AUCTORES
Globalize your Research
case report | DOI: https://doi.org/10.31579/2690-4861/723
1Aravind Eye Hospital and Post-Graduate Institute of Ophthalmology, Coimbatore 641 014, India.
2Sankara Nethralaya, Chennai 600 006, India
*Corresponding Author: Anita Raghavan, Aravind Hospital, Avinashi Road, Peelamedu, Coimbatore.
Citation: Anita Raghavan, Siddharth Narendran, Dhanurekha L, Devi Rosette R, Narendran Venkatapathy, et al, (2025), Concurrent Microsporidial and HSV Keratitis in an Immunocompetent Child, International Journal of Clinical Case Reports and Reviews, 24(2); DOI:10.31579/2690-4861/723
Copyright: © 2025, Anita Raghavan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 28 February 2025 | Accepted: 13 March 2025 | Published: 21 March 2025
Keywords: microsporidia; stromal keratitis; hsv; concurrent; pcr
Purpose: The most common misdiagnosis of microsporidial stromal keratitis is HSV keratitis. We describe the successful diagnosis and resolution of a case of stromal keratitis which was PCR positive for both microsporidia and HSV in an immunocompetent patient.
Observations: Clinically suspected to be stromal microsporidial keratitis, the corneal scrapings were positive for both microsporidia as well as HSV-1. Polyhexamethylene biguanide (PHMB) 0.04%, voriconazole 1%, ganciclovir 0.15% topically combined with oral albendazole were employed to obtain a favorable outcome.
Conclusions: Unresponsive cases of microsporidial keratitis should also be evaluated for HSV, especially given the ubiquitous nature of the latter.
Key Message: Unresponsive cases of microsporidial keratitis should also be evaluated for HSV, especially given the ubiquitous nature of the latter
Introduction
Microsporidial keratitis (MK) is caused by a parasitic spore-forming fungus, belonging to the Phylum Microspora.[1,2] It causes epithelial and stromal keratitis. The Genus Encephalitozoon is usually implicated in the former, while the Genera Nosema or Microsporidium are more likely to cause stromal keratitis. [1-3]
Unlike the acute presentation of epithelial disease, the stromal form evolves slowly, and usually presents as an area of stromal infiltration with edema, is non-suppurative and may be multifocal. It is often recalcitrant to all forms of therapy and usually requires keratoplasty for disease eradication. However, a few individual reports have described successful resolution with medical therapy. The most common misdiagnosis of stromal microsporidial keratitis is viral stromal keratitis, with which it shares certain features – such as a fairly quiet eye, well defined greyish white infiltration, and minimal-to-no anterior chamber reaction.[4] It is important to note that suppurative forms of presentation have also been described which mimic bacterial or fungal keratitis.[4-7]
HSV stromal keratitis is a very common condition which can present with epithelial, stromal or endothelial involvement. The disease, especially the stromal form, can mimic various forms of microbial keratitis. Classically, the stromal form can present with stromal edema and keratic precipitates or as a dense stromal necrosis indistinguishable from other forms of keratitis.[8] One of the most frequent misdiagnosis of stromal microsporidiosis is viral stromal keratitis.
We report the co-occurrence of microsporidial and viral keratitis in an immunocompetent individual, and the strategies employed for successful resolution. To the best of our knowledge this has not been reported before.
A 14-year-old girl presented with defective vision and photophobia of one month’s duration in the Right eye (RE). Her prior therapy included topical steroids, gatifloxacin, ganciclovir, as well as oral valacyclovir. Recorded vision was 6/6 in the affected eye, but with significant blurring. Examination revealed an area of almost full-thickness, central stromal greyish-white, oedematous, non-suppurative infiltration, measuring 4mm x 4mm, with a few keratic precipitates. (Figure 1). The pupil was brisk, the lens clear. Corneal sensation was present but reduced compared to the fellow eye, which was normal in all respects. Clinically, microsporidiosis was suspected. Corneal scrapings were obtained for Gram stain and PCR, the former being positive for microsporidia.
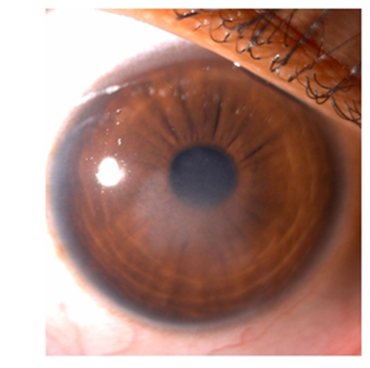
Figure 1: Slit-Lamp biomicroscopy on presentation
Therapy was initiated with polyhexamethylene biguanide (PHMB) 0.04%, voriconazole 1% (8/day), and itraconazole 1% eye ointment. Tablet albendazole 200mg twice a day for 3 weeks was also given. At 4 weeks the lesion remained stationary, and therefore (given the variation in corneal sensation between the 2 eyes), ganciclovir eye ointment 0.15% was added 3 times a day. (Figure 2) After 2 weeks the stromal oedema had reduced (45 days from presentation), with the area of involvement
now measuring 2.4mm into 3mm. Scarring was noted in the temporal aspect of the lesion. Both voriconazole and PHMB were tapered to 6 times. Itraconazole and ganciclovir eye ointments were continued at the same dosage. At 3 months the lesion had almost resolved and medications were gradually tapered over the next 90 days. (Figure 3) PHMB was discontinued after 130 days. Voriconazole in tapering doses, and itraconazole and ganciclovir gel ointments once-a-day, were continued for another 2 months.

Figure 2: Slit-Lamp biomicroscopy after 4 weeks
Figure 3: Slit-Lamp biomicroscopy after 3 months of therapy
The material taken for PCR was processed for both HSV and microsporidia. DNA was amplified by PCR with primers using Primer blast software from NCBI specific for Vittaforma corneae and Encephalitozoon cuniculi targeting the alpha-tubulin gene. The primer
sequence, thermal profile and expected amplicon size used for PCR are given in Table 1. Detection of Herpes simplex virus was performed using the Artus HSV-1/2 RG PCR Kit (Qiagen, Germany) which amplifies the 154bp region of HSV-1 and HSV-2 genomes. The results from the PCRs were positive for Encephalitozoon sp, and Herpes Simplex Virus 1.
| Microsporidia | Sequence (5’-3’) | Thermal profile | Amplicon size | |
| 1. | Vittaforma cornea | FP: ATCAGCGCAGAAGGCATCTC | 94℃- 5mins
58℃ -1 min 30 72℃- 1 min cycles 72℃- 5 mins | 400 bp
|
| RP: CGCACGCTTAGCAAACATCA | ||||
| 2. | Encephalitozoon cuniculi | FP: TGGAGCAGATAAGAAGAATGGC | 94℃- 5mins 94℃ - 1 min 61℃ -1 min 30 72℃- 1 min cycles 72℃- 5 mins | 120bp |
| RP: GCTATCTTTGGTGCCGGATA |
Table 1: Primer sequence, thermal profile, and amplicons for Microsporidia PCR
The most common misdiagnosis of microsporidial keratitis is viral stromal keratitis with which it shares several clinical features. The first paper that suggested a possible co-existent infection with both microsporidia and HSV was by Mittal et al in their retrospective analysis of 263 excised corneal buttons.[5] They noted that 7 of these buttons were positive for microsporidia, both on histopathological examination as well as by PCR. Of note, the authors found 42% of these cases to have a granulomatous response with intense polymorphonuclear infiltration and stromal necrosis. Interestingly, these cases were also positive for HSV on PCR. The authors therefore postulated that patients with severe microsporidial keratitis should also be investigated for HSV-1 as this may impact outcomes. However, our case did not have any signs of suppuration or thinning indicative of the potential presence of HSV. One other consideration was the possibility of immune stromal keratitis due to MS (as suggested by Mohanty et al [9]), but at no point were steroids administered to promote resolution; it is therefore presumed in our case that both the parasitic and viral disease were active infections.
The medical management of stromal microsporidiosis is difficult and penetrating keratoplasty is considered the definitive therapeutic option. Sabhapandit in their series of 34 cases reported that 73% of their cases failed medical therapy with topical PHMB and chlorhexidine, with or without oral albendazole, and required keratoplasty for disease eradication.[10] However, a few individual cases have had successful outcomes. Donovan reported successful resolution with oral albendazole and topical voriconazole administered over 4 weeks [11] whereas, Coca et al reported successful resolution with topical voriconazole and oral itraconazole administered over 8 weeks. [12] Raghavan et al have reported successful resolution of stromal MS with PHMB/ chlorhexidine, fluconazole, and oral albendazole [13] Past medical treatments for microsporidial stromal keratitis have included topical chloramphenicol, fumagillin, oral albendazole or itraconazole, thiabendazole, propamidine isethionate, chlorhexidine, metronidazole, PHMB, and benzimidazole.[7,10,12]
Our case resolved successfully with a combination of antiparasitic and antiviral therapy. Significantly, the stromal oedema resolved only with addition of topical antivirals. Given the fact that stromal microsporidiosis has several features in common with viral stromal keratitis, misdiagnoses are frequent. It should also be noted that, when steroids are given in viral stromal keratitis, this could have a deleterious effect if there is an underlying microsporidial infection.[14]
Stromal microsporidiosis is generally considered to be a difficult to treat condition and very often requires keratoplasty for eradication. We report the successful resolution of a case of concurrent keratitis caused by microsporidia and HSV-1 in an immunocompetent child, facilitated by early recognition and institution of appropriate anti-parasitic as well as anti-viral therapy. The implicated microsporidia belonged to the genus Encephalitozoon – which is rarely associated with stromal microsporidiosis. Voriconazole and PHMB appear to be effective in treating stromal microsporidosis; however, the duration and the dosage needs further clarification. It is possible that some treatment failures of either stromal microsporidosis or viral stromal keratitis could be due to the failure to recognise the presence of an additional organism. In unresponsive or poorly responding cases, this consideration, as well as molecular diagnostics could prove valuable.