelvis where observed in the left adrenal gland an image of nodular appearance, with defined edges, hypodense, measuring 20 x 15mm. Patient is prepared for surgery, exploratory laparoscopy was performed, which revealed a left adrenal gland measuring 8 x 6cm with adenoma in the superficial cortex measuring 3 x 2cm. Left laparoscopic adrenalectomy was performed, a pathological anatomy report was received that reported: benign neoplastic nodular lesion, suggestive of Aldosteronoma. Strict controls of blood pressure figures are maintained where a favorable response is observed, achieving figures of 120/80 mmHg without antihypertensive treatment one year after surgery, obtaining a cure for high blood pressure and refractory hypokalemia through surgical removal of adrenal adenoma. In many cases Conn syndrome is often asymptomatic; When symptoms do occur, they are generally secondary to hypertension or the resulting hypokalemia, such as cramps, easy fatigue, cardiac arrhythmias manifested by palpitations, progressive weakness, even reporting cases of generalized paralysis, polydipsia and polyuria due to diabetes insipidus induced by hypokalemia. In this case it manifested itself with complex ventricular tachycardia complicated with syncope associated with palpitations, diaphoresis, convulsion and worsening to its most lethal form as pulseless polymorphic helical ventricular tachycardia, which required defibrillation and placement of a temporary pacemaker in the patient, fortunately with a response. appropriate [14].
The morbidity and mortality of this syndrome is mostly associated with one of these two conditions. Laparoscopic surgery for unilateral aldosterone hypersecretion is associated with a morbidity of around 8%, with the majority of complications being minor, with no surgical complications occurring. It generally results in normalization of aldosterone secretion and kalaemia, as well as a significant decrease in blood pressure, but normotension without treatment is only achieved in half of the cases. Normotension after adrenalectomy is more common in young patients with recent hypertension than in patients with long-standing hypertension or a family history of hypertension. Strict controls of blood pressure levels were maintained where a favorable response was observed, achieving levels of 120/80 mmHg without antihypertensive treatment, as well as normal potassium values without its restoration 8 months after surgery [15, 16].
Conn Syndrome is a commonly overlooked disease. A timely diagnosis, followed by specific treatment, is important to reduce the risk of cardiovascular complications in affected patients, which is why we affirm that the historical perspective and learning the lessons of the past are essential for medical practice. A clinical case is presented, whose initial clinical suspicion was given in a female patient with arterial hypertension and refractory hypokalemia, whose complementary studies confirm the suspicion, a left laparoscopic transabdominal adrenalectomy was performed and an anatomopathological study reported aldosteronoma. Strict controls of blood pressure and potassium values were maintained, where a favorable response was achieved one year after surgery, obtaining complete cure through surgical removal of the adrenal adenoma.
The authors declare that they have no conflict of interest.
Informed Consent: Informed consent was obtained from all participants included in the study.
Funding: The authors received no specific funding for this work.